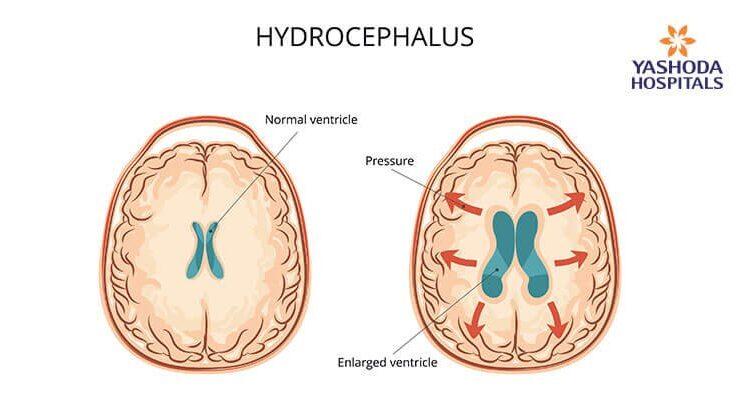
Hydrocephalus Symptoms: Hydrocephalus, often referred to as “water on the brain,” is a serious condition where an abnormal accumulation of cerebrospinal fluid (CSF) occurs within the brain’s ventricles.
This accumulation can lead to increased intracranial pressure, potentially causing damage to brain tissues and impairing brain functions.
Understanding the symptoms and causes of hydrocephalus is crucial for early detection and effective management.
What is Hydrocephalus?
Hydrocephalus is a medical condition characterized by an abnormal accumulation of cerebrospinal fluid (CSF) within the brain’s ventricles. This buildup can increase pressure inside the skull, potentially leading to brain damage and other serious complications. The term “hydrocephalus” is derived from Greek, where “hydro” means water and “cephalus” means head, literally translating to “water on the brain.”
Overview of the Condition
Hydrocephalus can affect individuals of any age but is most commonly seen in infants and older adults. The condition can be congenital (present at birth) or acquired due to factors such as head injuries, infections, tumors, or bleeding in the brain. Symptoms can vary depending on age and severity but often include headaches, nausea, balance problems, vision disturbances, and cognitive impairments.
Early diagnosis and treatment are crucial to managing hydrocephalus effectively. Treatments typically involve surgical procedures to divert the excess fluid to other parts of the body where it can be absorbed, often using a device called a shunt.
Types of Hydrocephalus
Hydrocephalus is generally classified into several types:
- Congenital Hydrocephalus: Present at birth, this type is often caused by genetic abnormalities or developmental disorders such as spina bifida.
- Acquired Hydrocephalus: Occurs after birth and can result from injury, infections like meningitis, tumors, or hemorrhage.
- Communicating Hydrocephalus: This type occurs when CSF flows freely through the brain’s ventricles but is blocked after leaving the ventricles, leading to fluid buildup.
- Non-communicating Hydrocephalus: Also known as obstructive hydrocephalus, this type is characterized by a blockage within the ventricular system, preventing CSF from flowing properly.
- Normal Pressure Hydrocephalus (NPH): Common in older adults, NPH is marked by enlarged ventricles and normal CSF pressure, often leading to symptoms like walking difficulties, dementia, and urinary incontinence.
However, understanding the different types of hydrocephalus is essential for appropriate diagnosis and treatment, ensuring better outcomes and quality of life for those affected.
Common Symptoms of Hydrocephalus
Recognizing these symptoms early is crucial for effective treatment. Below, we detail the common symptoms of hydrocephalus in both infants and older individuals.
Symptoms in Infants
Infants with hydrocephalus often exhibit distinct symptoms due to their developing skulls and brains. Parents and caregivers should be vigilant for the following signs:
- Enlarged Head Size: A rapidly increasing head circumference is a key indicator. The head may appear disproportionately large compared to the body.
- Bulging Fontanel: The soft spot on top of a baby’s head, known as the fontanel, may appear tense or bulging due to increased intracranial pressure.
- Vomiting: Frequent vomiting without an obvious cause can be a sign of hydrocephalus, as the increased pressure affects the brain’s control of nausea.
- Irritability: Excessive fussiness or inconsolable crying can be a result of the discomfort caused by elevated intracranial pressure.
- Poor Feeding: Difficulty in feeding or poor appetite may be observed, potentially leading to inadequate weight gain.
Symptoms in Older Children and Adults
In older children and adults, the symptoms of hydrocephalus can be more varied and may affect physical, cognitive, and visual functions. Key symptoms include:
- Headache: Persistent or severe headaches, often described as worse in the morning or after lying down, are common.
- Nausea: Similar to infants, nausea and vomiting can occur, sometimes alongside headaches.
- Balance Problems: Difficulty in maintaining balance, walking, or frequent stumbling can indicate hydrocephalus.
- Blurred or Double Vision: Visual disturbances, such as blurred or double vision, can result from increased pressure on the optic nerves.
- Cognitive Challenges: Issues with memory, concentration, and reasoning abilities may arise, affecting daily activities and learning.
- Difficulty Walking: Problems with coordination and gait, leading to an unsteady walk or frequent falls, are often noted in those with hydrocephalus.
If you or a loved one exhibit these symptoms, seeking medical advice promptly is essential.
Causes of Hydrocephalus
Understanding these causes is crucial for early detection and treatment. The causes of hydrocephalus can be broadly categorized into congenital and acquired.
Congenital Causes
1. Genetic Factors:
Some cases of hydrocephalus are linked to genetic abnormalities. These genetic mutations can disrupt the normal flow and absorption of cerebrospinal fluid (CSF), leading to an accumulation within the brain.
2. Developmental Disorders:
Developmental disorders, such as spina bifida or Dandy-Walker malformation, are significant contributors to congenital hydrocephalus. These conditions affect the brain’s structure, impeding the proper circulation of CSF.
Acquired Causes
1. Infections:
Infections such as meningitis can lead to hydrocephalus. Meningitis causes inflammation of the brain and spinal cord membranes, which can obstruct the flow of CSF, resulting in its buildup.
2. Head Injuries:
Traumatic brain injuries can damage brain tissues and blood vessels, leading to an obstruction in the CSF pathways. This obstruction can cause hydrocephalus to develop over time.
3. Brain Tumors:
Tumors in the brain can block the flow of CSF, causing it to accumulate. The pressure from the excess fluid can lead to hydrocephalus, adding to the complications of the primary tumor.
4. Bleeding in the Brain:
Intracranial hemorrhage, or bleeding within the brain, can also cause hydrocephalus. Blood from the hemorrhage can block the CSF pathways, preventing the fluid from draining properly.
By understanding these causes, healthcare providers can better diagnose and treat hydrocephalus, potentially mitigating its impact on patients’ lives.
Diagnosis of Hydrocephalus
Understanding the various methods used for diagnosing hydrocephalus, along with recognizing the importance of early detection, is crucial for patients, caregivers, and healthcare providers.
Methods of Diagnosing Hydrocephalus
The diagnosis of hydrocephalus involves a combination of clinical assessment and imaging techniques to accurately assess the presence and extent of fluid accumulation in the brain. Here are the most commonly used diagnostic methods:
- Neurological Examination: A thorough neurological exam by a healthcare provider can help identify signs of hydrocephalus. Symptoms such as changes in vision, difficulty with balance, poor coordination, and delayed developmental milestones in infants often prompt further investigation.
- Ultrasound: For infants, an ultrasound through the soft spots on the skull (fontanels) can be a quick and non-invasive method to detect hydrocephalus. This method is particularly useful for newborns and young infants whose skull bones have not yet fully fused.
- Magnetic Resonance Imaging (MRI): MRI is a highly detailed imaging technique that provides clear images of the brain, making it effective in identifying the enlargement of ventricles caused by excess CSF. It also helps in assessing the underlying causes and the exact locations of fluid accumulation.
- Computed Tomography (CT) Scan: A CT scan is a faster imaging method that can also show the presence of hydrocephalus. It is particularly useful in emergency situations where quick assessment is crucial.
- Intracranial Pressure Monitoring: In some cases, measuring the pressure inside the head is necessary, especially if symptoms are severe or worsening. This method involves the insertion of a device into the skull to measure ongoing pressure levels.
Importance of Early Diagnosis
Early diagnosis of hydrocephalus is vital for several reasons:
- Preventing Progressive Symptoms: Early detection and treatment can prevent the progression of symptoms and potential permanent brain damage. It can significantly improve the quality of life for the affected individual.
- Improving Treatment Outcomes: The earlier hydrocephalus is diagnosed, the more effective the treatment can be. Surgical options such as shunt systems or endoscopic third ventriculostomy (ETV) can be implemented more successfully if the condition is caught early.
- Reducing Complications: Timely intervention can reduce the risk of complications associated with advanced hydrocephalus, including intellectual impairment and physical disabilities.
If hydrocephalus is suspected, it is imperative to consult healthcare professionals who can initiate the diagnostic process and recommend the best course of treatment.
Treatment Options for Hydrocephalus
Effective management is crucial to alleviate symptoms and prevent long-term complications. This article outlines the surgical treatments, non-surgical treatments, and long-term management strategies for hydrocephalus.
Surgical Treatments for Hydrocephalus
- Shunt System Insertion: The most common surgical treatment for hydrocephalus is the insertion of a shunt system. This involves placing a flexible tube in one of the brain’s ventricles to divert excess fluid to another part of the body, such as the abdominal cavity, where it can be absorbed. Shunts can be programmable or non-programmable, allowing for adjustable fluid drainage depending on the patient’s needs.
- Endoscopic Third Ventriculostomy (ETV): This surgical procedure involves creating a hole in the floor of the third ventricle to allow fluid to bypass the obstruction and flow towards the areas where it can be naturally absorbed. ETV is often preferred for patients with non-communicating hydrocephalus as it eliminates the need for implanting a device.
- Choroid Plexus Cauterization: Sometimes combined with ETV, this procedure involves cauterizing the choroid plexus, a part of the brain that produces cerebrospinal fluid, to reduce fluid production.
Non-Surgical Treatments for Hydrocephalus
While surgery is the most common treatment for hydrocephalus, there are non-surgical options that may be considered, particularly in mild cases or when surgery poses too high a risk:
- Medication: Though not a cure, medications such as acetazolamide and furosemide can help reduce the production of CSF and alleviate symptoms in some patients.
- Lumbar Puncture: In some emergency situations, a lumbar puncture may be performed to remove excess CSF and relieve pressure. However, this is a temporary solution and not used for long-term management.
- Observation: In cases where the condition is stable and not causing significant symptoms, close monitoring with regular check-ups and brain imaging may be the only treatment necessary.
Long-term Management and Follow-Up
Long-term management of hydrocephalus is essential to monitor the effectiveness of the treatment and detect any changes in the condition. Follow-up typically involves:
- Regular Medical Reviews: Patients will need regular check-ups to assess neurological health and the functioning of any implanted devices.
- Neuroimaging Tests: MRI or CT scans are frequently used to monitor the brain’s ventricles and the effectiveness of the treatment strategy.
- Lifestyle Adjustments: Patients may be advised to make lifestyle changes to manage symptoms better and improve overall health, such as engaging in gentle exercise, maintaining a balanced diet, and avoiding activities that increase intracranial pressure.
- Support Services: Access to educational resources, psychological support, and community services can help patients and families cope with the challenges of living with hydrocephalus.
However, regular communication with healthcare providers and adherence to treatment plans are crucial to successfully managing this chronic condition.
Living with Hydrocephalus
Living with hydrocephalus can be challenging for both patients and their families. Understanding how to manage the condition effectively, accessing robust support networks, and adopting practical coping strategies are essential for maintaining a good quality of life. Here, we provide a comprehensive guide to navigating the complexities of hydrocephalus.
Coping Strategies for Patients and Families
- Educate Yourself and Family: Knowledge is power. Understanding hydrocephalus and its potential impact on health and lifestyle helps in managing expectations and preparing for challenges.
- Regular Medical Check-ups: Consistent monitoring of the condition by healthcare professionals helps in early detection of complications and adjustments in treatment plans.
- Mental Health Support: It’s important for patients and family members to seek mental health support to cope with emotional and psychological stress. Therapy, counseling, and support groups can be very beneficial.
- Adaptive Tools and Technology: Use tools and technology designed to assist those with physical limitations. Items like programmable shunts, mobility aids, and home modifications can help in managing symptoms and improving quality of life.
- Establish a Routine: A structured daily routine can help in reducing uncertainty and stress for both patients and caregivers, making daily life more manageable.
- Community Engagement: Staying engaged with community activities can provide social support and reduce feelings of isolation.
Support Groups and Resources
- Local and Online Support Groups: Many organizations offer support groups for individuals with hydrocephalus and their families, providing a platform to share experiences and advice.
- Educational Resources: Websites of organizations such as the Hydrocephalus Association offer educational materials, updates on research, treatment options, and ways to connect with specialists.
- Financial Assistance Programs: Look for financial aid available through healthcare institutions and public service bodies to help manage the cost of ongoing treatment and equipment.
- Professional Networks: Building a network of healthcare providers familiar with hydrocephalus, including neurologists, therapists, and counselors, ensures comprehensive care.
Managing Daily Life and Potential Complications
- Symptom Management: Stay vigilant about symptoms like headaches, nausea, or changes in vision, which could indicate shunt malfunctions or other complications.
- Emergency Preparedness: Keep emergency contact numbers handy and ensure all family members know what to do in case of a sudden complication.
- Lifestyle Adjustments: Dietary modifications, physical therapy, and regular exercise adapted to the patient’s capabilities can help in managing symptoms and improving overall health.
- Education and Employment: Seek accommodations in educational and work environments to suit the individual needs of those with hydrocephalus, ensuring they have access to opportunities for personal and professional growth.
- Regular Updates With Healthcare Providers: Keeping in constant communication with healthcare professionals helps in promptly addressing any changes in the condition and adapting treatment plans accordingly.
By embracing these strategies, patients with hydrocephalus and their families can lead more controlled and fulfilling lives. Additionally, leveraging the support and resources available can greatly assist in navigating the challenges posed by the condition.
FAQs about Hydrocephalus Symptoms
1. What are the common symptoms of hydrocephalus in infants?
In infants, common symptoms of hydrocephalus include an unusually large head, a rapid increase in head size, a bulging soft spot on the top of the head, vomiting, sleepiness, irritability, and poor feeding.
2. How do hydrocephalus symptoms manifest in older children and adults?
Older children and adults may experience different symptoms such as headaches, blurred or double vision, difficulty with balance, poor coordination, gait disturbances, urinary incontinence, and cognitive challenges such as memory loss.
3. Can hydrocephalus cause changes in personality or behavior?
Yes, hydrocephalus can lead to changes in personality and behavior. Individuals might exhibit increased irritability, mood swings, or a change in personality traits. In some cases, there can also be a noticeable decline in school or work performance.
4. Are hydrocephalus symptoms consistent in everyone?
No, symptoms can vary widely among individuals depending on the severity of the condition, the areas of the brain affected, and the person’s age. Early detection and treatment are crucial for managing symptoms effectively.
5. What should I do if I suspect someone has hydrocephalus?
If you suspect hydrocephalus, it is important to seek medical attention immediately. A healthcare professional can perform a physical exam and may recommend imaging tests such as an ultrasound, MRI, or CT scan to diagnose the condition accurately.
6. Are there emergency symptoms of hydrocephalus that require immediate medical attention?
Yes, some symptoms require immediate medical attention, such as sudden intense headaches, vomiting, a significant change in consciousness or alertness, muscle weakness, or sudden problems with vision. These could indicate a worsening condition that needs urgent care.
7. Can the symptoms of hydrocephalus be treated or managed?
Yes, the symptoms of hydrocephalus can often be managed with surgical interventions such as the insertion of a shunt system to drain excess cerebrospinal fluid. Medications and rehabilitation therapies can also help manage symptoms and improve quality of life.
Conclusion
In summary, understanding the symptoms of hydrocephalus is crucial for early diagnosis and effective management. This condition, characterized by an accumulation of fluid in the brain, manifests through various signs such as headaches, nausea, blurred vision, and difficulties with balance. Recognizing these symptoms early can significantly improve the outcome for individuals affected.
It is essential not to overlook these indicators, as timely medical intervention can prevent complications and enhance quality of life. If you or someone you know exhibits symptoms of hydrocephalus, it is imperative to consult a healthcare professional immediately. Seeking expert advice at the earliest ensures appropriate evaluation and the initiation of necessary treatments, paving the way for better health management. Remember, early recognition and action are key in addressing the challenges of hydrocephalus effectively.
References
For those seeking more detailed information and further validation of the topics covered in our discussion on hydrocephalus symptoms, the following references are invaluable. Each source is reputable and provides deeper insights into the condition, offering readers additional resources for education and understanding:
- National Institute of Neurological Disorders and Stroke (NINDS) – NINDS offers a comprehensive overview of hydrocephalus, including symptoms, treatment options, and ongoing research. Read more about hydrocephalus on the NINDS website.
- Mayo Clinic – The Mayo Clinic provides a detailed description of hydrocephalus symptoms, causes, and diagnostic procedures. Their resources are helpful for patients and caregivers alike. Explore hydrocephalus resources at the Mayo Clinic.
- MedlinePlus – A service of the U.S. National Library of Medicine, MedlinePlus offers accessible health information on hydrocephalus, including a medical encyclopedia and links to latest treatments and studies. Visit MedlinePlus for more information on hydrocephalus.
These sources are recommended for their authoritative information and user-friendly presentation, making them excellent starting points for individuals looking to expand their knowledge on hydrocephalus.