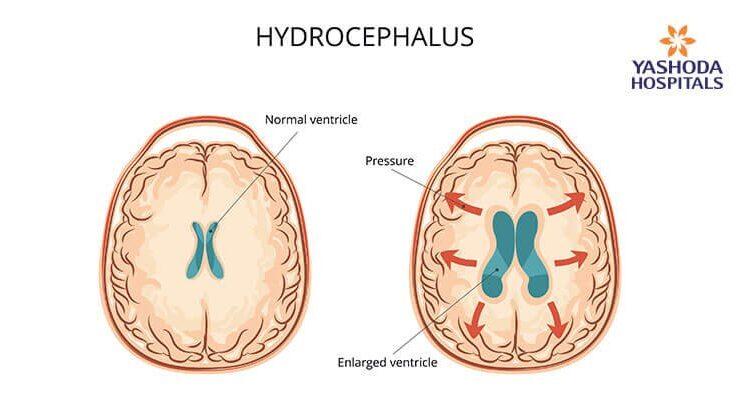
Hydrocephalus Treatment: Hydrocephalus is a medical condition characterized by an abnormal accumulation of cerebrospinal fluid (CSF) within the ventricles, or cavities, of the brain.
This can lead to increased intracranial pressure inside the skull, which can cause swelling of the brain, potentially damaging it.
Understanding the diagnosis and treatment options for hydrocephalus is crucial for managing this complex condition effectively.
Understanding Hydrocephalus
Hydrocephalus is a medical condition characterized by an excessive accumulation of cerebrospinal fluid (CSF) in the brain. This build-up occurs in the ventricles, or cavities, within the brain, potentially leading to increased intracranial pressure. This abnormal pressure can damage brain tissues and impair brain function. Understanding the types, causes, risk factors, and symptoms of hydrocephalus is crucial for early diagnosis and management.
Types of Hydrocephalus
Hydrocephalus can be classified into several types based on its origin, underlying mechanisms, and the time of onset:
- Congenital Hydrocephalus: Present at birth, this type results from genetic predispositions or developmental disorders like spina bifida.
- Acquired Hydrocephalus: This form develops after birth due to conditions such as brain tumors, head injuries, or infections.
- Communicating Hydrocephalus: In this type, CSF can still flow between the ventricles, which are not blocked but the absorption into the bloodstream is impaired.
- Non-communicating Hydrocephalus: Also known as obstructive hydrocephalus, this occurs when the flow of CSF is blocked along one or more of the narrow passages connecting the ventricles.
- Normal Pressure Hydrocephalus (NPH): Occurring in older adults, NPH is characterized by ventricle enlargement without a corresponding increase in CSF pressure.
Causes and Risk Factors
The causes of hydrocephalus can vary based on the type, but some common factors include:
- Genetic mutations leading to structural defects in the brain.
- Developmental disorders, such as those that affect the brain and spinal cord during fetal development.
- Infections that affect the brain, such as meningitis or encephalitis.
- Brain tumors or lesions that block the flow of CSF.
- Injuries to the brain that result in bleeding or blockage of CSF pathways.
Risk factors enhance the likelihood of developing hydrocephalus and may include premature birth, a history of neural tube defects, or a family history of the condition.
Symptoms Across Different Age Groups
The symptoms of hydrocephalus can vary significantly between infants, children, and adults due to differences in skull rigidity and other physiological factors.
- Infants: Symptoms in infants include an unusually large head, a rapid increase in head size, a bulging fontanel (soft spot on the top of the head), vomiting, sleepiness, irritability, and seizures.
- Children: In older children, symptoms might involve headache, double vision, poor coordination, ataxia (a lack of muscle control), and difficulties with balance and walking.
- Adults: Adults, especially the elderly, might exhibit symptoms of NPH, which include memory loss, difficulty walking, and impaired bladder control, often mistaken for aging or dementia-related disorders.
However, early diagnosis and treatment improve the outlook for those with hydrocephalus, minimizing potential long-term impacts on brain function and overall health.
Diagnosis of Hydrocephalus
Detecting hydrocephalus early is crucial for effective management and treatment. Understanding the initial signs and the diagnostic procedures involved can help in seeking timely medical attention.
Initial Signs That Warrant Medical Attention
Hydrocephalus can manifest through various symptoms that should prompt immediate medical consultation. In infants, signs include an unusually large head, a rapid increase in head size, or a bulging soft spot (fontanel) on the top of the head. Older children and adults might experience headaches, blurred or double vision, difficulty with balance, poor coordination, and cognitive challenges. Any of these symptoms warrant a consultation with a healthcare provider to rule out hydrocephalus or other medical conditions.
Diagnostic Tests and Procedures
Once hydrocephalus is suspected based on initial symptoms, several diagnostic tests and procedures are typically employed to confirm the diagnosis:
1. Neurological Examinations: A basic neurological exam will assess motor and sensory skills, presence of reflexes, and cognitive function. This can help determine the impact of potential fluid accumulation on brain function.
2. Imaging Tests:
- Ultrasound: For infants, an ultrasound through the open fontanel provides a non-invasive look at the brain. It can help detect enlarged ventricles caused by fluid accumulation.
- MRI (Magnetic Resonance Imaging): MRI provides a detailed image of the brain. It can show the flow of cerebrospinal fluid (CSF) and reveal whether the fluid pathways are blocked.
- CT Scan (Computed Tomography): A CT scan can quickly provide images to detect or rule out hydrocephalus. It is often used in emergency situations when rapid diagnosis is necessary.
3. Intracranial Pressure Monitoring: In some cases, doctors might measure the pressure inside the head to determine if the increase in cerebrospinal fluid is causing high intracranial pressure, which is indicative of hydrocephalus.
The Role of Early Diagnosis in Effective Management
Early diagnosis plays a pivotal role in the effective management of hydrocephalus. Timely identification of the condition allows for earlier intervention, which can significantly improve the prognosis. Interventions might include surgical procedures such as the insertion of a shunt system to divert fluid away from the brain to another part of the body where it can be absorbed, or endoscopic third ventriculostomy, which creates a new pathway for cerebrospinal fluid flow.
Managing hydrocephalus effectively with early diagnosis can prevent the progression of symptoms and lead to better developmental, cognitive, and physical outcomes, especially in children. It also minimizes the potential long-term impact on quality of life for patients of all ages.
Treatment Options for Hydrocephalus
Effective management of hydrocephalus is crucial, and treatment typically involves both surgical and non-surgical approaches, depending on the severity and underlying cause of the condition.
Surgical Treatments
Surgical intervention is the most common treatment for hydrocephalus, aiming to relieve pressure in the brain by draining the excess CSF. The following are the primary surgical options:
- Shunt System: This is the most prevalent surgical treatment, where a shunt (a flexible tube) is inserted into the ventricle to divert the flow of CSF away from the brain and towards another area of the body, such as the abdominal cavity, where it can be absorbed. Shunts can be programmable or non-programmable, depending on the needs of the patient.
- Endoscopic Third Ventriculostomy (ETV): Suitable for obstructive (non-communicating) hydrocephalus, ETV involves making a hole in the floor of the third ventricle using an endoscope, which allows CSF to bypass the obstruction and flow towards the reabsorption sites. This procedure is often preferred over shunt placement because it eliminates the need for a foreign object in the body and has a lower risk of infection.
- Ventriculoperitoneal Shunt (VP Shunt): This specific type of shunt system helps to manage CSF flow by connecting the ventricles of the brain to the peritoneal cavity.
Each surgical option carries risks, including infection, shunt malfunction, and the need for further surgeries. Therefore, the decision to proceed with surgery is made after careful evaluation of the individual patient’s condition and overall health.
Non-Surgical Management
In some cases, particularly where surgery is not immediately necessary or in very mild cases, non-surgical management may be appropriate. Non-surgical options include:
- Medication: Though not a cure, medications can be used to help reduce the production of CSF temporarily. Drugs such as acetazolamide and furosemide are sometimes prescribed to decrease fluid production.
- Observation: In cases where hydrocephalus is stable and not causing significant symptoms, regular monitoring through neurological assessments and imaging studies might be the only intervention.
- Lifestyle Adjustments: Adjusting daily activities to avoid excessive strain or trauma to the head can help manage symptoms. Additionally, physical therapy and occupational therapy might be recommended to address developmental delays or physical symptoms in children.
However, regular follow-ups with healthcare providers are essential to monitor the condition and adjust treatment plans as necessary. Early diagnosis and timely intervention are critical to managing hydrocephalus effectively and minimizing potential complications.
Managing Life with Hydrocephalus
Living with hydrocephalus, a condition characterized by an accumulation of cerebrospinal fluid in the brain, presents numerous challenges. Understanding its impact on quality of life, along with implementing effective long-term management strategies, is crucial for patients and their caregivers. Additionally, tapping into robust support systems and resources can significantly ease the journey. Below, we delve into these critical aspects to provide a comprehensive guide for managing life with hydrocephalus.
Impact of Hydrocephalus on Quality of Life
Hydrocephalus can significantly affect a person’s daily activities and overall well-being. Here are some common ways in which the condition impacts quality of life:
- Physical Limitations: Mobility might be affected due to balance and coordination problems. Physical symptoms like headaches and fatigue can also limit activity levels.
- Cognitive Effects: Learning disabilities, memory problems, and difficulties in problem-solving are often observed, affecting educational and occupational opportunities.
- Emotional and Social Impact: The physical and cognitive challenges can lead to social isolation and emotional issues such as anxiety and depression.
- Healthcare Burdens: Frequent medical appointments, potential surgeries, and ongoing therapy can be stressful and time-consuming for both patients and their families.
Long-Term Management Strategies
Effectively managing hydrocephalus involves a combination of medical treatment and lifestyle adaptations. Here are key strategies for long-term management:
- Regular Medical Check-ups: Routine monitoring by healthcare professionals helps manage symptoms and prevent complications.
- Surgical Interventions: Shunt systems or endoscopic third ventriculostomy (ETV) may be necessary to manage fluid levels in the brain.
- Rehabilitation Therapies: Physical, occupational, and speech therapies can help improve mobility, daily function, and communication skills.
- Educational and Vocational Counseling: Tailored educational programs and career guidance accommodate learning disabilities and help integrate patients into society.
- Lifestyle Modifications: Diet, exercise, and relaxation techniques can help manage symptoms and improve overall health.
Support Systems and Resources for Patients and Caregivers
Navigating hydrocephalus is a shared journey, and numerous support systems are available:
- Patient Networks and Support Groups: These provide a platform for sharing experiences and advice, reducing feelings of isolation.
- Educational Resources: Books, websites, and seminars help patients and caregivers understand the condition and keep up-to-date with the latest treatment options.
- Community Services and Assistance Programs: Local health services may offer assistance with transportation, home care, and medical costs.
- Counseling and Mental Health Support: Professional counseling can help patients and families cope with the emotional challenges of hydrocephalus.
- Advocacy and Awareness Organizations: Groups like the Hydrocephalus Association offer resources, advocate for patient rights, and fund research into better treatments.
Embracing a comprehensive management plan, utilizing available resources, and building a support network are vital for those affected by hydrocephalus to lead fulfilling lives. By focusing on these elements, patients and caregivers can navigate the complexities of the condition more effectively.
Advances in Hydrocephalus Treatment
Hydrocephalus, a condition characterized by an accumulation of cerebrospinal fluid in the brain, has seen significant advancements in treatment methods, improving outcomes for patients worldwide. Recent research has catalyzed the development of innovative treatment approaches and surgical techniques, enhancing both safety and effectiveness.
Recent Research and Developments in Treatment Methods
In the realm of hydrocephalus treatment, recent years have showcased groundbreaking research focusing on both medicinal and surgical solutions. Pharmacological research is exploring drugs that can reduce cerebrospinal fluid production or increase its absorption, offering potential non-invasive treatment options. These developments could revolutionize how we manage this condition, particularly for patients who are less suited for surgery.
Innovations in Surgical Techniques and Technology
Surgical intervention remains the cornerstone of hydrocephalus management, with innovations significantly improving patient outcomes. The advent of neuroendoscopic techniques allows for minimally invasive procedures to treat hydrocephalus. These methods, such as endoscopic third ventriculostomy (ETV), provide alternatives to traditional shunt systems, reducing the risks associated with shunt dependency and complications like infections and blockages. Moreover, advancements in imaging technologies have improved surgical accuracy, making procedures safer and more efficient.
Future Directions in Hydrocephalus Management
Looking ahead, the future of hydrocephalus management is promising, with several research directions poised to further transform treatment paradigms. The integration of advanced biotechnologies, including stem cell therapy and regenerative medicine, holds the potential to repair or replace damaged brain tissue caused by hydrocephalus. Additionally, the development of smarter, more adaptive shunt systems that can dynamically adjust to the changing needs of the patient’s cerebrospinal fluid dynamics is on the horizon. These innovations not only aim to enhance the quality of life for those affected but also reduce long-term healthcare costs by minimizing complications and the need for multiple surgeries.
These advances in hydrocephalus treatment underscore a rapidly evolving field where research, innovation, and technology converge to offer new hope and improved care for patients suffering from this challenging condition.
FAQs about Hydrocephalus Treatment
What is hydrocephalus?
Hydrocephalus is a medical condition characterized by an abnormal buildup of cerebrospinal fluid (CSF) in the ventricles, or cavities, of the brain. This excess fluid can increase pressure inside the skull, potentially causing damage to brain tissues and impairing brain function.
How is hydrocephalus treated?
Treatment for hydrocephalus typically involves surgical intervention to help drain the excess fluid. The most common procedure is the insertion of a device called a shunt. This device diverts the flow of CSF from the brain to another part of the body, where it can be absorbed into the bloodstream. Another less common treatment is endoscopic third ventriculostomy (ETV), which involves creating a hole to allow fluid to flow more freely within the brain’s ventricular system.
Are there different types of shunts?
Yes, there are several types of shunts used to treat hydrocephalus, including ventriculoperitoneal (VP) shunts, ventriculoatrial (VA) shunts, and lumboperitoneal (LP) shunts. The type of shunt used typically depends on the patient’s specific needs and the underlying cause of the hydrocephalus.
What are the risks of hydrocephalus surgery?
While shunt surgery is generally safe, there are potential risks and complications, including infection, shunt malfunction, and the need for additional surgeries. Regular follow-ups with healthcare providers are necessary to monitor the function of the shunt and overall brain health.
Can hydrocephalus be cured?
Hydrocephalus is generally a chronic condition, and while surgical treatments can manage symptoms and divert CSF, they do not cure the underlying condition. Ongoing medical care and monitoring are crucial for managing hydrocephalus effectively over time.
How can I support someone with hydrocephalus?
Supporting someone with hydrocephalus involves providing emotional and practical assistance, understanding their symptoms and treatment plan, and helping them keep up with medical appointments. Additionally, joining a support group or connecting with community resources can be beneficial for both patients and caregivers.
Conclusion
In conclusion, understanding and recognizing the symptoms of hydrocephalus is crucial for timely diagnosis and treatment. Early detection plays a pivotal role in managing this condition effectively, potentially preventing complications and improving the quality of life for those affected.
We encourage individuals experiencing symptoms or those caring for someone who might be at risk to consult healthcare providers without delay. Ongoing care and regular consultations with medical professionals are essential to monitor the condition and adapt treatment plans as needed.
Stay proactive about your health and maintain open communication with your medical team to navigate the challenges of hydrocephalus with confidence.
References
For those seeking to deepen their understanding of hydrocephalus treatment options and validate the information discussed, the following references are invaluable resources. Each source is recognized for its credibility and depth of information in the field of neurology and hydrocephalus management:
- Mayo Clinic – Hydrocephalus Treatment Overview: This comprehensive guide by the Mayo Clinic offers an extensive overview of treatments, procedures, and care options for hydrocephalus. It’s an essential resource for patients and healthcare providers alike. Read more about Hydrocephalus treatments at Mayo Clinic.
- National Institute of Neurological Disorders and Stroke – Hydrocephalus Fact Sheet: This fact sheet provides detailed information on the symptoms, causes, and various treatment methods available for hydrocephalus, including surgical and non-surgical approaches. Visit the NINDS page on Hydrocephalus.
- Johns Hopkins Medicine – Hydrocephalus: Johns Hopkins is a leader in medical research and treatment. Their section on hydrocephalus includes articles on innovation in treatment techniques and patient care tips. Explore Johns Hopkins Medicine’s insights on Hydrocephalus.
- Hydrocephalus Association – Resources for Patients and Families: This organization provides a wealth of resources, including treatment options, research updates, and community support for individuals and families affected by hydrocephalus. Learn more from the Hydrocephalus Association.
These resources are recommended for anyone looking to obtain reliable and up-to-date information on hydrocephalus and its treatment options.