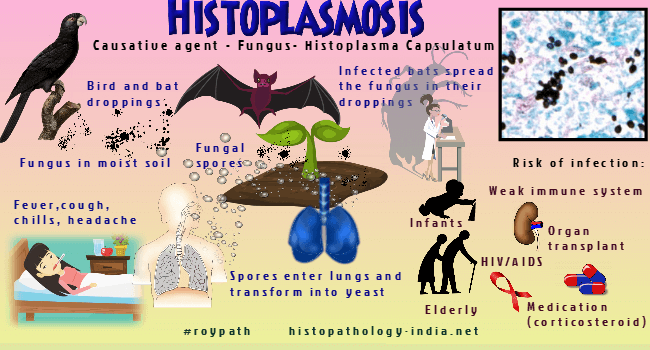
Histoplasmosis Symptoms: Histoplasmosis is a fungal infection primarily caused by the fungus Histoplasma capsulatum.
This disease can affect both humans and animals, particularly when they inhale the fungal spores from the environment.
Typically found in soil contaminated with bird or bat droppings, this infection is more common in certain regions, especially in river valleys and areas with significant bird populations.
What is Histoplasmosis?
Histoplasmosis is a fungal infection caused by inhaling spores of the fungus Histoplasma capsulatum. This infection primarily affects the lungs, but it can also spread to other parts of the body, especially in individuals with weakened immune systems. While many people infected with Histoplasma spores may not show symptoms, others can experience flu-like symptoms, respiratory issues, and in severe cases, chronic lung disease or disseminated histoplasmosis, which can be life-threatening.
How the Infection Spreads
Histoplasmosis is contracted through the inhalation of Histoplasma spores, which are often found in environments where bird or bat droppings are present. Common sources and methods of infection include:
- Soil Disturbance: Activities that disturb soil, such as construction, farming, or gardening, can release fungal spores into the air.
- Bird and Bat Droppings: Areas with a high concentration of bird or bat droppings, such as caves, chicken coops, and old buildings, are common sources of Histoplasma spores.
- Outdoor Activities: Activities like spelunking (cave exploration) and cleaning chicken coops or other areas with droppings can increase the risk of inhaling spores.
Populations Most at Risk
While histoplasmosis can affect anyone, certain populations are at higher risk, including:
- Individuals with Weakened Immune Systems: People with HIV/AIDS, those undergoing chemotherapy, or individuals on immunosuppressive medications are more susceptible to severe forms of the infection.
- Infants and Elderly: Both infants and the elderly have weaker immune systems, making them more vulnerable to histoplasmosis.
- Workers in High-Risk Occupations: Farmers, construction workers, pest control workers, and others who frequently disturb soil or come into contact with bird or bat droppings are at an increased risk.
- Travelers to Endemic Areas: People visiting areas where histoplasmosis is common, such as the Ohio and Mississippi River valleys in the United States, have a higher risk of exposure.
However, understanding histoplasmosis, how it spreads, and who is at risk can help in taking preventive measures and seeking timely medical attention if symptoms arise.
Common Symptoms of Histoplasmosis
The symptoms can vary widely, especially in the early stages. Here’s an exhaustive list of the initial symptoms you might experience:
Initial Symptoms of Histoplasmosis
- Fever: A common early sign, often accompanied by chills.
- Cough: Persistent and sometimes dry.
- Fatigue: General tiredness and lack of energy.
- Chest Pain: Often described as a sharp or aching pain.
- Headache: Can be mild to severe.
- Muscle Aches: Often experienced throughout the body.
- Shortness of Breath: Difficulty breathing, especially with exertion.
- Joint Pain: Can affect one or multiple joints.
- Loss of Appetite: Leading to unintended weight loss.
- Night Sweats: Excessive sweating during the night.
Variation in Symptoms
The severity and form of histoplasmosis significantly influence the symptoms. Here’s how they can vary:
Acute Pulmonary Histoplasmosis
In mild cases, symptoms resemble those of a common cold or flu and might resolve without treatment. These include fever, cough, and fatigue. In more severe cases, acute pulmonary histoplasmosis can cause high fever, chest pain, and difficulty breathing.
Chronic Pulmonary Histoplasmosis
This form often affects individuals with pre-existing lung conditions, such as emphysema. Symptoms can be more severe and persistent, including a chronic cough, weight loss, and night sweats. Chest pain and shortness of breath are also common.
Disseminated Histoplasmosis
This is the most severe form and can affect multiple organs. It is more likely in individuals with weakened immune systems, such as those with HIV/AIDS. Symptoms can include severe fatigue, weight loss, high fever, and enlargement of the liver and spleen. Other symptoms might include skin lesions and oral ulcers.
However, understanding the variability in symptoms based on the severity and form of histoplasmosis is crucial for early detection and effective treatment. If you suspect you have been exposed to Histoplasma capsulatum, seek medical advice promptly.
Causes of Histoplasmosis: An In-Depth Look
Understanding the causes of histoplasmosis is crucial for prevention and management. Here’s a detailed look at the sources, environments, and risk factors associated with this infection.
The Fungal Source: Histoplasma capsulatum
Histoplasma capsulatum is a dimorphic fungus, meaning it can exist in two forms: as a mold in the environment and as a yeast in the human body. When people disturb environments where this fungus thrives, they can inhale the fungal spores, leading to infection. This transformation from mold to yeast is what causes histoplasmosis.
Environments Where Histoplasma Capsulatum Thrives
Histoplasma capsulatum flourishes in specific environments, particularly those rich in organic material. The most common environments include:
- Bird Droppings: Areas contaminated with bird droppings, such as chicken coops, pigeon roosts, and other bird habitats, provide a nutrient-rich environment for the fungus.
- Bat Droppings: Bat caves and other locations where bat guano accumulates are prime spots for Histoplasma growth.
- Soil: Soil, especially in regions with heavy organic content and near water bodies, can harbor the fungus. Agricultural fields, gardens, and construction sites are potential risk areas.
Activities and Conditions Increasing Risk of Exposure
Certain activities and conditions can increase the risk of exposure to Histoplasma capsulatum. These include:
- Disturbing Contaminated Soil: Activities like gardening, farming, or construction work that disturb the soil can release fungal spores into the air.
- Exploring Caves: Spelunking or cave exploration can expose individuals to bat droppings and subsequently to Histoplasma spores.
- Handling Birds or Cleaning Bird Droppings: Cleaning chicken coops, pigeon roosts, or other areas with accumulated bird droppings increases the risk of inhaling spores.
- Living or Working in Endemic Areas: Regions such as the Ohio and Mississippi River valleys in the United States are known for higher prevalence of Histoplasma, increasing the risk for residents and workers in these areas.
- Weakened Immune System: Individuals with compromised immune systems, such as those with HIV/AIDS, cancer patients, or those on immunosuppressive drugs, are at higher risk of developing severe histoplasmosis.
By understanding these sources, environments, and risk factors, individuals can take preventive measures to reduce their risk of histoplasmosis. Awareness and proper precautions are key to avoiding this potentially serious fungal infection.
Diagnosis of Histoplasmosis
Here, we will explore the primary diagnostic tests used and discuss the significance of medical history and physical examination in diagnosing histoplasmosis.
List of Diagnostic Tests Used
- Antigen Detection: This test is one of the most sensitive methods for diagnosing histoplasmosis, especially in severe cases. It involves detecting the presence of Histoplasma antigens in blood, urine, or tissues.
- Antibody Tests: These tests, including complement fixation and immunodiffusion, measure the body’s immune response to Histoplasma. They are particularly useful in chronic cases of the disease.
- Molecular Tests: PCR (Polymerase Chain Reaction) testing can detect Histoplasma DNA in a sample, which is helpful for a definitive diagnosis.
- Culture: Culturing the fungus from body fluids and tissues can provide a direct evidence of histoplasmosis, but it is a more time-consuming method.
- Imaging: Chest X-rays or CT scans are used to identify lung abnormalities caused by histoplasmosis.
- Biopsy: In cases where the infection has spread to other organs, a biopsy may be necessary to determine the extent and nature of the infection.
The Importance of Medical History and Physical Examination
Medical History: A detailed medical history is critical in diagnosing histoplasmosis. This includes asking about recent activities that might have exposed the patient to Histoplasma spores, such as excavation work or exposure to bat or bird droppings. Understanding the patient’s travel history is also crucial, as histoplasmosis is more prevalent in certain geographic regions.
Physical Examination: A thorough physical exam can provide additional clues to a diagnosis of histoplasmosis. Symptoms such as fever, chest pain, and a cough, coupled with findings like hepatosplenomegaly (enlarged liver and spleen) or lymphadenopathy (swollen lymph nodes), can prompt further diagnostic testing specific to histoplasmosis.
Diagnosing histoplasmosis accurately is essential for initiating the right treatment and preventing complications. While laboratory tests are indispensable, the role of a detailed medical history and thorough physical examination cannot be overstated. These elements together guide healthcare providers in making an informed diagnosis and tailoring the treatment plan to the patient’s specific needs.
Treatment Options for Histoplasmosis
Managing and treating this condition effectively depends on the severity of the symptoms and the specific needs of the patient. Below, we explore the various treatment methods available for histoplasmosis and discuss important considerations for different patient groups.
List of Treatment Methods
1. Antifungal Medications:
- Mild to Moderate Infections: For individuals displaying mild symptoms, treatment might not be necessary as symptoms can resolve on their own. However, for moderate cases, doctors typically recommend antifungal medications such as itraconazole.
- Severe Infections: In cases of severe histoplasmosis or chronic pulmonary histoplasmosis, amphotericin B might be administered initially, followed by itraconazole to prevent recurrence.
2. Monitoring and Supportive Care: Monitoring involves regular check-ups to assess the efficacy of the treatment and to make sure that the infection is resolving. Supportive care may include treatments to manage symptoms such as fever, cough, and fatigue.
3. Lifestyle Adjustments: Patients are advised to avoid areas where the Histoplasma capsulatum fungus is likely to be found, such as chicken coops and bat caves, to prevent reinfection.
4. Surgical Intervention: In rare cases, if the infection leads to complications like lung nodules or significant scarring, surgical interventions may be required.
Considerations for Different Patient Groups
Immunocompromised Patients: Patients with weakened immune systems, including those with HIV/AIDS or those undergoing cancer treatments, are at higher risk of severe infection. They require prompt and aggressive treatment with antifungal medications. Long-term maintenance therapy may be necessary to prevent recurrence.
Children: The treatment approach in children generally mirrors that in adults, but dosage and medication choice must be carefully considered to suit their age and weight. Pediatric infectious disease specialists should be involved in the treatment planning.
Pregnant Women: Treating histoplasmosis in pregnant women requires special consideration to avoid harm to the fetus. Amphotericin B, although effective, is generally reserved for more severe cases due to its potential side effects.
Elderly Patients: Elderly patients may have other underlying conditions that can complicate the treatment of histoplasmosis. A more cautious approach may be needed, and interactions with other medications must be carefully managed.
However, early diagnosis and tailored treatment strategies are crucial for effective management and to minimize the risk of complications. Regular follow-ups and adjustments in the treatment plan may be necessary to ensure the best outcomes for each patient.
Preventing Histoplasmosis
Histoplasmosis is a fungal infection caused by inhaling spores of the Histoplasma fungus, which thrives in environments with bird or bat droppings. To reduce the risk of contracting this infection, follow these essential tips and strategies:
1. Avoid High-Risk Areas
- Stay Away from Contaminated Soil: Avoid disturbing soil that may contain bird or bat droppings, such as areas near chicken coops, bird roosts, and old buildings.
- Check Before Entering: Before entering caves, old barns, or other high-risk areas, assess the likelihood of fungal contamination.
2. Use Protective Gear
- Wear Masks: When working in or around high-risk areas, always wear a mask that can filter out fungal spores. N95 respirators are recommended for optimal protection.
- Protective Clothing: Wear gloves, long sleeves, and long pants to minimize skin exposure to contaminated materials.
3. Safe Practices for Outdoor Activities
- Wet the Soil: If you must disturb soil in high-risk areas, dampen it first to reduce the number of airborne spores.
- Avoid Direct Contact: Refrain from touching your face, eyes, or mouth when working in potentially contaminated areas.
4. Control Bird and Bat Populations
- Regular Cleaning: Clean areas regularly to prevent the accumulation of bird or bat droppings. Use water to moisten the droppings before removal to prevent spores from becoming airborne.
- Exclusion Techniques: Implement exclusion techniques to prevent birds and bats from nesting in buildings and other structures.
5. Stay Informed and Educated
- Know the Risks: Be aware of the symptoms of histoplasmosis, which include fever, cough, and fatigue. Early detection and treatment are crucial.
- Educate Others: Inform family, friends, and colleagues about the risks and preventive measures to help reduce the spread of histoplasmosis.
By following these tips and strategies, you can significantly reduce the risk of contracting histoplasmosis and ensure a safer environment for yourself and others.
FAQs about Histoplasmosis Symptoms
What are the common symptoms of histoplasmosis?
Histoplasmosis often starts with flu-like symptoms such as fever, chills, muscle aches, and headache. As the infection progresses, you might experience a cough, chest pain, and fatigue. Some individuals may also develop a rash or joint pain.
How long after exposure do symptoms appear?
Symptoms of histoplasmosis typically appear 3 to 17 days after exposure to the fungus Histoplasma capsulatum. The onset and severity of symptoms can vary based on the individual’s immune system and the extent of exposure.
Can histoplasmosis be asymptomatic?
Yes, many people infected with histoplasmosis do not show any symptoms. This is especially common in individuals with healthy immune systems. However, those with weakened immune systems or underlying health conditions are more likely to experience noticeable symptoms.
Is histoplasmosis contagious?
Histoplasmosis is not contagious and cannot be spread from person to person. It is contracted by inhaling spores from the environment, often from bird or bat droppings in soil.
What should I do if I suspect I have histoplasmosis?
If you suspect you have histoplasmosis, especially if you have been in an area known for the fungus, seek medical attention. Early diagnosis and treatment can prevent complications, particularly in individuals with compromised immune systems.
Conclusion
Recognizing the symptoms of histoplasmosis is crucial for early diagnosis and effective treatment. By understanding the signs and seeking timely medical attention, you can significantly improve health outcomes.
If you are at risk or experience symptoms such as fever, cough, or fatigue, it’s important to consult a healthcare provider promptly. Early intervention can make all the difference in managing this potentially serious infection. Stay informed, stay vigilant, and prioritize your health.
References
Citing reputable sources is essential for validating the information provided on histoplasmosis symptoms. Here are some trusted references for further reading:
- Centers for Disease Control and Prevention (CDC) – For comprehensive information on histoplasmosis, including symptoms, treatment, and prevention. Visit CDC’s histoplasmosis page.
- Mayo Clinic – Detailed insights on histoplasmosis symptoms, diagnosis, and management. Explore Mayo Clinic’s guide to histoplasmosis.
- MedlinePlus – A reliable source for medical information, offering an overview of histoplasmosis, its causes, and symptoms. Check out MedlinePlus on histoplasmosis.
- American Lung Association – Provides information on how histoplasmosis affects lung health and what to look out for. Learn more from the American Lung Association.
These references offer credible and detailed information to help you understand histoplasmosis better.