Histoplasmosis Treatment: Histoplasmosis is a fungal infection caused by the inhalation of spores from the fungus Histoplasma capsulatum.
This disease is prevalent in certain parts of the United States, particularly in the Ohio and Mississippi River valleys. It primarily affects the lungs but can also disseminate to other parts of the body, especially in immunocompromised individuals.
Understanding the diagnosis and treatment of histoplasmosis is crucial for effective management and improved patient outcomes.
Understanding Histoplasmosis
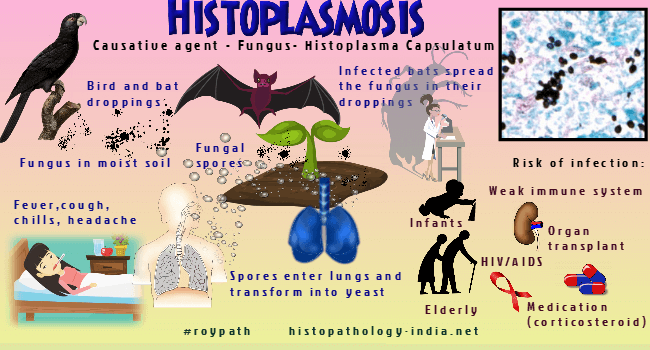
Histoplasmosis is a fungal infection caused by inhaling the spores of the fungus Histoplasma capsulatum. This condition primarily affects the lungs but can also impact other parts of the body. Here’s a deeper look into the causes, epidemiology, symptoms, and progression of histoplasmosis.
Causes of Histoplasmosis
Histoplasmosis is caused by the fungus Histoplasma capsulatum. The spores of this fungus are found in environments rich in bat and bird droppings, such as:
- Bird roosts
- Old barns
- Caves
- Poultry houses
Disturbance of these habitats, such as during excavation or demolition, can release the spores into the air, making them easy to inhale and leading to infection.
Epidemiology: Prevalence and Risk Factors
Histoplasmosis is most commonly found in certain geographic regions, particularly:
- The central and eastern United States, especially areas around the Ohio and Mississippi River valleys
- Parts of Central and South America
- Africa
- Asia
- Australia
People most at risk include:
- Farmers
- Poultry keepers
- Construction workers
- Speleologists (cave explorers)
- Archaeologists
Anyone who disturbs areas where the spores are likely to be present can be at risk, but those with weakened immune systems, such as individuals with HIV/AIDS or those on immunosuppressive drugs, are more susceptible to severe forms of the disease.
Common Symptoms and Progression of the Disease
The symptoms of histoplasmosis vary greatly, ranging from very mild to severe, and depend largely on the amount of spores inhaled. Common symptoms include:
- Fever
- Cough
- Fatigue
- Chills
- Headache
- Chest pain
- Body aches
In mild cases, histoplasmosis can resolve on its own without treatment. However, severe cases, especially in those with compromised immune systems, may require antifungal medication. The disease can progress significantly if left untreated, potentially leading to chronic lung disease or disseminated histoplasmosis, which affects multiple organs and can be fatal.
However, understanding the risks and symptoms of histoplasmosis is crucial, especially for those living in or visiting high-risk areas or those engaged in activities that disturb soil. Early diagnosis and treatment are key to managing the effects of this infectious disease.
Diagnosis of Histoplasmosis
Diagnosing histoplasmosis involves a series of steps to accurately identify the infection, differentiate between acute and chronic forms, and determine the most effective treatment plan. Below are the critical aspects of diagnosing histoplasmosis:
Steps in Diagnosing Histoplasmosis
- Clinical Evaluation: The process begins with a thorough medical history and physical examination to identify symptoms and risk factors.
- Laboratory Tests: Blood and other laboratory tests are conducted to detect histoplasmosis markers.
- Imaging Techniques: Imaging such as chest X-rays or CT scans help visualize lung involvement.
- Tissue Biopsy: In certain cases, a biopsy of affected tissue may be necessary to confirm the diagnosis.
Differentiating Between Acute and Chronic Histoplasmosis
- Acute Histoplasmosis: This form typically occurs after a large exposure to Histoplasma spores and presents with flu-like symptoms such as fever, cough, and fatigue. It is often self-limiting.
- Chronic Histoplasmosis: More common in individuals with pre-existing lung conditions, chronic histoplasmosis develops slowly and presents with symptoms like weight loss, night sweats, and a persistent cough.
Diagnostic Tools and Tests
- Blood Tests: Blood tests are crucial in diagnosing histoplasmosis. They can detect antibodies or antigens associated with the Histoplasma fungus, providing a preliminary diagnosis.
- Imaging Techniques: Chest X-rays and CT scans are used to detect abnormalities in the lungs that are indicative of histoplasmosis. These imaging techniques help in assessing the extent and severity of the infection.
- Tissue Biopsy: When other tests are inconclusive, a biopsy of lung tissue or other affected areas can be performed. Microscopic examination of the tissue can confirm the presence of Histoplasma fungi.
The Role of Medical History and Physical Examination
A comprehensive medical history and physical examination are foundational in diagnosing histoplasmosis. Understanding the patient’s exposure to environments where Histoplasma is prevalent (e.g., bird or bat droppings) and recognizing symptoms aligned with histoplasmosis are critical first steps. Physical examination helps identify signs such as enlarged lymph nodes or abnormal lung sounds, further guiding the diagnostic process.
However, the diagnosis of histoplasmosis involves a combination of clinical evaluation, laboratory tests, imaging techniques, and sometimes tissue biopsy. Differentiating between acute and chronic forms is essential for effective treatment, and a thorough medical history and physical examination play a vital role in accurate diagnosis.
Treatment Options for Histoplasmosis
Histoplasmosis treatment varies depending on the severity of the disease. For mild to moderate cases, antifungal medications are typically effective, while severe or disseminated histoplasmosis may require more aggressive treatment strategies.
First-Line Treatments
Antifungal Medications
The primary treatment for histoplasmosis involves antifungal medications. The most commonly prescribed drugs are:
- Itraconazole: Often the first choice for treating mild to moderate histoplasmosis. It is usually administered orally.
- Amphotericin B: Used for more severe cases or when initial treatment with itraconazole is ineffective. This medication is typically administered intravenously.
Duration and Dosage Recommendations
- Itraconazole: For mild to moderate histoplasmosis, the usual dosage is 200 mg once or twice daily for 6 to 12 weeks.
- Amphotericin B: For severe cases, the typical dosage ranges from 0.7 to 1 mg/kg per day, administered over several weeks.
Treatment for Severe or Disseminated Histoplasmosis
In cases of severe or disseminated histoplasmosis, a more intensive treatment approach is required. This often involves an initial course of Amphotericin B to rapidly control the infection, followed by a prolonged course of itraconazole to ensure complete eradication of the fungus.
Considerations for Immunocompromised Patients
Patients with compromised immune systems, such as those with HIV/AIDS, organ transplant recipients, or individuals undergoing chemotherapy, require special consideration. These patients are at higher risk for severe or disseminated histoplasmosis and may need longer courses of antifungal therapy, close monitoring, and potentially adjunctive treatments to manage their condition effectively.
Emerging Treatments and Clinical Trials
Research is ongoing to develop new and more effective treatments for histoplasmosis. Emerging therapies and clinical trials are exploring:
- Novel Antifungal Agents: Investigating new drugs that target the fungus more effectively or have fewer side effects.
- Immunotherapy: Enhancing the body’s immune response to fight the infection more effectively.
- Combination Therapies: Combining existing antifungal medications with other treatments to improve outcomes.
Staying informed about the latest developments in histoplasmosis treatment can help patients and healthcare providers make the best decisions for managing this disease.
Managing Side Effects and Follow-up Care for Histoplasmosis
Histoplasmosis treatment can be crucial in managing the infection effectively, but it’s important to be aware of the potential side effects and the need for comprehensive follow-up care. Here’s how patients can manage side effects and ensure long-term health after treatment.
Common Side Effects of Histoplasmosis Treatment
Treatment for histoplasmosis, particularly when involving antifungal medications such as Itraconazole or Amphotericin B, can lead to various side effects. Some of the most commonly reported side effects include:
- Nausea and Vomiting: These are frequent side effects, especially with potent antifungal medications.
- Headaches: Patients might experience mild to severe headaches as a response to medication or the underlying infection.
- Rash: Skin reactions can occur, typically manifesting as rashes that may or may not be itchy.
- Liver Enzyme Abnormalities: Antifungals can affect liver function, necessitating regular monitoring of liver enzymes.
- Fatigue: Feeling unusually tired is a common effect of both the infection and its treatment.
Understanding these side effects can help patients and healthcare providers manage them more effectively, reducing discomfort and preventing more serious health issues.
Monitoring and Managing Long-Term Health After Treatment
After the completion of histoplasmosis treatment, monitoring long-term health is crucial to ensure that the infection has been fully resolved and to address any complications that may arise. Key aspects include:
- Regular Blood Tests: To check for liver health and ensure that blood counts are normal.
- Lung Function Tests: If the infection had affected the lungs, periodic checks might be needed to assess any long-term impact on lung capacity and function.
- Renal Function: Since some antifungal medications can impact kidney function, renal tests might be necessary.
Managing these aspects with the help of healthcare professionals ensures that any lingering effects of the infection are addressed promptly.
Importance of Follow-Up Visits to Prevent Recurrence
Follow-up visits play a pivotal role in the recovery process and in preventing the recurrence of histoplasmosis. These visits allow healthcare providers to:
- Assess the Effectiveness of Treatment: To ensure that the infection is responding well to treatment.
- Detect Early Signs of Recurrence: Early detection can prevent more serious complications.
- Adjust Medications if Needed: Based on side effects or response to treatment.
- Provide Guidance on Health Maintenance: Including lifestyle adjustments or dietary changes to support recovery.
These visits are essential not just for health monitoring but also for reassuring patients and guiding them through their recovery journey.
By managing side effects effectively and adhering to a structured follow-up care plan, patients can achieve better outcomes and minimize the risk of histoplasmosis recurrence. Regular communication with healthcare providers is key to navigating this process successfully.
Prevention and Awareness of Histoplasmosis
Effective prevention and awareness are key to reducing the incidence of this disease. Here, we explore the preventive measures individuals can take, the public health strategies that are vital for education, and the role of healthcare providers in raising awareness and facilitating early detection.
Preventive Measures to Avoid Exposure to the Fungus
- Avoid Risky Areas: Since the fungus thrives in environments rich in bird or bat droppings, avoid activities in such areas, especially in enclosed spaces like caves or abandoned buildings.
- Use Protective Gear: When working in potentially contaminated areas, such as during gardening or excavation near bird roosts or old buildings, wear protective respirators and clothing.
- Control Dust: If you must disturb soil or other materials where spores might be present, wetting down the area can help minimize the amount of dust and spores kicked up into the air.
- Home and Workplace Safety: Ensure that buildings are properly maintained to avoid the accumulation of bird or bat droppings, and clean these areas with appropriate safety measures in place.
- Educate Yourself and Others: Being aware of the risks and transmission methods of Histoplasma capsulatum can drastically reduce exposure chances.
Public Health Strategies and Education on Histoplasmosis
- Public Awareness Campaigns: Health departments can run informational campaigns to educate the public about the risks of histoplasmosis, particularly in endemic areas.
- Information Distribution: Distributing brochures, posters, and digital content that detail preventative practices and the importance of avoiding high-risk areas.
- School and Community Education: Implementing educational programs in schools and community centers that discuss how to recognize potential fungal habitats and avoid them.
- Collaboration with Local Organizations: Partnering with local wildlife, environmental, and health organizations to broaden the reach of educational efforts.
- Research and Surveillance: Encouraging ongoing research and maintaining surveillance to monitor and respond to cases of histoplasmosis effectively.
Role of Healthcare Providers in Raising Awareness and Early Detection
- Educational Outreach: Healthcare providers can educate patients about histoplasmosis, especially those who live in or travel to endemic areas.
- Screening and Reporting: Providers should consider histoplasmosis in differential diagnoses for patients presenting with respiratory symptoms and a history of exposure to high-risk environments.
- Community Engagement: Engaging in community outreach programs to spread awareness about the disease, its symptoms, and the importance of early medical consultation.
- Professional Development: Keeping abreast of the latest developments and guidelines in diagnosing and treating histoplasmosis through continuous medical education.
- Patient Counseling: Advising patients on how to reduce exposure risks, particularly immunocompromised individuals who are more susceptible to severe infections.
By integrating these preventive measures, educational strategies, and healthcare initiatives, communities can significantly reduce the risks associated with histoplasmosis and improve public health outcomes.
FAQs about Histoplasmosis Treatment
What is histoplasmosis and how is it treated?
Histoplasmosis is a fungal infection caused by inhaling the spores of the fungus Histoplasma capsulatum. Treatment depends on the severity of the infection. Mild cases may not require treatment beyond monitoring, as symptoms often resolve on their own. More severe cases, especially those involving the lungs or spread throughout the body, may require antifungal medications such as itraconazole or amphotericin B.
Who needs treatment for histoplasmosis?
Not everyone exposed to Histoplasma capsulatum will require treatment. People with mild symptoms may recover without medication. However, those with weakened immune systems, underlying health conditions, or severe infections typically need antifungal treatment. It is crucial to consult with a healthcare provider if you suspect you have histoplasmosis.
How long does treatment for histoplasmosis last?
The duration of treatment for histoplasmosis can vary. For acute pulmonary histoplasmosis, antifungal therapy might be prescribed for several weeks to months. For chronic or disseminated histoplasmosis, treatment could extend for at least a year to ensure the infection is fully cleared.
Are there any side effects of histoplasmosis treatment?
Yes, antifungal medications can have side effects. Common side effects of itraconazole include nausea, rash, and liver enzyme abnormalities. Amphotericin B, used for more severe cases, can cause kidney issues, fever, and chills. Monitoring by a healthcare provider is important to manage any adverse effects and adjust treatment as necessary.
Can histoplasmosis be prevented?
While complete avoidance of the fungus in endemic areas is challenging, reducing exposure to dust in places where the fungus is likely to grow, such as chicken coops and old barns, can help. Wearing masks and using protective equipment during excavation or construction can also reduce the risk of inhaling spores.
Conclusion
Recognizing, diagnosing, and effectively treating histoplasmosis is crucial for maintaining good health, particularly in regions where this fungal infection is prevalent. As we’ve explored, histoplasmosis can range from mild to severe, and understanding its symptoms and risk factors is key. Early diagnosis and appropriate treatment can significantly improve outcomes for those affected.
If you are in an at-risk population or live in an area known for histoplasmosis, it’s essential to be aware of the potential exposure to this fungus. We encourage anyone who suspects they might be affected or experiences symptoms such as fever, cough, and fatigue, to seek medical advice promptly. Early medical intervention is your best defense against the complications associated with histoplasmosis. Stay informed, stay cautious, and ensure your health is always a priority.
References
For those looking to delve deeper into the treatment of histoplasmosis and validate the information provided, here are some reputable sources worth consulting:
- Centers for Disease Control and Prevention (CDC) – This resource offers comprehensive information on the diagnosis, treatment, and prevention of histoplasmosis. CDC on Histoplasmosis.
- Mayo Clinic – The Mayo Clinic provides detailed patient-friendly information about the symptoms, causes, and treatment options for histoplasmosis. Mayo Clinic’s Histoplasmosis Guide.
- National Organization for Rare Disorders (NORD) – NORD offers insights into histoplasmosis with in-depth details about the condition, including risk factors and therapeutic procedures. NORD on Histoplasmosis.
- Medscape – For a more medical professional-targeted approach, Medscape’s resource on histoplasmosis includes news, case studies, and treatment protocols. Medscape Histoplasmosis Resource.
- PubMed Central – An invaluable resource for academic and clinical studies, offering access to numerous research articles and studies on histoplasmosis. PubMed Central Search for Histoplasmosis.
These sources are instrumental for patients, healthcare professionals, and anyone interested in understanding more about histoplasmosis and its management.