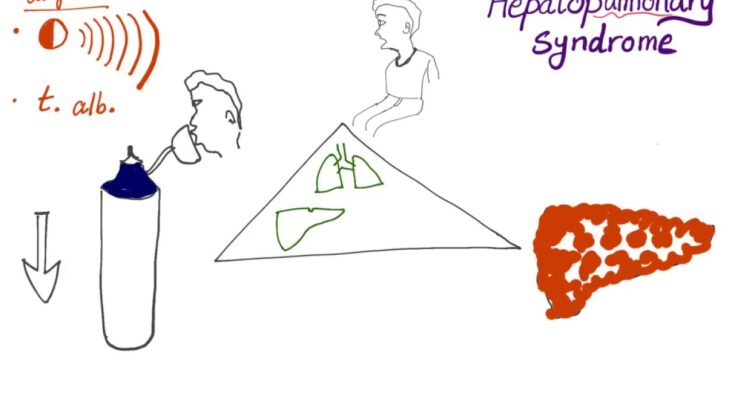
Hepatopulmonary Syndrome Symptoms: Hepatopulmonary Syndrome (HPS) is a complex medical condition that arises as a complication of liver disease.
It is characterized by the presence of a liver disorder coupled with lung abnormalities and abnormalities in blood oxygenation.
This article delves into the symptoms and causes of Hepatopulmonary Syndrome, offering a comprehensive understanding of this lesser-known yet significant condition.
What is Hepatopulmonary Syndrome?
Hepatopulmonary Syndrome (HPS) is a medical condition that occurs when liver disease leads to abnormalities in the lungs’ blood vessels. This condition typically arises in individuals with chronic liver disease or cirrhosis, and it involves the expansion (or dilation) of blood vessels in the lungs which impairs the oxygen exchange process. As a result, patients with HPS often experience shortness of breath and lower oxygen levels in their blood, particularly when they are upright.
Epidemiology: Prevalence and Risk Factors
The prevalence of Hepatopulmonary Syndrome varies widely, depending on the severity and type of underlying liver disease. Studies suggest that HPS affects between 10% to 30% of patients with cirrhosis. The risk of developing HPS increases with the progression of liver disease. Key risk factors include the presence of advanced liver cirrhosis, portal hypertension (high blood pressure in the liver’s blood vessels), and more severe liver dysfunction. Both the duration and severity of liver disease can influence the likelihood of developing HPS, making early diagnosis and management of liver conditions crucial.
Connection Between Liver Dysfunction and Lung Health
The connection between liver dysfunction and lung health is complex and significant. The liver plays a crucial role in filtering toxins from the blood and managing blood clotting; when it’s impaired, these functions can deteriorate, leading to systemic complications including issues in the lungs. In HPS, liver dysfunction leads to an imbalance in the production and breakdown of certain chemicals and hormones that regulate blood vessel behavior. This imbalance promotes the dilation of blood vessels in the lungs, which, while increasing blood flow, reduces the efficiency of oxygen transfer to the bloodstream. This interaction showcases how interconnected our organ systems are, with liver health having a profound impact on pulmonary function.
Symptoms of Hepatopulmonary Syndrome
Recognizing the symptoms early can significantly impact the management of the condition. Here, we explore the early signs, common symptoms, their progression over time, and provide hypothetical patient stories to illustrate the impact of HPS.
Early Signs and Common Symptoms
The early signs of Hepatopulmonary Syndrome can be subtle and often overlap with symptoms of underlying liver disease. Key early symptoms include:
- Shortness of Breath: This is often noticed during physical activity but can occur even at rest in more severe cases.
- Increased Breathing Rate: Patients may find themselves breathing more rapidly, especially during exertion.
- Cyanosis: A bluish tinge to the skin, lips, or fingernails, indicating low oxygen levels in the blood.
- Clubbing: Swelling and softening of the fingertips or toes, with nails that may curve downward.
- Fatigue: Generalized tiredness and a decrease in stamina, which are common to many liver disorders but can be exacerbated by oxygen deficits.
How Symptoms Progress Over Time
As Hepatopulmonary Syndrome advances, symptoms typically increase in both frequency and severity:
- Worsening Shortness of Breath: Initially noticeable only during exercise, this symptom can become a constant issue as the syndrome progresses.
- Platypnea: A unique symptom of HPS, where breathing difficulty increases when standing up from a sitting or lying position.
- Orthodeoxia: A drop in oxygen levels when standing up, which can be detected through pulse oximetry tests.
- Gastrointestinal Issues: As liver function worsens, issues such as abdominal swelling (ascites) and varices may occur, complicating the overall health picture.
Hypothetical Case Studies
Case Study 1: John, a 52-year-old with chronic liver disease
John has been managing chronic liver disease for several years. Recently, he has noticed an increased difficulty in breathing, particularly when engaging in activities like walking his dog. His condition worsened over a few months, leading to fatigue that interfered with his daily activities. An evaluation revealed low blood oxygen levels, and subsequent investigations confirmed the diagnosis of Hepatopulmonary Syndrome.
Case Study 2: Maria, a 45-year-old school teacher
Maria, previously diagnosed with liver cirrhosis, began experiencing unusual symptoms such as shortness of breath and a bluish tinge to her lips after exertion. Her symptoms became more pronounced over time, affecting her ability to teach. A visit to her doctor and the appearance of clubbing in her fingers led to further tests that diagnosed HPS. Maria’s treatment focused on managing her liver condition alongside her breathing issues.
By staying informed about conditions like HPS, patients and healthcare providers can better navigate the challenges they present. Remember, if you or someone you know is experiencing symptoms similar to those described, it is important to consult a healthcare provider for a comprehensive evaluation.
Causes and Pathophysiology of Hepatopulmonary Syndrome
Understanding its causes and pathophysiology is essential for medical professionals and patients alike to manage this syndrome effectively. This section will explore the triggers of HPS, the role of arterial gas exchange and pulmonary vasodilation, and the impact of liver cirrhosis on lung function.
Causes of Hepatopulmonary Syndrome
HPS is primarily associated with liver disease, particularly cirrhosis and, in some cases, acute liver failure. The main causes include:
- Chronic Liver Diseases: Chronic conditions such as hepatitis, alcoholic liver disease, and nonalcoholic fatty liver disease can lead to cirrhosis, which is the most common precursor of HPS.
- Portal Hypertension: This condition, characterized by increased blood pressure within the portal venous system, is commonly observed in cirrhosis patients and is a key contributor to the development of HPS.
- Genetic Factors: Although not fully understood, genetic predispositions may play a role in the susceptibility to HPS in individuals with liver disease.
The Role of Arterial Gas Exchange and Pulmonary Vasodilation
The pathophysiology of HPS involves two critical aspects: impaired arterial gas exchange and pulmonary vasodilation.
- Impaired Arterial Gas Exchange: In HPS, the ability of the lungs to exchange gases (oxygen and carbon dioxide) is compromised. This impairment is primarily due to the formation of microscopic blood vessels (microvascular dilatation) in the lung, which allows blood to bypass the normal oxygenation process.
- Pulmonary Vasodilation: There is an abnormal widening of blood vessels within the lungs in HPS, driven by various biological mediators such as nitric oxide. This vasodilation contributes to an increased blood flow to poorly ventilated areas of the lung, further exacerbating the gas exchange inefficiency.
Impact of Liver Cirrhosis on Lung Function
Liver cirrhosis significantly impacts lung function, manifesting in several ways:
- Decreased Oxygenation: Cirrhosis can lead to a reduction in the oxygen-carrying capacity of the blood, resulting in lower oxygen levels in the arterial blood.
- Vascular Alterations: The structural and functional changes in the pulmonary blood vessels not only affect gas exchange but also lead to an increased risk of respiratory complications.
- Pulmonary Hypertension: In some cases, cirrhosis can contribute to the development of pulmonary hypertension, a serious condition that can complicate the management of HPS.
Addressing these aspects is crucial in the treatment and management of HPS, highlighting the interconnected nature of liver and lung health.
Diagnosing Hepatopulmonary Syndrome
Diagnosing HPS requires a careful and systematic approach using several diagnostic tests and criteria. Below, we explore the common diagnostic tools and their roles in confirming the presence of HPS.
Common Diagnostic Tests and Criteria
The diagnosis of Hepatopulmonary Syndrome hinges on three primary criteria:
- Liver Disease: Chronic liver disease or portal hypertension must be present. This is typically established through patient history, clinical examination, and liver function tests.
- Pulmonary Gas Exchange Abnormalities: Evidence of abnormal gas exchange is crucial. This is generally assessed by measuring the levels of oxygen in the blood.
- Intrapulmonary Vascular Dilatations (IPVDs): The presence of abnormal blood vessels in the lungs, which are typically assessed using imaging tests.
The Role of Arterial Blood Gas Analysis
Arterial blood gas (ABG) analysis is pivotal in diagnosing Hepatopulmonary Syndrome. This test measures the partial pressures of oxygen (PaO2) and carbon dioxide (PaCO2) in the arterial blood, providing insight into the patient’s ability to oxygenate and remove carbon dioxide. In HPS, ABG typically shows hypoxemia — a reduced level of blood oxygen. This test is often supplemented by measuring the alveolar-arterial (A-a) gradient, which helps confirm the presence of a gas exchange abnormality, a defining characteristic of HPS.
Imaging Tests and Their Significance
Imaging plays a critical role in diagnosing HPS, with specific tests aimed at confirming the presence of intrapulmonary vascular dilatations:
- Contrast-enhanced Echocardiogram: This is one of the most important diagnostic tools for HPS. It involves the injection of saline contrast (agitated saline) into a peripheral vein during an echocardiogram. The appearance of microbubbles in the left heart chamber, typically within three to six cardiac cycles after their appearance in the right heart, indicates the presence of intrapulmonary shunts typical of HPS.
- Pulmonary Angiography: While not routinely used due to its invasive nature, pulmonary angiography can be utilized in complex cases to visualize the pulmonary vascular anatomy directly.
- Chest X-ray and CT Scan: These are more general imaging tests that can help rule out other causes of hypoxemia and detect complications related to liver disease but are not specific for diagnosing HPS.
In summary, diagnosing Hepatopulmonary Syndrome requires a multidisciplinary approach involving a detailed examination of liver function, arterial blood gas analysis to assess gas exchange, and specific imaging tests to confirm intrapulmonary vascular abnormalities. Early and accurate diagnosis is crucial to managing the condition effectively and improving patient outcomes.
Treatment Options for Hepatopulmonary Syndrome
Managing HPS effectively is crucial for improving quality of life and outcomes. Here, we explore the current treatment strategies, the role of liver transplantation, and supportive therapies along with lifestyle modifications that can help manage symptoms.
Current Treatment Strategies for Hepatopulmonary Syndrome
Treating HPS focuses primarily on addressing the underlying liver condition while managing the symptoms related to oxygen deprivation. Currently, there are no specific medical treatments approved solely for HPS, making the management of the underlying liver disease and symptomatic care pivotal. However, researchers are exploring various potential therapies that could directly target the pathophysiological changes in the lungs associated with HPS.
- Oxygen Therapy: This is commonly prescribed to alleviate symptoms of hypoxemia (low blood oxygen levels). Regular oxygen supplementation can help maintain adequate oxygen levels in the blood, improving patient comfort and activity levels.
- Medication: While no drugs are currently approved specifically for HPS, medications that treat the liver disease itself, like those used in cirrhosis or hepatitis, are integral to the overall management strategy.
Role of Liver Transplantation
Liver transplantation is currently the only known cure for HPS. It has been shown to improve or resolve the pulmonary symptoms in most patients. The eligibility for a liver transplant depends on multiple factors, including the severity of liver disease, the presence of other medical conditions, and overall health status. Post-transplant, many patients experience significant improvements in lung function and a reduction in symptoms, highlighting the effectiveness of this treatment in severe cases.
Supportive Therapies and Lifestyle Modifications
In addition to medical treatments, supportive therapies and lifestyle changes play a critical role in managing HPS:
- Nutritional Support: A balanced diet tailored to liver health can help manage symptoms and improve overall well-being. Patients are often advised to limit salt intake and consume high-energy foods that are easier on the liver.
- Physical Activity: Gentle exercises, under medical supervision, can help maintain muscle tone and improve cardiovascular health without overstraining the body.
- Avoiding Alcohol: Alcohol can exacerbate liver disease, so abstinence is crucial for patients with HPS.
- Regular Monitoring: Frequent medical check-ups are necessary to monitor the progress of liver disease and adjust treatments as needed.
By integrating these treatments and lifestyle adjustments, patients with Hepatopulmonary Syndrome can achieve better management of their symptoms and an improved quality of life. Early diagnosis and a comprehensive treatment approach are essential to managing the complexities of HPS effectively.
Prevention and Management of Hepatopulmonary Syndrome
Understanding how to prevent and manage this syndrome can significantly enhance quality of life and improve outcomes. Here’s a guide on preventive measures for at-risk populations, effective symptom management, and the importance of regular medical check-ups and liver health monitoring.
Preventive Measures for At-Risk Populations
Preventing Hepatopulmonary Syndrome begins with addressing the underlying liver conditions that predispose individuals to the syndrome. Individuals with chronic liver disease or cirrhosis are at heightened risk and should take the following steps:
- Maintain a Healthy Lifestyle: A balanced diet, regular exercise, and avoiding alcohol and tobacco can help maintain liver health and reduce the risk of HPS.
- Regular Liver Health Screenings: Early detection of liver problems allows for timely intervention which can prevent the progression to HPS.
- Vaccinations: Staying up to date with vaccinations can prevent infections that may exacerbate liver disease.
Managing Symptoms Effectively
Once HPS develops, managing symptoms effectively is crucial for maintaining quality of life. Key strategies include:
- Oxygen Therapy: Many patients with HPS benefit from supplemental oxygen, which can alleviate the hypoxemia (low blood oxygen levels) characteristic of the syndrome.
- Medication Management: Certain medications can help manage the symptoms of HPS. Consulting with a healthcare provider for the most suitable options is essential.
- Pulmonary Rehabilitation: Engaging in pulmonary rehabilitation can improve lung efficiency and overall physical stamina.
Importance of Regular Medical Check-Ups and Liver Health Monitoring
Regular medical check-ups play a vital role in both preventing HPS and managing it effectively if it occurs. These check-ups should include:
- Comprehensive Liver Function Tests: Regular testing helps track liver health and detect any deterioration that might lead to complications like HPS.
- Consultations with Specialists: Regular visits to a hepatologist or a pulmonologist can help manage the complexities of HPS.
- Monitoring for Early Symptoms: Early detection of symptoms such as shortness of breath, blue discoloration of the skin (cyanosis), or clubbing of the fingers is crucial for timely intervention.
However, while Hepatopulmonary Syndrome is a serious health condition, taking preventive measures, effectively managing symptoms, and maintaining regular medical check-ups can greatly assist in managing the disease and improving overall well-being.
FAQs about Hepatopulmonary Syndrome
What is Hepatopulmonary Syndrome?
Hepatopulmonary Syndrome (HPS) is a medical condition that occurs when liver disease, such as cirrhosis, causes abnormalities in the lungs, leading to oxygenation problems. It is characterized by the widening of blood vessels in the lungs, which impairs the efficient exchange of oxygen and can result in breathing difficulties.
What causes Hepatopulmonary Syndrome?
The exact cause of Hepatopulmonary Syndrome is not completely understood, but it is closely linked to advanced liver disease. Factors contributing to HPS may include the release of certain chemicals or substances by the diseased liver that lead to the expansion of blood vessels in the lungs.
What are the symptoms of Hepatopulmonary Syndrome?
Symptoms of HPS can vary but typically include shortness of breath, especially when upright (a condition known as platypnea), bluish discoloration of the skin or lips (cyanosis), and clubbing of the fingers. These symptoms tend to worsen over time as the liver disease progresses.
How is Hepatopulmonary Syndrome diagnosed?
Diagnosing HPS involves a combination of clinical evaluation, blood tests, imaging studies like chest X-rays or echocardiograms, and specialized tests to measure the efficiency of gas exchange in the lungs. A definitive diagnosis usually requires a contrast echocardiography, which can detect abnormal connections between blood vessels in the lungs.
How can Hepatopulmonary Syndrome be treated?
Treatment options for HPS are primarily aimed at managing the underlying liver disease. In cases where liver function is severely compromised, a liver transplant may be considered, which can reverse the symptoms of HPS in many patients. Other supportive treatments may include oxygen therapy to help alleviate symptoms of low oxygen levels in the blood.
Is there a cure for Hepatopulmonary Syndrome?
Currently, there is no direct cure for HPS other than liver transplantation in suitable candidates. Managing the underlying liver disease and supportive treatments to alleviate symptoms are the primary approaches to care.
How common is Hepatopulmonary Syndrome?
Hepatopulmonary Syndrome is considered a rare complication of liver disease. It is estimated to affect between 10% to 30% of patients with cirrhosis or other chronic liver diseases, although the severity and symptoms can vary significantly among individuals.
Can lifestyle changes help with Hepatopulmonary Syndrome?
While lifestyle changes cannot cure HPS, they can help manage the symptoms and underlying liver conditions. Recommendations typically include avoiding alcohol, maintaining a healthy diet, and managing weight. Regular monitoring and medical care are crucial for managing the progression of liver disease and its complications.
Conclusion
In this article, we discussed the critical aspects of Hepatopulmonary Syndrome (HPS), a complex condition that arises from liver disease and affects the lungs, leading to a variety of respiratory symptoms. Key points to remember include the primary symptoms of HPS, such as shortness of breath and blue-tinged skin (cyanosis), as well as its causes, which are generally linked to advanced liver disease and increased blood flow to the lungs.
Early diagnosis and treatment of Hepatopulmonary Syndrome are essential. Timely intervention can significantly improve the quality of life and overall outcomes for those affected. Treatments may vary but often focus on managing the underlying liver condition and addressing the oxygenation issues in the lungs.
If you or someone you know is experiencing symptoms that could be related to Hepatopulmonary Syndrome, it’s crucial to consult a healthcare professional. Medical experts can provide a thorough evaluation and recommend an appropriate treatment plan based on individual health needs. Remember, addressing concerns early with the help of skilled healthcare providers is the best step towards managing the symptoms and complications of HPS effectively.
References
For additional information and to verify the details discussed regarding Hepatopulmonary Syndrome symptoms, we recommend consulting the following reputable sources. These references provide comprehensive insights and are instrumental in deepening understanding of this medical condition:
- National Institutes of Health (NIH) – This source offers a detailed exploration of Hepatopulmonary Syndrome, focusing on symptoms, diagnosis, and treatment options. Visit their page on Hepatopulmonary Syndrome here.
- Mayo Clinic – Known for its easy-to-understand patient education materials, the Mayo Clinic provides an overview of the symptoms associated with Hepatopulmonary Syndrome and discusses potential therapeutic approaches. Learn more by accessing their resource here.
- MedlinePlus – A service of the U.S. National Library of Medicine, MedlinePlus offers reliable information on Hepatopulmonary Syndrome, including symptoms and ongoing research. Check out their detailed page here.
- American Liver Foundation – This organization provides comprehensive information on various liver diseases, including Hepatopulmonary Syndrome. They offer resources that cover symptom management and treatment. Visit their website for more information here.
These resources are credible and valuable for anyone seeking further knowledge on Hepatopulmonary Syndrome, enhancing both understanding and awareness of this complex medical condition.