Hepatopulmonary Syndrome Treatment: Hepatopulmonary Syndrome (HPS) is a complex medical condition that arises as a complication of liver disease and is characterized by the presence of liver dysfunction and abnormalities in the pulmonary gas exchange.
This syndrome significantly impacts the quality of life and the prognosis for patients with liver diseases, making timely diagnosis and effective treatment crucial for improving outcomes.
Understanding Hepatopulmonary Syndrome
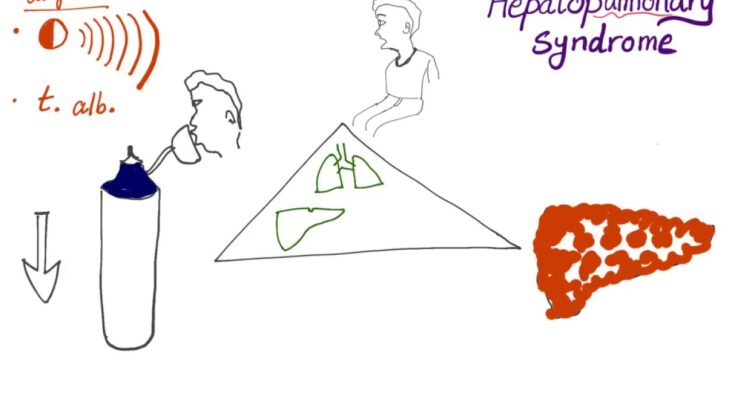
Hepatopulmonary Syndrome (HPS) is a complex medical condition that arises as a complication of liver disease. It primarily affects the lungs and the ability to oxygenate blood. As liver function deteriorates, blood vessels in the lungs may dilate abnormally, leading to decreased oxygen levels in the bloodstream. Understanding the epidemiology, risk factors, and key symptoms of HPS is crucial for early diagnosis and management.
Epidemiology: Who is Most at Risk?
Hepatopulmonary Syndrome is predominantly seen in individuals with chronic liver disease or cirrhosis. Although HPS can occur at any stage of liver disease, it is more frequent in the advanced stages. Studies indicate that HPS affects between 10% to 32% of patients with cirrhosis, making regular screening important for these patients. The risk is not confined to a specific type of liver disease, as HPS has been observed in various underlying conditions such as alcoholic liver disease, viral hepatitis, and nonalcoholic fatty liver disease.
Key Symptoms and Signs to Watch For
The symptoms of Hepatopulmonary Syndrome may vary and often worsen with the progression of liver disease. Common signs include:
- Shortness of Breath (Dyspnea): This occurs mainly during physical activity but can also be noticeable when at rest in more severe cases.
- Platypnea: This is a rare symptom characterized by increased shortness of breath while sitting up, which improves when lying down.
- Cyanosis: A bluish discoloration of the skin, especially the lips and fingertips, indicating low oxygen levels in the blood.
- Spider Angiomas: These are small, spider-like blood vessels visible on the skin, commonly associated with liver disease.
- Digital Clubbing: Swelling of the tips of the fingers or toes and changes in the angle between the nails and the nail base.
For anyone with existing liver disease, noticing any of these symptoms warrants immediate medical consultation. Early detection and intervention can significantly impact the management of HPS and the overall prognosis of liver disease. Regular follow-ups with a healthcare provider specializing in liver health are essential for those at risk.
Diagnosis of Hepatopulmonary Syndrome
Initial Assessment and Medical History Relevance
The initial evaluation for Hepatopulmonary Syndrome (HPS) begins with a comprehensive assessment of the patient’s medical history and symptoms. This step is crucial as it helps clinicians identify any underlying liver disease, which is a key component of HPS. During this phase, healthcare providers look for signs of chronic liver disease or cirrhosis, and inquire about symptoms such as shortness of breath, cyanosis (bluish discoloration of the skin), and clubbing of the fingers, which are indicative of HPS.
Key Diagnostic Tests
Several diagnostic tests are essential in confirming a diagnosis of Hepatopulmonary Syndrome:
1. Blood Tests to Check Liver Function: These tests evaluate how well the liver is performing its normal functions. Abnormal results can indicate liver disease, which is associated with HPS.
2. Imaging Studies:
- Chest X-ray: Helps in assessing the lung’s structure and detecting any abnormalities.
- CT Scan: Provides a detailed image of the liver and lungs, aiding in the identification of complications related to liver diseases and abnormal lung vascularities that are characteristic of HPS.
3. Pulse Oximetry and Arterial Blood Gas Analysis: These tests measure the oxygen levels in the blood. In HPS, these levels are typically lower due to impaired oxygen exchange.
4. Contrast Echocardiography (Bubble Study): This specific test is critical for diagnosing HPS. It involves injecting a saline solution mixed with a small amount of air into a vein and observing its passage through the heart to detect abnormal blood flow between arteries and veins in the lungs, a hallmark of HPS.
The Role of Specialists in Diagnosing HPS
The diagnosis of Hepatopulmonary Syndrome often requires collaboration among specialists from multiple disciplines:
- Hepatologists or liver specialists, manage the underlying liver disease and coordinate care related to liver function.
- Pulmonologists focus on the respiratory aspects of HPS, managing symptoms such as shortness of breath and hypoxemia.
- Cardiologists, particularly those skilled in echocardiography, are crucial for conducting and interpreting results from bubble studies.
These specialists play a vital role in ensuring a comprehensive approach to diagnosis and management, maximizing the chances of a favorable outcome for patients with HPS. By utilizing a combination of detailed medical history, specific diagnostic tests, and specialist consultations, an accurate diagnosis of Hepatopulmonary Syndrome can be achieved, leading to appropriate management strategies.
Current Treatments for Hepatopulmonary Syndrome
Managing HPS effectively requires a comprehensive approach that includes both medical therapies and surgical interventions. Understanding the available treatments and their outcomes is crucial for both patients and healthcare providers.
Medical Therapies
Medical management of HPS primarily focuses on alleviating symptoms and improving oxygenation before more definitive treatments can be applied. Here are some of the common medical therapies used:
- Supplemental Oxygen: Providing supplemental oxygen is the first line of treatment to improve the arterial oxygenation levels in patients with HPS. This therapy helps reduce symptoms related to hypoxia, such as shortness of breath and increased heart rate.
- Pulmonary Vasodilators: Medications such as pentoxifylline, a phosphodiesterase inhibitor, have been used experimentally to decrease pulmonary vascular dilatation, although results have been variable. Other vasodilators like sildenafil, which is typically used to treat pulmonary hypertension, may also be employed to manage HPS.
- Garlic Extract: Although not widely adopted, some studies suggest that garlic extract, due to its anti-angiogenic properties, might reduce pulmonary vasodilation and improve gas exchange.
While these medical treatments can provide symptomatic relief and temporary improvement in oxygenation, they do not address the underlying liver disease and are generally considered palliative.
Surgical Interventions
Surgical treatment options provide a more definitive approach to managing HPS. The most prominent surgical intervention is liver transplantation:
- Liver Transplantation: Currently, liver transplantation is the only known cure for HPS. This surgery addresses the root cause of HPS by replacing the diseased liver with a healthy one from a donor. Studies have shown that post-transplant, the majority of patients experience a significant improvement in oxygenation and a reversal of pulmonary symptoms. The survival rate post-transplant is also notably higher for patients with HPS compared to those with severe liver disease without HPS.
- Pre-Transplant Interventions: In cases where transplantation is delayed, procedures such as transjugular intrahepatic portosystemic shunt (TIPS) may be used. This procedure reduces portal pressure and can ameliorate symptoms, but it does not cure HPS and is not suitable for all patients.
Effectiveness and Outcomes
The effectiveness of treatments for HPS varies. Supplemental oxygen and medications offer temporary relief, but they do not halt the progression of the disease. Liver transplantation, while effective, comes with its own set of challenges, including the risk of surgery and the need for lifelong immunosuppression. However, the outcomes following a liver transplant are generally positive, with improvements in gas exchange and quality of life.
However, while current medical therapies can manage symptoms and improve quality of life temporarily, liver transplantation remains the most effective treatment for reversing the pathophysiological changes of hepatopulmonary syndrome. Ongoing research and advancements in treatment options are essential for improving the long-term health outcomes for patients suffering from this complex syndrome.
Challenges in Treating Hepatopulmonary Syndrome
Hepatopulmonary Syndrome (HPS) presents unique challenges in medical treatment due to its complex nature and the interplay between liver disease and lung vascular abnormalities. Understanding these challenges is crucial for effective management and improving patient outcomes.
Common Challenges Faced During Treatment
- Diagnosis Difficulty: HPS can be hard to diagnose because its symptoms, such as shortness of breath and cyanosis, often overlap with other conditions associated with liver disease. Advanced imaging techniques and hypoxia assessments are required for accurate diagnosis.
- Diverse Severity Levels: The severity of HPS varies widely among patients. This variation complicates treatment decisions, as the approach must be tailored to the individual’s specific condition and degree of hypoxemia.
- Limited Treatment Options: Currently, there are limited therapeutic options specifically targeting the pathophysiology of HPS. Treatments are often focused on managing symptoms rather than curing the underlying condition.
- Risk of Progression: Even with treatment, HPS can progress, leading to worsening gas exchange and hypoxia. This progression can complicate the management of liver disease and impact the timing and eligibility for liver transplantation.
Management of Complications
- Oxygen Therapy: Supplemental oxygen is used to manage hypoxemia, but it does not address the underlying pulmonary vascular dilations.
- Medications: While no medications are approved specifically for HPS, some drugs like pentoxifylline or anti-angiogenic agents have been studied for their potential benefits in improving pulmonary vascular complications.
- Liver Transplantation: This is considered the most effective treatment for reversing HPS. However, assessing transplant eligibility and managing post-operative complications pose significant challenges.
- Monitoring and Supportive Care: Regular monitoring of lung and liver functions is essential, alongside supportive therapies to manage symptoms and improve quality of life.
Importance of a Multidisciplinary Approach
A multidisciplinary approach is essential in the treatment of HPS, involving hepatologists, pulmonologists, transplant surgeons, and other specialists. This team collaboration ensures:
- Comprehensive Assessment: Accurate assessment of both liver and lung functions to tailor treatment plans.
- Integrated Care: Coordinated management of liver disease and pulmonary symptoms, enhancing the effectiveness of treatment and patient compliance.
- Advanced Research and Treatment Options: Facilitation of access to clinical trials and new therapies that could potentially benefit patients with HPS.
Effective treatment of Hepatopulmonary Syndrome is a complex process that requires overcoming numerous challenges, managing complications meticulously, and utilizing a collaborative, multidisciplinary approach to provide optimal patient care.
Advances and Future Directions in Hepatopulmonary Syndrome Treatment
Recent Advancements in Treatment Options
The treatment landscape for Hepatopulmonary Syndrome (HPS) has seen significant progress in recent years. Innovative therapies and improved management techniques have enhanced the quality of life for patients suffering from this complex condition, which arises from liver disease and affects the lungs. A pivotal development has been the use of supplemental oxygen therapy, which has proven to alleviate symptoms and improve oxygenation in HPS patients. Additionally, the refinement of liver transplantation criteria has also marked a significant step forward. Liver transplantation is currently the only definitive treatment for HPS, and recent modifications in candidate selection have improved outcomes for patients with severe manifestations of the syndrome.
Ongoing Research and Clinical Trials
Research into HPS is dynamic, with multiple studies aiming to uncover the underlying mechanisms of the syndrome and develop more effective treatments. Ongoing clinical trials are focusing on various aspects of HPS, including the potential benefits of pharmacological treatments that can decrease pulmonary vasodilation, a key feature of HPS. Drugs such as pentoxifylline, which is known for its anti-inflammatory properties, are under investigation for their efficacy in improving lung function in HPS patients. Researchers are also exploring the role of endothelin receptor antagonists, which may help manage the pulmonary vascular aspects of the disease.
Potential Future Therapies Under Investigation
Looking ahead, the future of HPS treatment appears promising with several potential therapies under investigation. One area of interest is gene therapy, which aims to address the genetic factors contributing to the syndrome. Advances in molecular biology could lead to targeted therapies that specifically correct the abnormal signaling pathways involved in HPS. Additionally, the exploration of stem cell therapy offers a potential avenue for regenerating damaged liver tissue and subsequently reducing pulmonary complications. As research continues to evolve, these innovative approaches may provide groundbreaking solutions for managing and potentially curing Hepatopulmonary Syndrome.
The ongoing advancements in the understanding and treatment of Hepatopulmonary Syndrome highlight a hopeful trajectory toward more effective and targeted therapies. With continuous research and the development of new treatment protocols, the future for patients with HPS looks increasingly optimistic.
FAQs about Hepatopulmonary Syndrome Treatment
What is Hepatopulmonary Syndrome?
Hepatopulmonary Syndrome (HPS) is a medical condition that occurs when liver disease, such as cirrhosis, leads to lung-related complications, including abnormal oxygen exchange. It typically manifests with symptoms like shortness of breath and blue skin coloration (cyanosis), particularly when standing or sitting up.
How is Hepatopulmonary Syndrome diagnosed?
Diagnosing HPS involves a series of tests. A doctor will typically recommend a pulse oximetry test to check oxygen levels in the blood. If low levels are detected, further testing like arterial blood gas, contrast echocardiography, and possibly lung imaging studies might be conducted to confirm the diagnosis and assess the severity.
What are the current treatments for Hepatopulmonary Syndrome?
The treatment for HPS mainly focuses on managing the underlying liver condition. Oxygen therapy can be used to relieve symptoms, but the most definitive treatment is often a liver transplant. This approach addresses the root cause of the syndrome by replacing the damaged liver with a healthy one.
Can medications improve Hepatopulmonary Syndrome?
Currently, there are no specific medications approved to directly treat HPS. Treatment generally targets the underlying liver disease and symptom management. However, ongoing clinical trials and research are focused on finding effective pharmacological treatments for HPS.
Is a liver transplant always necessary for Hepatopulmonary Syndrome?
A liver transplant is considered the most effective treatment for reversing the effects of HPS, but it’s not suitable for everyone. The decision depends on various factors, including the severity of the liver disease, the patient’s overall health, and suitability for surgery. For patients who are not transplant candidates, managing symptoms and complications is the main approach.
How successful are liver transplants in treating Hepatopulmonary Syndrome?
Liver transplants have a high success rate in significantly improving or curing HPS. Many patients experience a substantial improvement in symptoms and lung function post-transplant. However, the success of the transplant largely depends on individual factors like the severity of the condition and the patient’s health at the time of the transplant.
Conclusion
Patient support and continuous care play vital roles in managing HPS. Given the complexity of the syndrome, patients require a comprehensive care approach involving specialists in hepatology, pulmonology, and often transplant surgery. Support groups and patient education also significantly contribute to better management outcomes by helping patients understand their condition and adhere to treatment protocols.
Furthermore, ongoing research is crucial for advancing our understanding of HPS. Enhancements in diagnostic techniques and treatment strategies can lead to better patient outcomes and potentially more curative approaches in the future. Encouraging the medical research community to focus on innovative therapies and interdisciplinary approaches could pave the way for significant breakthroughs in HPS treatment.
Continued efforts in research, patient care, and treatment optimization will undoubtedly improve the quality of life for individuals affected by Hepatopulmonary Syndrome and offer hope for more effective management of this challenging condition.
References
For further reading and to validate the information provided on Hepatopulmonary Syndrome (HPS) treatment, consider exploring the following reputable sources:
- National Institutes of Health (NIH) – This government website offers comprehensive details on Hepatopulmonary Syndrome, including symptoms, diagnosis, and treatment options. Visit their page on HPS here.
- American Liver Foundation – A leading advocate for liver health, the American Liver Foundation provides valuable resources and guidance on liver-related conditions, including Hepatopulmonary Syndrome. Find more about HPS treatment options here.
- Mayo Clinic – Known for its reliable and detailed patient care information, the Mayo Clinic offers an in-depth look at Hepatopulmonary Syndrome. Their resource can be accessed here.
- PubMed Central – An archive of biomedical and life sciences journal literature, PubMed Central provides a collection of peer-reviewed articles on Hepatopulmonary Syndrome that can be accessed here.
Each of these sources provides essential information that can help deepen your understanding of Hepatopulmonary Syndrome, its implications, and the latest treatment protocols.