Hepatocellular Carcinoma Symptoms: Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, which strikes predominantly those who suffer from chronic liver diseases, such as cirrhosis caused by hepatitis B or hepatitis C infection.
This in-depth article explores the critical symptoms and underlying causes of hepatocellular carcinoma, providing essential information for both patients and healthcare providers.
Understanding Hepatocellular Carcinoma (HCC)
Hepatocellular Carcinoma (HCC) is the most common type of primary liver cancer, which originates in the liver without spreading from another organ. This malignant condition arises from hepatocytes, the liver’s predominant cell type. HCC is known for its aggressive nature and poor prognosis if not detected early. Understanding its impact on liver functions and overall health is crucial for timely diagnosis and management.
Epidemiology of Hepatocellular Carcinoma
HCC holds a significant presence globally, particularly in regions where viral hepatitis B or C is prevalent. It ranks as the sixth most common cancer and the third leading cause of cancer-related deaths worldwide. The prevalence of HCC varies geographically, with the highest incidence rates observed in East Asia and sub-Saharan Africa due to the high prevalence of chronic hepatitis B infection in these areas.
Risk Factors Associated with HCC
The development of Hepatocellular Carcinoma is closely linked to several risk factors, including:
- Chronic Viral Hepatitis: Chronic infections with hepatitis B virus (HBV) or hepatitis C virus (HCV) are among the leading risk factors.
- Cirrhosis: Regardless of its cause, cirrhosis, or scarring of the liver tissue, increases the risk of HCC. Causes of cirrhosis include alcohol abuse, nonalcoholic fatty liver disease, and chronic hepatitis.
- Other Factors: These include age (risk increases with age), gender (more common in males), and environmental factors such as aflatoxin exposure.
How HCC Develops in the Liver
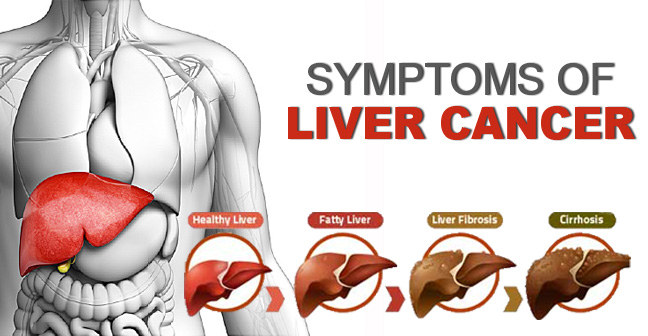
Hepatocellular carcinoma typically develops in the setting of chronic liver inflammation and damage. Over time, factors like hepatitis infection and cirrhosis lead to repeated cycles of liver cell injury and repair. This process can cause mutations in the DNA of liver cells. As these genetic changes accumulate, they can cause cells to grow uncontrollably and form a tumor. Most often, HCC is diagnosed in patients who have been suffering from chronic liver conditions for many years, highlighting the importance of liver health monitoring and early intervention in at-risk populations.
However, understanding Hepatocellular Carcinoma is vital for early detection and effective treatment strategies. By recognizing the risk factors and knowing the developmental process of HCC, individuals and healthcare providers can better manage and potentially prevent this serious condition.
Symptoms of Hepatocellular Carcinoma (HCC)
Here, we explore both the early and advanced symptoms of HCC, and discuss how these symptoms can differ among patients.
Early Symptoms of Hepatocellular Carcinoma
In its early stages, hepatocellular carcinoma might not present any noticeable symptoms, which can make early detection challenging. However, some individuals may experience subtle signs that should not be overlooked:
- Fatigue: This is one of the most common early symptoms, where the patient feels unusually tired.
- Mild abdominal pain or discomfort: Often localized on the right side of the abdomen.
- Unexplained weight loss: Losing weight without trying can be a sign of various conditions, including HCC.
- Loss of appetite: A decrease in the desire to eat, sometimes accompanied by nausea.
- General weakness: A pervasive feeling of weakness that is not related to physical exertion.
These symptoms are often nonspecific and can be mistaken for less serious conditions. It is crucial for individuals experiencing these symptoms persistently to consult a healthcare provider.
Advanced Symptoms of Hepatocellular Carcinoma
As the cancer progresses, the symptoms of HCC become more pronounced and severe:
- Jaundice: Yellowing of the skin and the whites of the eyes, resulting from the liver’s inability to process bilirubin.
- Ascites: Accumulation of fluid in the abdomen, causing swelling and increased abdominal girth.
- Severe abdominal pain: As the tumor grows, it can cause more significant pain and discomfort.
- Enlarged liver or spleen: Felt as a mass under the ribs on the right side.
- Easy bruising or bleeding: The liver’s impaired ability to produce blood clotting factors can lead to this symptom.
Variability of Symptoms Among Different Patients
The symptoms of hepatocellular carcinoma can vary widely among individuals. Factors such as the underlying cause of the liver cancer, the stage of the cancer, the patient’s overall health, and their liver function can all influence the type and severity of symptoms experienced. For instance, patients with underlying liver conditions like hepatitis or cirrhosis may experience different or more severe symptoms earlier in the disease process.
Some patients might show symptoms that are less common, such as a fever or a marked change in their blood sugar levels. Due to this variability, medical evaluations often include a range of tests to accurately diagnose and assess the extent of the disease.
However, understanding the potential symptoms of hepatocellular carcinoma is essential for at-risk individuals and for those who may be experiencing signs of liver issues. Early medical intervention is crucial in managing the disease effectively and can significantly improve the prognosis. If you or someone you know is experiencing any of these symptoms, it is important to seek professional medical advice.
Major Causes of Hepatocellular Carcinoma
Understanding the major causes and risk factors associated with HCC is crucial for early detection and effective management. Here, we delve into the primary contributors to the development of HCC, offering insights into how each factor plays a role in the progression of this serious disease.
Chronic Hepatitis B and C Infections
Chronic infections with hepatitis B virus (HBV) or hepatitis C virus (HCV) are among the leading causes of hepatocellular carcinoma. These viral infections can lead to long-term liver inflammation, which over time, causes severe liver damage and increases the risk of developing HCC. Globally, a substantial number of HCC cases are linked to HBV or HCV, emphasizing the importance of vaccination, early diagnosis, and effective treatment of these viral infections.
Cirrhosis from Alcohol Abuse and Other Causes
Cirrhosis, a condition characterized by progressive liver scarring, is another significant risk factor for HCC. While cirrhosis can result from chronic viral hepatitis, alcohol abuse is also a major contributor. Prolonged alcohol consumption can lead to alcoholic liver disease, which often progresses to cirrhosis. The damaged liver tissue becomes a fertile ground for the development of cancer cells, leading to HCC.
Other Risk Factors
Aflatoxin Exposure
Aflatoxins are toxic substances produced by certain types of mold, which can contaminate stored grains and nuts under specific conditions. Regular exposure to aflatoxins is a known risk factor for HCC, particularly in regions with insufficient food storage and safety measures. Aflatoxins induce genetic mutations in liver cells, thereby increasing the risk of cancer.
Nonalcoholic Fatty Liver Disease (NAFLD)
With rising obesity rates, NAFLD has become increasingly common and is now recognized as a significant risk factor for HCC. NAFLD can progress to nonalcoholic steatohepatitis (NASH), a more severe form of liver disease characterized by inflammation and liver cell damage, which can eventually lead to HCC.
Genetic Predispositions
Genetics also play a role in the susceptibility to HCC. Certain genetic conditions, such as hemochromatosis and alpha-1 antitrypsin deficiency, increase the risk of liver cirrhosis and subsequent hepatocellular carcinoma. Identifying genetic risks early can help in monitoring and managing potential progression to HCC.
However, understanding these causes not only helps in early detection and prevention but also underscores the importance of comprehensive liver health management and regular medical screenings. By addressing these risk factors proactively, individuals can significantly reduce their risk of developing HCC.
Diagnosis and Detection of Hepatocellular Carcinoma Symptoms
Early detection of HCC is crucial as it significantly enhances the effectiveness of treatment options, potentially leading to better survival rates and improved quality of life. This section explores the importance of timely diagnosis, outlines common diagnostic tools, and emphasizes the need for regular screening in high-risk groups.
Importance of Early Detection in Improving Treatment Outcomes
Detecting HCC at an early stage is paramount. The liver is a vital organ that supports nearly every other organ in the body in some capacity. Early-stage liver cancer does not usually present clear symptoms, making early detection challenging yet all the more vital. When diagnosed early, treatment options such as surgical resection, liver transplantation, and minimally invasive procedures like radiofrequency ablation are more feasible and can be highly effective. Early detection not only increases the likelihood of a complete cure but also significantly reduces the risk of serious complications associated with advanced liver cancer.
Common Diagnostic Tools and Tests for Hepatocellular Carcinoma
Several diagnostic tools and tests are pivotal in identifying HCC:
- Imaging Tests: Techniques such as ultrasound, computed tomography (CT) scans, and magnetic resonance imaging (MRI) are commonly used. These imaging tools can detect liver abnormalities and are instrumental in monitoring the progression of liver diseases that could lead to HCC.
- Alpha-fetoprotein (AFP) Test: Although not exclusively specific to HCC, elevated levels of AFP in the blood can suggest the presence of liver cancer, particularly in at-risk populations.
- Liver Biopsy: This is the most definitive method for diagnosing HCC. A small sample of liver tissue is collected using a needle inserted through the skin into the liver and examined under a microscope to identify cancerous cells.
- Blood Tests: Tests that evaluate liver function can provide indirect evidence of liver abnormalities, potentially pointing to HCC.
The Role of Regular Screening for High-Risk Individuals
Regular screening is critical for individuals at high risk of developing HCC. This group includes people with chronic hepatitis B or C, those with a history of alcohol abuse, patients with cirrhosis, and individuals with a family history of liver cancer. Regular screening involves periodic imaging tests and blood tests to monitor liver health and function. This proactive approach allows for the early detection of liver cancer, even before symptoms develop, thereby facilitating early and potentially more effective treatment.
However, understanding and utilizing the appropriate diagnostic tools and engaging in regular screening if at high risk are key strategies in the fight against hepatocellular carcinoma. These measures are instrumental in catching the disease in its earliest stages, which is often when treatment can be most successful.
Treatment Options for Hepatocellular Carcinoma
Due to the complexity of this condition, various treatment strategies are adopted based on the stage of the cancer, the patient’s overall health, and specific liver function. Below, we explore both surgical and non-surgical treatments available for HCC and discuss the critical importance of a personalized treatment plan.
Surgical Options
Surgery remains a cornerstone in the treatment of hepatocellular carcinoma, particularly for patients diagnosed at an early stage where the tumor is localized. Here are the primary surgical treatments:
- Partial Hepatectomy: This procedure involves the removal of the part of the liver that contains cancer. It’s suitable for patients with sufficient liver function and who do not have advanced cirrhosis.
- Liver Transplantation: For patients with advanced liver disease or those who have tumors that cannot be removed with surgery due to their location or size, liver transplantation might be an option. This involves replacing the liver with a healthy one from a donor. Candidates for this treatment must meet specific criteria to ensure the best outcomes.
Non-Surgical Treatments
Non-surgical options play a pivotal role, especially for those who cannot undergo surgery. These treatments include:
- Radiofrequency Ablation (RFA): RFA uses high-frequency radio waves to generate heat that destroys cancer cells. It’s most effective for small tumors.
- Transarterial Chemoembolization (TACE): This procedure delivers chemotherapy directly to the liver while blocking the artery that feeds the tumor, effectively starving and killing the cancer cells.
- Targeted Therapy and Immunotherapy: These treatments use medications that target specific pathways that cancer cells use to grow and spread. Immunotherapy helps to boost the body’s immune system to fight the cancer more effectively.
- Radiation Therapy: Advanced techniques like stereotactic body radiation therapy (SBRT) can deliver high doses of radiation precisely to the tumor, minimizing damage to surrounding healthy tissues.
The Importance of a Personalized Treatment Plan
Each case of hepatocellular carcinoma is unique, and therefore, a personalized treatment plan is crucial. The choice of treatment depends on various factors, including the number and size of tumors, liver function status, presence of cirrhosis, and overall health conditions. A multidisciplinary team of specialists—including hepatologists, oncologists, radiologists, and surgeons—works together to tailor the treatment approach to the individual’s specific clinical needs.
Creating a personalized plan ensures that the treatment is not only effective but also aligns with the patient’s lifestyle, preferences, and long-term health goals. This approach helps in managing side effects and improves the overall quality of life and survival rates.
However, treating hepatocellular carcinoma effectively involves a combination of multiple strategies, tailored to the patient’s specific condition. Whether through surgery, innovative non-surgical methods, or a mix of both, the focus is always on providing care that is best suited to the patient’s unique health profile.
FAQs about Hepatocellular Carcinoma Symptoms
What are the early symptoms of hepatocellular carcinoma?
Early symptoms of hepatocellular carcinoma (HCC) are often subtle and may be easily overlooked. Common early indicators include unexplained weight loss, a general feeling of fatigue, and a mild discomfort in the upper abdomen. Regular monitoring and medical check-ups are crucial for early detection, especially for individuals at higher risk.
Can hepatocellular carcinoma cause pain?
Yes, as hepatocellular carcinoma progresses, it can cause pain, particularly in the upper right quadrant of the abdomen. This pain may result from the tumor stretching the liver’s capsule or from the tumor invading nearby structures. Persistent or severe abdominal pain should be evaluated by a healthcare provider.
Are there any visible signs of hepatocellular carcinoma?
Visible signs of hepatocellular carcinoma can include jaundice, which is a yellowing of the skin and eyes caused by the liver’s inability to properly process bilirubin. Additionally, swelling in the abdomen due to fluid accumulation (ascites) may also be noticeable as the disease progresses. These symptoms warrant immediate medical attention.
How does hepatocellular carcinoma affect overall health?
Hepatocellular carcinoma can significantly impact overall health, leading to progressive liver dysfunction. This dysfunction can manifest as easy bruising or bleeding, intense itching, and muscle wasting. As liver function declines, complications like hepatic encephalopathy, which affects brain function, can also develop.
What should I do if I suspect symptoms of hepatocellular carcinoma?
If you suspect you are experiencing symptoms of hepatocellular carcinoma, it is essential to consult a healthcare provider immediately. Early diagnosis and treatment are pivotal for improving prognosis and managing the effects of the disease. Be proactive in discussing any concerning symptoms with your doctor, especially if you have underlying liver conditions or a family history of liver cancer.
Conclusion
Hepatocellular carcinoma (HCC) is a primary liver cancer that poses significant health challenges globally. Key symptoms of HCC include unintentional weight loss, loss of appetite, upper abdominal pain, nausea, and jaundice. The causes of this disease are well-identified and include chronic infection with hepatitis B or C, long-term alcohol consumption, non-alcoholic fatty liver disease, and exposure to aflatoxins.
Early detection and management are crucial in improving the prognosis of HCC. Individuals who are at risk, especially those with known liver disease or a family history of liver cancer, should prioritize regular medical evaluations. If you or someone you know falls into these risk categories, it is advisable to consult with a healthcare provider for ongoing monitoring and appropriate diagnostic tests. Regular check-ups can lead to early detection, which significantly enhances treatment effectiveness and can improve outcomes.
Taking proactive steps in managing your health is the best strategy against hepatocellular carcinoma. Stay informed, stay vigilant, and seek professional medical advice regularly.
References
For those seeking additional information or verification of the details shared about the symptoms of Hepatocellular Carcinoma, here is a list of credible sources:
- National Cancer Institute – Provides comprehensive information on Hepatocellular Carcinoma, including symptoms, diagnosis, and treatment options. Read more about Hepatocellular Carcinoma Symptoms at the National Cancer Institute.
- Mayo Clinic – Offers detailed insights into the signs, symptoms, and causes of Hepatocellular Carcinoma. A trusted resource for patient education. Explore Hepatocellular Carcinoma Symptoms on Mayo Clinic.
- American Cancer Society – Provides statistics, treatment options, and research news about Hepatocellular Carcinoma. A valuable resource for both patients and healthcare professionals. Visit the American Cancer Society for more information on Hepatocellular Carcinoma.
These resources are reliable and can be used to deepen your understanding of Hepatocellular Carcinoma and its symptoms. They are recognized for their commitment to providing up-to-date and scientifically accurate health information.