Hepatocellular Carcinoma Treatment: Hepatocellular Carcinoma (HCC) is the most common type of primary liver cancer, predominantly affecting individuals with chronic liver diseases such as hepatitis B, hepatitis C, and cirrhosis.
The complexity of HCC and its underlying causes necessitate a sophisticated approach to diagnosis and treatment.
Understanding Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, primarily affecting adults. It ranks as the sixth most prevalent cancer and the third leading cause of cancer-related deaths worldwide. This cancer originates in the hepatocytes, the liver’s main type of cell, and is often diagnosed in individuals who have chronic liver diseases, such as cirrhosis or hepatitis.
Risk Factors Contributing to the Development of HCC
Several risk factors increase the likelihood of developing hepatocellular carcinoma:
- Chronic viral hepatitis: Hepatitis B and C are among the leading causes of HCC worldwide.
- Cirrhosis: Any form of cirrhosis, whether caused by alcohol, non-alcoholic fatty liver disease, or chronic hepatitis, significantly increases HCC risk.
- Lifestyle factors: Chronic alcohol abuse, smoking, and obesity are notable risk factors.
- Genetic predispositions: Certain genetic disorders like hemochromatosis and alpha-1 antitrypsin deficiency increase the risk.
- Environmental toxins: Exposure to aflatoxins, which are produced by fungi on stored agricultural products, and other industrial chemicals can contribute to HCC development.
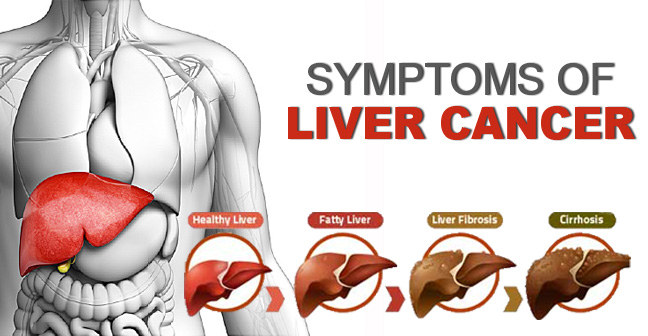
Pathophysiology: How Hepatocellular Carcinoma Develops
The development of hepatocellular carcinoma is a complex process involving multiple steps and pathways. It typically progresses over many years and is often preceded by liver damage and inflammation which lead to cirrhosis. The pathogenesis of HCC involves the accumulation of genetic mutations and epigenetic alterations that disrupt cellular processes such as DNA repair, cell cycle regulation, and apoptosis (programmed cell death).
Chronic inflammation from hepatitis infections or toxic substances leads to cellular damage and increased cellular turnover. Over time, this creates a favorable environment for genetic mutations and malignant transformation. The liver’s regenerative capacity, which normally helps maintain liver function, can instead facilitate the expansion of malignant cells, allowing the cancer to progress and eventually spread to other parts of the body.
However, understanding the multifaceted nature of hepatocellular carcinoma’s development, risk factors, and prevalence is crucial for effective prevention, early detection, and targeted treatment strategies.
Signs and Symptoms of Hepatocellular Carcinoma
Recognizing these symptoms early can significantly influence the urgency and approach to treatment. Here, we discuss the common symptoms associated with both early and advanced stages of HCC, and how these symptoms guide medical interventions.
Symptoms in Early Stages
In the early stages, hepatocellular carcinoma might not present any noticeable symptoms. However, as the tumor grows, subtle signs can begin to manifest. Common early symptoms include:
- Unexplained weight loss: Losing weight without changes in diet or exercise routine can be an early indicator.
- Loss of appetite: Feeling less hungry than usual over a period of time.
- Mild abdominal pain: Discomfort or pain in the upper right quadrant of the abdomen.
- General weakness and fatigue: Feeling unusually tired can be one of the nonspecific early signs.
- Slight jaundice: Early stages of jaundice might include slightly yellow eyes and skin.
Detecting HCC at this stage can be challenging due to the vague nature of the symptoms, which often resemble less serious conditions.
Symptoms in Advanced Stages
As the cancer progresses to more advanced stages, the symptoms become more pronounced and severe. These include:
- Increased abdominal pain: Pain may become more persistent and localized as the tumor enlarges.
- Noticeable jaundice: More evident yellowing of the skin and eyes.
- Ascites: Accumulation of fluid in the abdomen, leading to swelling.
- Easy bruising or bleeding: Liver dysfunction can interfere with blood clotting.
- Enlarged liver or spleen: Felt as a mass under the ribs on the right side.
- Vomiting and nausea: These symptoms can become more frequent as the disease progresses.
How Symptoms Influence Treatment Urgency and Approach
The presence and severity of symptoms play a crucial role in determining the urgency and specifics of treatment for hepatocellular carcinoma. Early detection, often facilitated by vigilant observation of the initial subtle symptoms, can lead to more effective management options, such as surgical resection or localized treatments like radiofrequency ablation.
In advanced stages, where symptoms are more severe and the cancer may have spread, treatment focuses on palliative care to relieve symptoms and improve quality of life. Systemic therapies, including chemotherapy and targeted therapies, might be considered to manage the disease.
Diagnostic Approaches for Hepatocellular Carcinoma
Effective management of HCC relies on timely and accurate diagnosis. This article delves into the various diagnostic strategies, emphasizing screening methods for at-risk populations, imaging techniques, and the essential role of biopsy and laboratory tests in confirming the diagnosis.
Screening Methods for At-Risk Populations
Screening for HCC is crucial in individuals with a high risk of developing the condition, such as those with cirrhosis or chronic hepatitis B and C. Regular screening helps in early detection, potentially improving treatment outcomes and survival rates. The recommended screening protocol typically involves an ultrasound every six months. Alpha-fetoprotein (AFP) testing, a blood test used to detect a particular protein, may also complement ultrasound screenings, although its sensitivity varies.
Imaging Techniques Used in the Diagnosis
Imaging techniques play a pivotal role in the diagnosis of hepatocellular carcinoma. These non-invasive methods provide detailed visuals of the liver, helping in identifying and characterizing any lesions. Key imaging modalities include:
- Ultrasound: Often the first step in screening, ultrasound can detect liver tumors early, especially in cirrhotic livers. It is affordable and readily available.
- Computed Tomography (CT) Scan: CT scans offer a more detailed view, showing the size, shape, and exact location of the tumors. They are particularly useful in staging the cancer and planning treatment.
- Magnetic Resonance Imaging (MRI): MRI is highly effective for differentiating benign from malignant liver lesions and is superior in assessing the vascular anatomy of the liver. It uses magnetic fields and radio waves to produce high-resolution images.
Role of Biopsy and Other Laboratory Tests in Confirming HCC
While imaging tests provide crucial information, a biopsy is often necessary to confirm the diagnosis of HCC. During a biopsy, a small sample of liver tissue is removed using a needle guided by ultrasound or CT scan and examined microscopically. Biopsies can confirm the presence of cancer cells and help distinguish HCC from other types of liver tumors.
Other laboratory tests can also support the diagnosis or provide additional information about the patient’s liver health and function, including liver function tests, serum albumin levels, and bilirubin levels. These tests are essential for planning the appropriate management and therapeutic approach.
However, the diagnostic process for hepatocellular carcinoma involves a combination of screening in at-risk populations, detailed imaging studies, and confirmatory biopsy along with other laboratory tests. Early and accurate diagnosis through these methods is critical in managing HCC effectively and improving patient outcomes.
Current Treatment Options for Hepatocellular Carcinoma
Below, we explore the various treatment modalities currently available for HCC, highlighting the importance of personalized treatment plans.
Surgical Treatments: Resection and Liver Transplant Options
Surgical interventions are often considered for patients with HCC, particularly those with localized disease and good liver function. The two primary surgical options include:
- Liver Resection: This involves the surgical removal of the tumor along with a margin of healthy tissue. Resection is typically reserved for patients who have sufficient liver reserve and no significant portal hypertension or extrahepatic disease.
- Liver Transplant: For patients with advanced liver disease or those who have tumors that cannot be completely removed by resection, a liver transplant may be the best option. Transplants provide the benefit of removing the entire liver, thus eliminating all tumor sites, and curing the underlying liver disease.
Local Therapies: Ablation and Embolization Techniques
Local therapies are crucial for patients who may not be suitable candidates for surgery. These treatments target the tumor directly, minimizing damage to the surrounding healthy liver tissue:
- Ablation: Techniques such as radiofrequency ablation (RFA) or microwave ablation (MWA) use heat to destroy cancer cells. Ablation is most effective for small tumors and can be performed percutaneously, thereby reducing recovery time and complications.
- Embolization Techniques: These include transarterial chemoembolization (TACE) and radioembolization (Y90). These procedures involve the delivery of chemotherapy drugs or radioactive particles directly into the liver’s blood supply feeding the tumor, effectively starving it of nutrients and leading to tumor cell death.
Systemic Treatments
When HCC has spread beyond the liver or when local treatments are not feasible, systemic treatments are considered:
- Chemotherapy: While less commonly used for HCC due to its limited effectiveness and considerable side effects, chemotherapy can still be part of a treatment plan, particularly in combination therapies.
- Targeted Therapy: Drugs such as sorafenib, which targets specific pathways that cancer cells use to grow, can help control tumor growth and spread. These medications are usually recommended for advanced HCC.
- Immunotherapy: This treatment leverages the body’s immune system to fight cancer. Drugs like nivolumab and pembrolizumab have shown promise in improving survival rates in HCC patients, especially those who have not responded to other treatments.
Importance of Personalized Treatment Plans
Given the complexity and variability of HCC, personalized treatment plans are essential. These plans are based on several factors, including the stage of the cancer, liver function, overall health, and personal preferences of the patient. A multidisciplinary team approach involving hepatologists, oncologists, radiologists, and surgeons is crucial to devise the most effective treatment strategy, aiming not just for survival, but also for quality of life.
However, the management of hepatocellular carcinoma is multifaceted and evolving. Continuous research and advances in treatment options offer hope and improved outcomes for patients battling this challenging disease.
Advances in Hepatocellular Carcinoma Treatment
Hepatocellular carcinoma (HCC) remains one of the most prevalent and challenging cancers to treat. However, recent advances in treatment and ongoing research offer new hope. This article explores the latest research, the importance of clinical trials, and the emerging role of precision medicine in combating HCC.
Latest Research and Emerging Therapies
Recent years have seen significant strides in understanding and treating HCC. Emerging therapies that are currently under research include targeted therapy drugs that focus on specific aspects of cancer cells to inhibit their growth. For instance, new kinase inhibitors and immune checkpoint inhibitors are showing promising results in early trials, offering more effective and less toxic treatment options than traditional chemotherapy.
Clinical Trials and Their Significance in Advancing Treatment Options
Clinical trials play a pivotal role in the advancement of HCC treatments. These trials are essential for testing the safety and efficacy of new treatments. They also provide insights into various aspects of the disease, helping to refine existing therapies and develop new intervention strategies. Participation in clinical trials not only helps in advancing medical research but also offers patients access to cutting-edge treatments that are not yet widely available.
The Role of Precision Medicine in HCC Treatment
Precision medicine is revolutionizing the treatment landscape for hepatocellular carcinoma. This approach tailors treatment to individual patients based on their genetic makeup, lifestyle, and environment. Advances in genetic testing have enabled doctors to identify specific mutations in HCC tumors, leading to more personalized and effective treatment plans. For example, therapies that target specific genetic alterations in tumor cells can potentially lead to better outcomes and fewer side effects compared to one-size-fits-all approaches.
However, the treatment of hepatocellular carcinoma is evolving rapidly, thanks to the relentless pursuit of innovation in medical research. With ongoing advancements in emerging therapies, the significance of clinical trials, and the integration of precision medicine, the future of HCC treatment looks promising. These developments not only aim to extend survival but also improve the quality of life for those affected by this challenging disease.
Managing Hepatocellular Carcinoma
Effective management encompasses follow-up care and monitoring, lifestyle adjustments, and a robust support system to handle both physical and emotional challenges. Here’s a detailed guide on navigating these aspects to optimize patient outcomes and enhance quality of life.
Follow-Up Care and Monitoring
Regular follow-up care is crucial for managing hepatocellular carcinoma, aiming to monitor the progress of the disease, assess the effectiveness of treatments, and catch any recurrence early. The components of follow-up care typically include:
- Regular Imaging Tests: Patients often undergo imaging tests such as ultrasound, CT scans, or MRIs every 3-6 months to monitor tumor status and liver health.
- Blood Tests: Blood tests measuring liver function and tumor markers (like alpha-fetoprotein, or AFP) help in assessing the disease’s progression and response to treatment.
- Physical Examinations: Routine check-ups involve thorough physical exams to evaluate overall health and detect any signs of cancer recurrence or treatment side effects.
- Multidisciplinary Consultations: Regular consultations with a hepatologist, oncologist, and other specialists ensure a coordinated approach to treatment and management of the condition.
Lifestyle Changes and Supportive Care
Managing symptoms of hepatocellular carcinoma and improving quality of life can also involve significant lifestyle changes and supportive care measures:
- Nutritional Support: A balanced diet tailored to individual needs can help maintain strength and body weight. A nutritionist can offer guidance on healthy eating habits, especially if liver function is compromised.
- Exercise: Regular, gentle exercise such as walking or yoga can improve physical function and combat fatigue. It’s important to tailor the intensity based on individual energy levels and overall health.
- Managing Side Effects: Addressing common side effects of treatment like nausea, pain, and fatigue through appropriate medications and therapies is essential.
- Avoiding Alcohol and Toxins: Alcohol can exacerbate liver damage, hence abstaining from it is crucial. Additionally, avoiding environmental toxins, such as certain chemicals and pollutants, protects liver health.
Importance of Mental and Emotional Support
The diagnosis of hepatocellular carcinoma can be overwhelmingly distressing for patients and their families. Ensuring robust mental and emotional support is pivotal:
- Support Groups: Joining support groups where patients share experiences and coping strategies can provide comfort and reduce feelings of isolation.
- Psychological Counseling: Professional counselors or psychologists can help patients and families deal with the psychological and emotional impacts of cancer diagnosis and treatment.
- Family and Social Support: Strong support from family and friends provides emotional stability and practical help during treatment.
- Stress Management Techniques: Techniques such as meditation, mindfulness, and relaxation exercises can help manage anxiety and improve overall mental well-being.
Adopting a comprehensive approach that combines diligent medical follow-up, lifestyle adjustments, and strong emotional support can significantly help manage hepatocellular carcinoma, ensuring patients not only survive but thrive during and after treatment.
FAQs about Hepatocellular Carcinoma Treatment
What are the main treatment options for Hepatocellular Carcinoma (HCC)?
The primary treatments for Hepatocellular Carcinoma include surgery (resection and liver transplant), local therapies like ablation and embolization, targeted therapy, immunotherapy, and radiation therapy. The choice of treatment depends on the stage of the cancer, the liver’s function, overall health, and personal preferences.
Is surgery always an option for HCC patients?
Surgery is not suitable for all HCC patients. It’s typically reserved for those who have a single tumor or a few small tumors and do not have advanced liver disease such as cirrhosis. A liver transplant may be considered if the liver is severely damaged.
What is targeted therapy, and how does it work for HCC?
Targeted therapy involves drugs that specifically target certain pathways or abnormalities in cancer cells. For HCC, drugs like sorafenib or lenvatinib might be used to help slow the growth of the tumor and are often used when surgery is not an option.
Can HCC be cured?
Curing HCC can be challenging, especially if diagnosed at an advanced stage. Early-stage HCC, when amenable to treatments like surgery or liver transplant, can sometimes be cured. In more advanced cases, treatment focuses on slowing the growth of the cancer and alleviating symptoms to improve quality of life.
What are the side effects of HCC treatments?
The side effects depend on the type of treatment. Surgical treatments can lead to complications such as infections and bleeding. Ablation therapies might cause pain and fever. Targeted therapies and immunotherapies can cause skin rash, fatigue, and gastrointestinal symptoms. Discuss with your healthcare provider about managing these side effects.
How often should someone with HCC be monitored during treatment?
Monitoring during HCC treatment typically includes regular imaging tests like CT scans or MRIs and blood tests to measure liver function and tumor markers. The frequency of these tests will depend on the type of treatment, the stage of cancer, and the individual’s overall health.
Are there new treatments being developed for HCC?
Yes, research is ongoing to find more effective treatments for HCC. Recent developments include new targeted therapies, advanced immunotherapies, and combinations of different treatment modalities to improve outcomes. Clinical trials may also be an option for accessing cutting-edge treatments.
Conclusion
In conclusion, the importance of early diagnosis and the development of innovative treatments for Hepatocellular Carcinoma (HCC) cannot be overstated. Early detection of HCC significantly enhances the effectiveness of treatments and improves survival rates. Innovations in treatment, including targeted therapies and advanced surgical techniques, are creating more options for patients, leading to better outcomes and quality of life.
Looking ahead, the future of HCC treatments appears promising. Ongoing research is focused on understanding the molecular and genetic mechanisms of the disease, which is expected to lead to more personalized and precise treatment strategies. Additionally, the integration of technology, such as artificial intelligence and machine learning, into diagnostic and treatment processes holds the potential to revolutionize the management of HCC. These advancements suggest a hopeful horizon for individuals affected by Hepatocellular Carcinoma, with the goal of achieving higher recovery rates and ultimately, a decrease in mortality associated with the disease.
References
For those seeking additional information or verification of the details discussed regarding the treatment of Hepatocellular Carcinoma (HCC), the following reputable sources are recommended. These links lead to reliable resources that can enhance understanding and provide deeper insights into various treatment options and advancements in HCC management.
- National Cancer Institute: This comprehensive resource offers detailed information on Hepatocellular Carcinoma including treatment options, clinical trials, and research developments. Visit National Cancer Institute for HCC
- Mayo Clinic: Renowned for its patient care and research, the Mayo Clinic provides an overview of diagnosis, treatment procedures, and ongoing care for Hepatocellular Carcinoma. Explore Mayo Clinic’s HCC Guide
- American Cancer Society: Useful for both patients and healthcare professionals, this site includes information on symptoms, causes, risk factors, and detailed treatment methods for Hepatocellular Carcinoma. Read more at American Cancer Society
These sources are maintained by well-regarded institutions that specialize in oncology and hepatology, making them excellent references for reliable and up-to-date information on Hepatocellular Carcinoma treatment.