Hepatitis E Treatment: Hepatitis E is a viral infection that primarily affects the liver, leading to inflammation and potentially severe complications.
It is caused by the Hepatitis E virus (HEV) and is predominantly transmitted through the consumption of contaminated water.
This article aims to provide a comprehensive guide on the diagnosis and treatment of Hepatitis E, underscoring the importance of early detection and effective medical interventions.
Understanding Hepatitis E
Hepatitis E is a liver infection caused by the Hepatitis E virus (HEV). It is a significant global health concern due to its potential severity and widespread prevalence. This article provides a detailed overview of how Hepatitis E is transmitted, the risk factors associated with the disease, its symptoms, and the demographics most affected by it.
Transmission Methods and Risk Factors
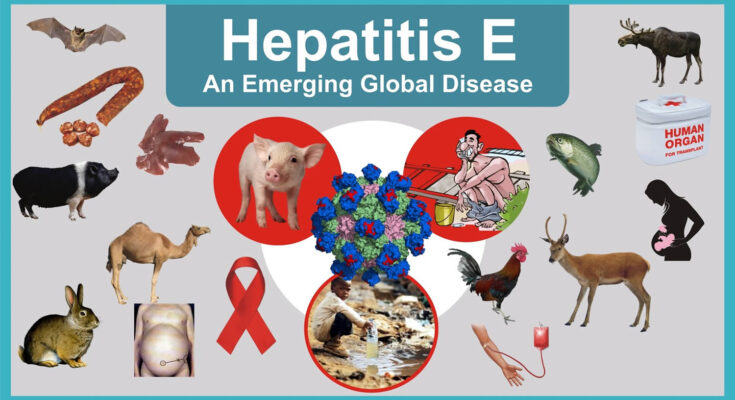
Hepatitis E is primarily transmitted through the fecal-oral route. This can occur through the consumption of contaminated water or food. In areas with poor sanitation, this is the most common mode of transmission. Other less common ways include:
- Person-to-person contact: Although rare, the virus can spread from one person to another, especially in close living conditions where personal hygiene might be compromised.
- Consuming raw or undercooked meat: Eating undercooked pork or deer meat has been linked to cases of Hepatitis E, particularly in developed countries.
- Blood transfusion and organ transplants: In rare cases, the virus has been transmitted through blood transfusions and organ transplants from infected donors.
Risk factors include:
- Traveling to or living in areas with poor sanitation: Travelers to regions with high rates of Hepatitis E, such as parts of Asia, Africa, and Mexico, are at increased risk.
- Poor personal hygiene and sanitation: Lack of proper sanitation and poor personal hygiene increase the risk of HEV infection.
- Consumption of raw or undercooked meat: Particularly pork and venison.
- Pregnancy: Pregnant women are at higher risk of severe complications from Hepatitis E.
Statistics on Prevalence and Demographics Most Affected
Hepatitis E has a higher prevalence in regions where sanitation and hygiene are poor. It is most commonly seen in parts of Asia, Africa, and Central America. According to the World Health Organization:
- An estimated 20 million HEV infections occur worldwide each year.
- Approximately 3.3 million of these are symptomatic cases of Hepatitis E.
- The disease is responsible for around 44,000 deaths annually.
The demographic most affected by Hepatitis E tends to be young adults aged 15 to 40 years. However, the disease can affect individuals of any age. Pregnant women, in particular, are at a higher risk of acute liver failure associated with the infection.
Symptoms of Hepatitis E
The symptoms of Hepatitis E are similar to those of other types of acute viral hepatitis and can include:
- Jaundice (yellowing of the skin and eyes)
- Fatigue
- Abdominal pain
- Mild fever
- Loss of appetite
- Nausea
- Vomiting
- Clay-colored stools
Symptoms usually resolve within 1-6 weeks. However, in rare cases, especially in pregnant women, the infection can lead to acute liver failure, which is a severe and life-threatening condition.
Diagnosing Hepatitis E
Identifying Hepatitis E accurately is crucial due to its potentially severe implications on health. The process begins with recognizing the symptoms and understanding when to seek testing. This article guides you through the initial screening, specific diagnostic tests, and the pivotal role healthcare professionals play in diagnosing this condition.
Initial Screening and Symptoms Prompting Testing
The journey to diagnosing Hepatitis E often starts with the observation of specific symptoms that mimic those of other viral hepatitis infections. These include jaundice (yellowing of the skin and eyes), fatigue, abdominal pain, loss of appetite, mild fever, and nausea. If these symptoms are present, especially following travel to areas where Hepatitis E is common or after consuming undercooked pork or shellfish, it’s important to consult a healthcare professional.
Specific Diagnostic Tests for Hepatitis E
Upon observing symptoms indicative of Hepatitis E, specific tests are essential to confirm the diagnosis:
- Hepatitis E IgM Antibody Test: This blood test detects IgM antibodies against the Hepatitis E virus (HEV), which are typically present in early infection stages.
- Hepatitis E RNA Test: Used to identify the presence of the HEV RNA in blood or stool, this test confirms active infection. It is particularly useful in chronic cases or in pregnant women, where the virus’s impact can be more severe.
- Liver Function Tests: While not specific to Hepatitis E, these tests help assess liver damage and dysfunction, which are common in hepatitis infections.
The Role of Healthcare Professionals in Diagnosis
Healthcare professionals are indispensable in the diagnosis of Hepatitis E. They perform multiple roles:
- Evaluation and Guidance: Doctors initially assess symptoms and exposure history to determine the likelihood of Hepatitis E.
- Conducting and Interpreting Tests: Healthcare providers not only order the appropriate diagnostic tests based on the clinical presentation but also interpret the results in the context of the patient’s overall health condition.
- Providing Treatment and Follow-up Care: In cases where Hepatitis E is confirmed, medical professionals guide patients through the treatment process and monitor their recovery.
However, early diagnosis and intervention are key in managing Hepatitis E effectively, reducing the risk of severe complications such as acute liver failure. If you experience symptoms consistent with Hepatitis E, it’s important to reach out to a healthcare provider promptly.
Treatment Options for Hepatitis E
Understanding the available treatment options can help manage the symptoms effectively and prevent complications. Here, we explore various approaches to treating Hepatitis E, including medications, supportive care, and the role of diet and lifestyle adjustments.
List of Treatment Approaches
The primary approach to managing Hepatitis E involves supportive care, as specific antiviral medications for this condition are not typically used. Treatment strategies are mainly aimed at alleviating symptoms and include:
- Hydration: Ensuring adequate fluid intake to prevent dehydration.
- Nutritional Support: Eating a well-balanced diet to support liver health and overall immunity.
- Avoiding Alcohol: Alcohol can exacerbate liver disease, so it’s advised to avoid it completely during and after infection.
- Monitoring: Regular monitoring of liver function tests to assess the health of the liver and the progression of the disease.
Specific Treatments: Medications and Supportive Care
In cases where Hepatitis E leads to acute liver failure, specific interventions may be required, including:
- Hospitalization: To provide intensive care and constant monitoring.
- Medications: While there are no specific antivirals for HEV, medications may be administered to manage symptoms such as nausea or pain.
- Liver Transplant: In extreme cases where the liver fails, a transplant may be the only option.
Role of Diet and Lifestyle Adjustments in Managing Symptoms
Lifestyle and dietary adjustments play a crucial role in managing and recovering from Hepatitis E. Patients are advised to:
- Maintain a Low-Fat Diet: High fat foods can be harder on the liver, so a low-fat diet is preferable.
- Increase Fiber Intake: Fibrous foods help improve overall digestive health, which can be beneficial during liver disease.
- Stay Hydrated: Adequate fluid intake helps maintain electrolyte balance and supports liver function.
- Rest: Adequate rest is essential to support the immune system and enhance recovery.
- Avoid Raw or Undercooked Meat: Especially pork and shellfish, as they can harbor the virus and other pathogens harmful to a compromised liver.
However, while there is no specific antiviral treatment for Hepatitis E, effective management involves supportive care, medications to alleviate symptoms, and significant diet and lifestyle changes. These adjustments help mitigate the symptoms and support liver health, contributing to a smoother recovery process.
Treatment Options for Hepatitis E
Understanding the available treatment options can help manage the symptoms effectively and prevent complications. Here, we explore various approaches to treating Hepatitis E, including medications, supportive care, and the role of diet and lifestyle adjustments.
List of Treatment Approaches
The primary approach to managing Hepatitis E involves supportive care, as specific antiviral medications for this condition are not typically used. Treatment strategies are mainly aimed at alleviating symptoms and include:
- Hydration: Ensuring adequate fluid intake to prevent dehydration.
- Nutritional Support: Eating a well-balanced diet to support liver health and overall immunity.
- Avoiding Alcohol: Alcohol can exacerbate liver disease, so it’s advised to avoid it completely during and after infection.
- Monitoring: Regular monitoring of liver function tests to assess the health of the liver and the progression of the disease.
Specific Treatments: Medications and Supportive Care
In cases where Hepatitis E leads to acute liver failure, specific interventions may be required, including:
- Hospitalization: To provide intensive care and constant monitoring.
- Medications: While there are no specific antivirals for HEV, medications may be administered to manage symptoms such as nausea or pain.
- Liver Transplant: In extreme cases where the liver fails, a transplant may be the only option.
Role of Diet and Lifestyle Adjustments in Managing Symptoms
Lifestyle and dietary adjustments play a crucial role in managing and recovering from Hepatitis E. Patients are advised to:
- Maintain a Low-Fat Diet: High fat foods can be harder on the liver, so a low-fat diet is preferable.
- Increase Fiber Intake: Fibrous foods help improve overall digestive health, which can be beneficial during liver disease.
- Stay Hydrated: Adequate fluid intake helps maintain electrolyte balance and supports liver function.
- Rest: Adequate rest is essential to support the immune system and enhance recovery.
- Avoid Raw or Undercooked Meat: Especially pork and shellfish, as they can harbor the virus and other pathogens harmful to a compromised liver.
However, while there is no specific antiviral treatment for Hepatitis E, effective management involves supportive care, medications to alleviate symptoms, and significant diet and lifestyle changes. These adjustments help mitigate the symptoms and support liver health, contributing to a smoother recovery process.
Challenges in Treating Hepatitis E
Hepatitis E is a significant public health issue, especially in rural and underdeveloped regions where access to clean water and medical facilities is often limited. This section delves into the complexities of treating Hepatitis E, highlighting the obstacles faced in such areas, as well as issues like resistance, complications, and the urgency for enhanced research and treatment methods.
Addressing Challenges in Rural and Underdeveloped Regions
Treating Hepatitis E in rural and underdeveloped areas presents unique challenges. These regions often suffer from a lack of basic infrastructure, including inadequate access to clean water, which is critical in preventing the disease. Moreover, limited healthcare facilities and a shortage of trained medical personnel make timely diagnosis and treatment difficult. The remote location of these communities further complicates the delivery of healthcare services and education about disease prevention.
Dealing with Resistance and Chronic Cases
Resistance to treatment and the management of chronic Hepatitis E cases add another layer of complexity. Although Hepatitis E is typically self-limiting, chronic infections can occur, particularly in immunocompromised individuals such as organ transplant recipients, HIV-infected patients, and those receiving chemotherapy. These chronic cases are challenging to manage due to the limited effectiveness of current treatments and the potential for developing resistance to available antiviral medications.
The Imperative for More Research and Improved Treatments
There is a critical need for more comprehensive research into Hepatitis E. This includes developing better diagnostic tools that are both affordable and effective, particularly for use in low-resource settings. Research into new treatments and vaccines is also essential, as current options are often insufficient to tackle the severity and complexity of the disease in varied populations. Improved understanding of the virus’s behavior and transmission in different environmental and social conditions will aid in formulating effective prevention strategies, ultimately reducing the disease burden globally.
However, overcoming the challenges of treating Hepatitis E requires a multifaceted approach that includes enhancing infrastructure in vulnerable regions, addressing drug resistance and chronic infections, and intensifying research efforts to develop more effective treatments and preventive measures.
Recent Advances in Hepatitis E Treatment
Hepatitis E, a viral infection primarily transmitted through contaminated water, has seen significant strides in treatment and management in recent years. This section delves into the latest research findings, emerging drugs, and the promising future of Hepatitis E treatment.
Latest Research Findings and Advancements in Treatment
Recent research into Hepatitis E has brought forward new insights that are shaping the approach to treatment. Advances in understanding the molecular biology of the Hepatitis E virus (HEV) have led to the development of targeted therapies that can more effectively combat the virus. Studies have shown that ribavirin, an antiviral drug, can be particularly effective in treating chronic Hepatitis E, offering a sustained virologic response in a significant percentage of cases. Additionally, improved diagnostic techniques are enabling earlier detection of the disease, which is crucial for effective treatment.
Emerging Drugs and Therapeutic Strategies
The landscape of Hepatitis E treatment is evolving with the introduction of emerging drugs and innovative therapeutic strategies. Researchers are exploring the use of sofosbuvir, traditionally used for Hepatitis C, in treating HEV, particularly in organ transplant recipients who are at higher risk for chronic infections. Preliminary results are promising, indicating that sofosbuvir may reduce viral load effectively in HEV-infected individuals.
Another exciting development is the potential use of vaccines. Although a vaccine for Hepatitis E (HEV 239) is available in China, its global application and acceptance are still under discussion. Ongoing trials aim to test its efficacy and safety in broader populations, which could revolutionize preventative strategies against HEV.
The Future of Hepatitis E Treatment and Management
Looking ahead, the future of Hepatitis E treatment appears promising. The ongoing research into antiviral therapies and vaccines is expected to yield more effective and accessible treatments. Additionally, there is a growing emphasis on integrating lifestyle and dietary modifications alongside medical treatment to manage symptoms and prevent disease progression.
As global health systems continue to improve surveillance and reporting mechanisms for Hepatitis E, earlier detection and treatment will likely become more common, reducing the disease’s impact significantly. With these advancements, Hepatitis E could transform from a challenging public health issue to a manageable condition, improving quality of life for patients around the world.
By focusing on innovative treatments and preventive strategies, the medical community is poised to make significant advancements in the fight against Hepatitis E, promising a healthier future for individuals affected by this virus.
FAQs About Hepatitis E Treatment
What are the main treatments for Hepatitis E?
Hepatitis E typically resolves on its own without the need for medical treatment. However, maintaining proper hydration is crucial. In severe cases, especially among pregnant women or those with weakened immune systems, hospitalization may be necessary to manage complications like acute liver failure.
Is there a specific medication for Hepatitis E?
Currently, there are no specific antiviral medications approved for the treatment of Hepatitis E. Treatment mainly involves supportive care, such as rehydration and rest. Research is ongoing to find effective specific treatments.
Can Hepatitis E be treated at home?
Yes, most cases of Hepatitis E can be managed at home with adequate fluid intake, rest, and a healthy diet. It is important to avoid alcohol as it can further strain liver function. Always consult with a healthcare provider for guidance tailored to your specific health condition.
How long does it take to recover from Hepatitis E?
The duration of the illness varies, but most people recover completely within one to two months. Symptoms such as jaundice, fatigue, and abdominal pain typically improve within a few weeks.
Is there a vaccine for Hepatitis E?
Yes, there is a vaccine for Hepatitis E, known as HEV 239, available in some countries. It is primarily recommended for people at higher risk of exposure, such as travelers to areas with high incidence rates of the virus, but it is not widely available globally.
Are there any dietary recommendations for someone with Hepatitis E?
A diet high in fruits, vegetables, and lean proteins can help support liver health. It’s also recommended to stay hydrated and avoid fatty, fried, or spicy foods as they can exacerbate liver stress.
When should someone with Hepatitis E see a doctor?
Consult a healthcare provider if you suspect you have Hepatitis E or if symptoms persist or worsen, such as severe nausea, vomiting, and yellowing of the skin or eyes. Pregnant women or individuals with chronic liver disease should seek medical attention immediately if infected.
Conclusion
In conclusion, the effective diagnosis and treatment of Hepatitis E are crucial for managing and mitigating the impacts of this potentially serious viral infection. With Hepatitis E predominantly transmitted through contaminated water sources, understanding and awareness are key to prevention and control.
It is essential for individuals, especially those in at-risk areas, to recognize the symptoms early and seek prompt medical attention. By doing so, they can reduce the risk of severe complications and contribute to better health outcomes.
We encourage everyone to stay informed and consult healthcare professionals if they suspect exposure to the virus. Early intervention is the best defense against the challenges posed by Hepatitis E.
References
For those interested in exploring more about the treatment of Hepatitis E and seeking further validation of the information provided, the following resources are highly reputable and can offer deeper insights:
- Centers for Disease Control and Prevention (CDC) – The CDC website provides comprehensive information on Hepatitis E, including symptoms, diagnosis, treatment, and prevention strategies. Visit their page on Hepatitis E here.
- World Health Organization (WHO) – WHO offers detailed guidelines and global data on Hepatitis E, which are essential for understanding the worldwide impact and treatment protocols. Access their resources on Hepatitis E here.
- Mayo Clinic – As a leading healthcare organization, Mayo Clinic offers a detailed overview of Hepatitis E, including causes, treatments, and tips for management. Learn more from their Hepatitis E section here.
These sources are updated regularly to reflect the latest research and findings in the field of Hepatitis E treatment and can serve as a reliable foundation for further reading.