Hepatitis C Symptoms: Hepatitis C is a viral infection that primarily affects the liver, leading to significant health complications if not diagnosed and managed effectively.
Understanding the symptoms and causes of Hepatitis C is crucial for early detection and treatment, which can significantly improve health outcomes.
What is Hepatitis C?
Hepatitis C is an infectious disease primarily affecting the liver, caused by the Hepatitis C virus (HCV). This disease can range from a mild illness lasting a few weeks to a serious, lifelong condition that can lead to severe liver damage or even liver cancer.
Brief History and Prevalence of the Disease
Hepatitis C was first identified in the late 1980s when it became apparent that there was another bloodborne hepatitis virus other than hepatitis A and B. Since its discovery, it has been a major public health challenge. It is estimated that approximately 58 million people worldwide are living with chronic Hepatitis C infection, with a significant number of these cases found in Eastern Mediterranean and European regions.
The prevalence of the disease varies greatly across different populations and regions, influenced by factors such as healthcare practices and the prevalence of high-risk behaviors. Advances in medical research have led to the development of direct-acting antiviral (DAA) drugs that have significantly improved treatment outcomes, offering a cure rate of over 95% in many cases.
However, early diagnosis and treatment can prevent health complications related to the disease and reduce its spread, highlighting the importance of awareness and education on Hepatitis C.
Understanding Hepatitis C Transmission
Understanding the transmission of this virus is crucial for prevention and managing its spread. Below, we explore the primary modes of transmission and the risk factors associated with contracting Hepatitis C.
Key Modes of Hepatitis C Transmission
1. Blood-to-Blood Contact: The most common route of transmission for Hepatitis C is through direct contact with infected blood. This can occur in various scenarios:
- Sharing Injection Equipment: People who inject drugs and share needles, syringes, or other injection equipment are at a high risk of contracting HCV.
- Healthcare Exposures: Accidental needle sticks or improper sterilization of medical equipment in healthcare settings can also transmit the virus.
- Tattooing and Piercing: Getting tattoos or piercings with non-sterile equipment can expose individuals to infected blood.
2. Mother-to-Child Transmission: Although less common, Hepatitis C can be transmitted from an infected mother to her baby during childbirth.
3. Sexual Contact: While the risk is significantly lower compared to other blood-borne diseases like HIV, HCV can still be transmitted through sexual activities, particularly among individuals with multiple partners or those who engage in rough sex, which can lead to bleeding.
Risk Factors for Contracting Hepatitis C
Understanding who is at risk can help in targeting preventive measures effectively. Here are the main risk factors:
- Injection Drug Use: The highest risk factor for Hepatitis C is the sharing of needles or other equipment used for injecting drugs.
- Healthcare Workers: Those who work in healthcare environments are at an elevated risk due to the possibility of coming into contact with infected blood, especially through needlestick injuries.
- Receiving Blood Transfusions or Organ Transplants: Before widespread screening of the blood supply began in 1992, Hepatitis C was often spread through transfusions and transplanted organs. Today, this risk is very low in countries where blood is tested for HCV.
- HIV-Positive Individuals: People who are HIV-positive are at a higher risk of co-infection with Hepatitis C, particularly due to similar routes of transmission.
- Individuals with Incarceration History: High-risk behaviors, such as sharing needles or unprotected sex, are more prevalent in correctional facilities, increasing the risk of HCV transmission.
However, engaging in safe injection practices, ensuring the use of sterile medical equipment, and avoiding sharing personal items like razors or toothbrushes that might have blood on them are practical steps to reduce the risk of infection.
Symptoms of Hepatitis C
It is essential to recognize the symptoms of Hepatitis C, as they play a crucial role in early diagnosis and treatment. Below, we explore the symptoms associated with the different stages of Hepatitis C, including acute and chronic phases, as well as asymptomatic cases.
Early-Stage Symptoms (Acute Hepatitis C)
The initial phase of Hepatitis C, known as acute Hepatitis C, often doesn’t manifest noticeable symptoms. When symptoms do appear, they are typically mild and flu-like, occurring within two weeks to six months after exposure to the virus. These symptoms may include:
- Fatigue: Often described as significant tiredness or exhaustion that doesn’t improve with rest.
- Fever: A mild to moderate fever, usually one of the first signs of infection.
- Appetite Loss: Decreased interest in eating, often accompanied by weight loss.
- Nausea: Feelings of sickness often leading to vomiting.
- Muscle and Joint Pain: General aches that are not linked to any specific injury.
- Abdominal Pain: Especially discomfort around the liver area.
- Jaundice: Yellowing of the skin and eyes, which indicates liver dysfunction.
It’s important to note that many people with acute Hepatitis C do not experience any symptoms and therefore do not seek medical treatment.
Chronic Hepatitis C Symptoms
If the virus remains in the body after the acute phase, it can lead to chronic Hepatitis C. This stage can last for decades without noticeable symptoms, making it particularly dangerous. Over time, chronic Hepatitis C can cause severe liver damage, including cirrhosis and liver cancer. Symptoms of chronic Hepatitis C may include:
- Persistent Fatigue: Continues to be a prevalent symptom.
- Cognitive Difficulties: Problems with concentration, memory, and completing complex tasks.
- Digestive Issues: Poor appetite, nausea, and indigestion.
- Skin Problems: Itching and rashes.
- Swelling in the Legs, Ankles, or Abdomen: Due to fluid buildup caused by liver scarring.
- Easy Bruising and Bleeding: As liver function declines, blood clotting may be impaired.
- Dark Urine and Pale Stool: Changes in waste elimination indicating liver issues.
Discussing Asymptomatic Cases
Many individuals with Hepatitis C do not exhibit any symptoms, particularly in the early stages of the infection. This asymptomatic nature often leads to a delay in diagnosis and treatment, increasing the risk of transmitting the virus to others. Regular medical check-ups and blood tests are critical, especially for those at higher risk of contracting HCV, such as people who have injected drugs, received unscreened blood transfusions before 1992, or have been exposed to contaminated medical equipment.
If you suspect you have been exposed to the hepatitis C virus or belong to a high-risk group, consult with a healthcare provider for testing and appropriate guidance.
Causes of Hepatitis C
This comprehensive guide explores the various avenues through which this infection can occur, emphasizing the predominant role of blood transmission, as well as highlighting some lesser-known causes that can contribute to its spread.
The Role of Blood-to-Blood Contact
The most common mode of Hepatitis C transmission is through blood-to-blood contact. This can occur in several ways:
- Injecting Drug Use: Sharing needles or other injecting equipment is the most frequent method through which HCV is spread. Tiny traces of blood, often invisible, can carry the virus from one person to another.
- Medical Procedures: Inadequately sterilized medical equipment can pose a risk, especially in healthcare settings where infection control practices are poor. This includes procedures like blood transfusions and organ transplants, particularly before widespread screening of the blood supply began in 1992.
- Tattooing and Piercing: Getting a tattoo or piercing with non-sterile equipment can also be a risk factor for acquiring Hepatitis C. It’s crucial that these procedures are done with properly sterilized tools.
Other Less Common Causes
In addition to the primary blood-to-blood transmission route, there are other, less frequent ways Hepatitis C can be transmitted:
- From Mother to Child: During childbirth, an infected mother can pass the virus to her baby. This is relatively uncommon, but it can occur.
- Sexual Contact: While sexual transmission of Hepatitis C is much less efficient than other bloodborne viruses like HIV, it’s still possible, especially among individuals with multiple sexual partners or those who have sexually transmitted infections.
- Shared Personal Items: Personal items such as razors or toothbrushes, which might come into contact with blood, can also be a source of infection, although this is rare.
By recognizing how the virus spreads, individuals can take steps to minimize their risk and health authorities can better focus their prevention strategies.
Complications of Hepatitis C
Understanding these complications is crucial for individuals diagnosed with or at risk for Hepatitis C. Here we explore the primary complications associated with this condition, emphasizing liver cirrhosis, liver cancer, and other health issues linked to chronic Hepatitis C.
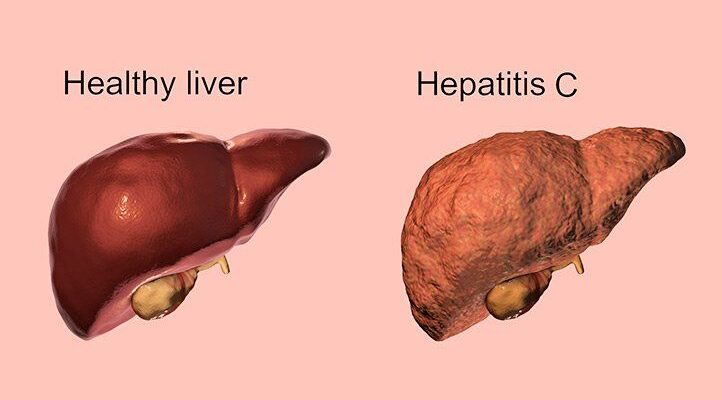
Liver Cirrhosis
Liver cirrhosis is one of the most severe complications of chronic Hepatitis C. It occurs when healthy liver tissue is replaced by scar tissue, impairing the liver’s ability to function properly. This scarring is a gradual process resulting from long-term, continuous damage to the liver. Symptoms may not be evident in the early stages but can develop into more serious problems like jaundice, bleeding disorders, and fluid accumulation in the abdomen. Preventing the progression of liver cirrhosis is critical and requires regular monitoring and treatment of Hepatitis C.
Liver Cancer
Individuals with chronic Hepatitis C are also at an increased risk of developing liver cancer, specifically hepatocellular carcinoma (HCC), the most common type of liver cancer. The risk of liver cancer increases significantly in patients who have developed cirrhosis due to Hepatitis C. Early detection and treatment of Hepatitis C can significantly reduce the risk of developing liver cancer. Regular surveillance for liver cancer is recommended for patients with advanced liver disease related to Hepatitis C.
Other Health Complications
Chronic Hepatitis C can also lead to complications beyond the liver. These include:
- Cryoglobulinemia: A condition where abnormal proteins in the blood clump together at lower temperatures, leading to inflammation and damage to various organs.
- Glomerulonephritis: A type of kidney disease caused by inflammation of the small blood vessels in the kidneys.
- Peripheral neuropathy: Damage to the nerves outside the brain and spinal cord, resulting in weakness, numbness, and pain typically in the hands and feet.
- Diabetes: Patients with chronic Hepatitis C are at a higher risk of developing type 2 diabetes, due to the virus’s impact on glucose metabolism.
Early diagnosis and appropriate management of Hepatitis C are crucial in preventing these complications. With the advancements in antiviral treatments, many individuals have a chance for a full recovery, significantly lowering the risks associated with the disease.
Effective management and awareness are key in preventing the serious consequences of Hepatitis C. Regular check-ups and adherence to treatment plans can help mitigate the impact of this condition and enhance the quality of life for those affected.
Diagnosis of Hepatitis C
Here, we explore the various methods used for screening and diagnosing this condition, and discuss why early diagnosis is essential.
Methods of Screening and Diagnostic Tests for Hepatitis C
Screening for Hepatitis C is recommended for individuals who are at risk of infection. The following methods are commonly used to diagnose HCV:
- HCV Antibody Test (Anti-HCV): This is the initial screening test used to detect antibodies to the Hepatitis C virus in the blood. A positive result indicates either a current or past infection and requires further testing to confirm active infection.
- HCV RNA Test: This test detects the presence of the virus’s RNA in the blood and confirms active infection. It is used following a positive HCV antibody test to confirm that the infection is current.
- HCV Genotype Test: After confirming an active infection, an HCV genotype test is conducted to determine the specific type or strain of the virus. This information is crucial for guiding treatment options as certain medications are more effective against specific genotypes.
- Liver Function Tests: These tests assess the liver’s health and function by measuring levels of liver enzymes in the blood. Abnormal results may suggest liver damage caused by Hepatitis C.
- Liver Biopsy: A more invasive procedure, a liver biopsy involves removing a small piece of liver tissue for examination. This test helps assess the degree of liver damage and fibrosis, which is important for determining the stage of the disease.
- FibroScan: Also known as transient elastography, this non-invasive test uses ultrasound waves to measure the stiffness of the liver. Stiffness indicates fibrosis, which helps evaluate liver damage without a biopsy.
- Imaging Tests: Techniques such as ultrasound, CT scans, and MRIs can be used to visualize the liver and assess for signs of liver damage or complications like cirrhosis.
Importance of Early Diagnosis
The importance of early diagnosis of Hepatitis C cannot be overstated. Early detection allows for timely intervention, which can significantly enhance the effectiveness of treatment. With recent advances in antiviral medications, Hepatitis C is now curable in most cases. Early treatment can prevent the progression of the disease to severe liver damage such as cirrhosis or liver cancer.
Moreover, diagnosing Hepatitis C early helps reduce the risk of transmission to others, as individuals who are aware of their infection status can take precautions to prevent spreading the virus. This is particularly important since Hepatitis C is primarily transmitted through blood-to-blood contact.
However, regular screening and diagnostic tests for Hepatitis C are key tools in the fight against this silent epidemic. They enable healthcare providers to detect the virus early, initiate effective treatment sooner, and prevent serious health complications, thereby improving the quality of life for those affected by HCV.
Prevention and Management of Hepatitis C
Preventing the transmission of Hepatitis C is crucial, as there is no vaccine currently available for the virus. The primary routes of Hepatitis C transmission include sharing needles, syringes, or other equipment to prepare and inject drugs, unsafe healthcare practices, unsterile tattoo and piercing equipment, and less commonly, through sexual contact. To reduce the risk of infection, the following preventive measures are recommended:
- Use of Sterile Needles: Always use new and sterile needles and syringes for each injection, whether for medical purposes or recreational drug use.
- Safe Medical Practices: Ensure that all medical and dental procedures are performed with sterile equipment. Healthcare facilities should adhere to strict infection control practices.
- Personal Hygiene Items: Avoid sharing personal items that may have come into contact with blood, such as razors, toothbrushes, and nail clippers.
- Tattoos and Piercings: Opt for reputable and licensed facilities that use sterile equipment and practice good hygiene.
- Education and Awareness: Spreading awareness about the modes of transmission and preventive strategies can significantly reduce the risk of Hepatitis C spread.
Implementing these measures can significantly decrease the risk of acquiring Hepatitis C.
Current Treatment Options and Management Strategies
Treatment for Hepatitis C has evolved significantly over the past decade, improving the outlook for those affected. The introduction of Direct-Acting Antivirals (DAAs) has revolutionized treatment, offering cure rates above 90%. These medications are generally well-tolerated, have fewer side effects, and require a shorter course of treatment compared to older therapies.
Management strategies for Hepatitis C involve:
- Regular Monitoring: Regular monitoring of liver function and viral levels helps determine the treatment’s effectiveness and progression of the disease.
- Lifestyle Adjustments: Patients are advised to avoid alcohol and reduce their liver’s workload, maintain a healthy weight, and follow a balanced diet.
- Co-infection Management: For those co-infected with HIV or Hepatitis B, managing all conditions simultaneously is crucial to improve overall health outcomes.
Future Outlook on Vaccines and Treatments
Research into developing a vaccine for Hepatitis C is ongoing. Although there are significant challenges due to the virus’s ability to mutate, recent advances in technology and understanding of the virus provide hope that a vaccine might be available in the future.
Additionally, treatment methods continue to improve, with new DAAs in development that promise even higher efficacy and fewer side effects. The focus is also shifting towards finding effective treatments for all genotypes of the virus, making treatment more accessible globally.
The future of Hepatitis C treatment and management looks promising, with continuous advancements paving the way towards more effective solutions and, hopefully, a vaccine.
FAQs about Hepatitis C Symptoms and Causes
1. What are the common symptoms of Hepatitis C?
Hepatitis C can often be a silent condition, especially in its early stages. Many individuals do not experience any symptoms initially. However, when symptoms do appear, they may include fatigue, jaundice (yellowing of the skin and eyes), abdominal pain, especially around the liver area, loss of appetite, nausea, and dark urine. It’s important to consult a healthcare provider for proper diagnosis and management if you experience any of these symptoms.
2. How long after exposure do Hepatitis C symptoms appear?
Symptoms of Hepatitis C can appear anywhere from 2 weeks to 6 months after exposure to the virus. However, many people might not notice any symptoms for several years, which is why Hepatitis C is often identified during routine medical tests or blood donation.
3. What causes Hepatitis C?
Hepatitis C is caused by the Hepatitis C virus (HCV). It is primarily transmitted through direct contact with infected blood. This can occur through sharing needles, syringes, or other equipment to inject drugs, unsanitary tattooing and piercing practices, and occasionally from mother to child during birth. It is less commonly transmitted through sexual contact.
4. Can Hepatitis C be sexually transmitted?
While Hepatitis C is not primarily a sexually transmitted disease, it can be transmitted sexually, particularly among individuals with multiple sexual partners, those who engage in rough sexual activities that may lead to bleeding, or among those with HIV. Safe sexual practices and regular health check-ups are advised to prevent transmission.
5. Is there a vaccine available for Hepatitis C?
Currently, there is no vaccine available for Hepatitis C. Prevention focuses on reducing the risk of exposure to the virus, primarily in healthcare settings and through public health interventions concerning drug use and needle safety. Research is ongoing, and scientists continue to work towards developing a vaccine.
6. Who is at risk of developing Hepatitis C?
Individuals at higher risk for Hepatitis C include those who have injected drugs and shared needles or syringes, recipients of blood transfusions or organ transplants before 1992 (when widespread screening of the blood supply began in the U.S.), healthcare workers after needlestick injuries, and individuals with HIV. Regular screening is recommended for those at high risk.
7. Can Hepatitis C be cured?
Yes, with advances in medical treatment, Hepatitis C can be cured. Direct-acting antiviral drugs (DAAs) are highly effective at clearing the virus from the body, usually within 8-12 weeks of treatment. It is important to diagnose the condition early and follow through with the prescribed treatment regimen.
Conclusion:
Understanding the symptoms and causes of Hepatitis C is crucial for early detection and effective management of the disease. Hepatitis C can often go unnoticed due to its mild or non-existent early symptoms, which can lead to serious liver damage over time if left untreated. Key symptoms to be aware of include fatigue, jaundice, abdominal pain, and unusual changes in urine and stool color.
For those who might be at risk—such as individuals with a history of intravenous drug use, those who have received contaminated blood transfusions, or have been exposed to unsterile medical equipment—it’s imperative to prioritize getting tested. Early testing can lead to timely treatment, significantly reducing the risk of severe liver complications like cirrhosis and liver cancer.
We strongly encourage anyone who believes they may be at risk for Hepatitis C to consult with a healthcare provider and consider screening. Taking action now can preserve health, prevent complications, and save lives. Your proactive steps towards testing could be the key to a healthier future.
References
For more comprehensive information and to validate the details discussed regarding Hepatitis C symptoms, consider exploring the following reputable sources. These references are essential for anyone seeking deeper insights or further reading on this significant health topic.
- Centers for Disease Control and Prevention (CDC) – The CDC offers extensive resources on Hepatitis C, including symptoms, transmission, and treatment options. Access their dedicated Hepatitis C section here.
- World Health Organization (WHO) – WHO provides global statistics, reports, and public health guidelines concerning Hepatitis C. Their informational portal can be found here.
- Mayo Clinic – For detailed medical content on the symptoms, causes, and treatments of Hepatitis C, visit the Mayo Clinic’s resource page here.
- PubMed Central – A service of the U.S. National Institutes of Health, this site offers access to numerous academic research papers on Hepatitis C. Explore the latest research here.
Each of these sources provides credible and detailed information that can enhance your understanding of Hepatitis C, aiding in both academic and personal research endeavors.