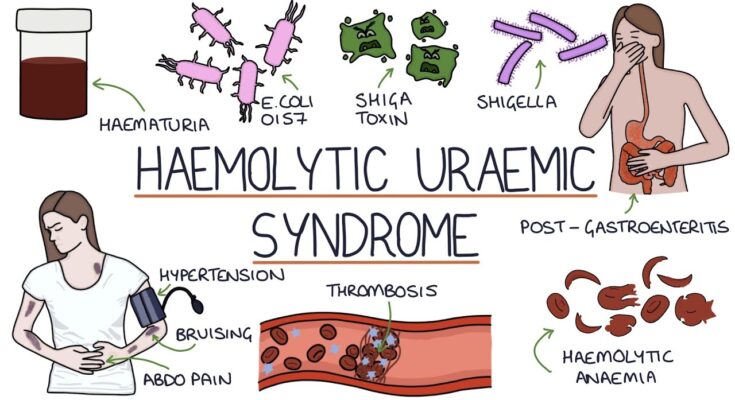
Hemolytic Uremic Syndrome Symptoms: Hemolytic Uremic Syndrome (HUS) is a severe, life-threatening condition primarily characterized by the triad of hemolytic anemia, acute kidney failure (uremia), and a low platelet count (thrombocytopenia).
Predominantly affecting children, this rare disorder can lead to significant morbidity and mortality if not diagnosed and treated promptly.
What is Hemolytic Uremic Syndrome?
Hemolytic Uremic Syndrome (HUS) is a serious condition primarily characterized by the destruction of red blood cells, acute kidney failure, and low platelet count. This syndrome can lead to severe complications, including permanent kidney damage and even death if not promptly treated.
How Hemolytic Uremic Syndrome Affects the Body
HUS typically unfolds in three critical stages affecting various body systems:
- Hemolysis: The sudden destruction of red blood cells leads to hemolysis, where parts of the red blood cells are scattered into the bloodstream, causing fatigue, pallor, and shortness of breath.
- Thrombocytopenia: A low platelet count follows, which is crucial for blood clotting. This reduction can cause bleeding issues, bruising easily, and prolonged bleeding from cuts.
- Renal Failure: The fragmented cells and other elements can clog the kidney’s filtering system, leading to acute kidney failure. This is marked by a decreased urine output, fluid retention, and swelling.
Prevalence and Demographics
HUS is rare, affecting about 2-3 per 100,000 people annually in the United States. The syndrome is most prevalent among children under the age of 5, particularly those who have been exposed to certain strains of E. coli bacteria, which are often contracted from contaminated food or water. Although less common, adults can also develop HUS, particularly those with weakened immune systems, pregnant women, or those with certain chronic diseases.
Awareness and early detection are critical for managing HUS effectively, highlighting the importance of recognizing symptoms early and seeking immediate medical attention.
Symptoms of Hemolytic Uremic Syndrome
Hemolytic uremic syndrome (HUS) is a serious condition primarily characterized by the destruction of red blood cells, acute kidney failure, and low platelet count. Understanding the symptoms of HUS is crucial for early diagnosis and treatment. Here, we detail the common symptoms, their progression, and guidelines on when to seek medical help.
Detailed List of Common Symptoms
Hemolytic uremic syndrome manifests through a variety of symptoms, which can vary in severity among individuals:
- Fatigue and Weakness – Due to the rapid destruction of red blood cells, individuals often experience significant fatigue and generalized weakness.
- Pale Skin – The loss of red blood cells can lead to paleness and a washed-out appearance.
- Fever – Although not present in all cases, some individuals may experience a low-grade fever.
- Bleeding Problems – A reduced platelet count can cause issues such as nosebleeds, bleeding gums, and easy bruising.
- Decreased Urine Output – Kidney impairment can result in reduced urine production, a key indicator of HUS.
- Dark or Bloody Urine – The urine may appear dark or bloody due to the kidneys filtering out damaged cells and waste.
- Swelling – Fluid retention can cause swelling, particularly in the legs, ankles, and around the eyes.
- Vomiting and Diarrhea – These symptoms are often the initial signs, sometimes containing blood.
- Confusion or Seizures – Severe cases can affect neurological functions, leading to confusion or seizures due to toxins affecting the brain.
Explanation of Symptom Progression
The progression of symptoms in HUS typically follows the onset of gastrointestinal symptoms like diarrhea and vomiting, which may be bloody. This is often followed by the more severe signs such as decreased urine output and swelling, indicative of kidney involvement. As the condition progresses, red blood cell destruction leads to fatigue, paleness, and further complications like bleeding issues due to low platelets. Neurological symptoms suggest an advanced stage requiring immediate attention.
When to Seek Medical Help
Immediate medical attention is critical if HUS is suspected, especially under the following circumstances:
- Persistent or Bloody Diarrhea: This is often one of the first signs of HUS, particularly following a gastrointestinal illness.
- Reduced Urine Output: A noticeable decrease in urine frequency or volume, especially if accompanied by dark or bloody urine.
- Unexplained Bruising or Bleeding: These are signs of a potentially serious decrease in platelet levels.
- Severe Fatigue or Weakness: These symptoms can indicate the worsening of anemia associated with red blood cell destruction.
- Swelling in the Limbs or Face: Swelling can be a sign of fluid retention related to kidney damage.
- Any Neurological Symptoms: Confusion, difficulty with concentration, or seizures are urgent symptoms that require immediate evaluation.
If you or someone you know begins to show signs of these symptoms, especially after an episode of severe diarrhea or a known outbreak of E. coli infection, seeking prompt medical evaluation is crucial. Early diagnosis and treatment can significantly improve outcomes in cases of hemolytic uremic syndrome.
Causes of Hemolytic Uremic Syndrome
Understanding the primary causes, risk factors, and predispositions associated with HUS is essential for prevention and management. This section explores these aspects to provide clear insights into the origins and risk enhancers of the syndrome.
Primary Causes of Hemolytic Uremic Syndrome
- Infection with Shiga Toxin-Producing Bacteria: The most common trigger for HUS is an infection by Shiga toxin-producing Escherichia coli (STEC), particularly E. coli O157:H7. These bacteria are typically acquired through the consumption of contaminated food or water, or through contact with an infected individual.
- Other Bacterial Infections: Apart from E. coli, other bacteria such as Shigella and Salmonella can also produce Shiga toxins that may lead to HUS.
- Genetic Factors: Atypical HUS (aHUS) is a less common form of the syndrome, often caused by genetic mutations that result in uncontrolled complement activation, a part of the immune system that contributes to inflammation and cell destruction.
- Certain Medications: Some medications, including chemotherapy drugs and immunosuppressants, can trigger HUS by causing damage to the endothelial cells lining the blood vessels.
- Pregnancy: HUS can occasionally occur in pregnant women, likely due to changes in the immune system and the body’s response to the placenta.
Risk Factors and Predispositions
Several factors may predispose individuals to developing HUS:
- Age: Children under 5 years of age and the elderly are more susceptible due to their relatively weaker immune systems.
- Weakened Immune System: Individuals with weakened immune systems, whether from conditions such as HIV/AIDS or from medical treatments such as chemotherapy, are at higher risk.
- Certain Genetic Conditions: People with hereditary predispositions to problems with the complement system are at increased risk for atypical HUS.
- Environmental Exposure: Outbreaks of STEC infections are often linked to specific sources such as undercooked meat, especially ground beef, unpasteurized milk, and contaminated water.
Awareness and timely medical intervention can significantly mitigate the severity of the condition and improve outcomes.
Diagnosis of Hemolytic Uremic Syndrome
Diagnosing Hemolytic Uremic Syndrome (HUS) is critical, as early detection and treatment significantly influence patient outcomes. HUS, primarily characterized by the triad of hemolytic anemia, acute renal failure, and thrombocytopenia, requires a careful and prompt assessment. Below is a comprehensive list of diagnostic procedures that healthcare providers use to diagnose HUS, along with an explanation of why early diagnosis is vital.
List of Diagnostic Procedures
- Complete Blood Count (CBC): A CBC is one of the first tests done to check for low platelets (thrombocytopenia), low red blood cell count (anemia), and elevated white cells as signs of infection or inflammation.
- Blood Smear: Under a microscope, a blood smear can reveal schistocytes (fragmented red cells) which indicate hemolytic anemia.
- Kidney Function Tests: Tests such as serum creatinine and blood urea nitrogen (BUN) assess kidney function and determine the extent of any damage or failure.
- Urinalysis: This test looks for abnormalities in the urine, such as the presence of blood or protein, which signal kidney problems.
- Stool Tests: Since some types of HUS are caused by infectious agents like E. coli O157:H7, testing a stool sample can help identify the presence of these bacteria.
- Serologic Tests: These tests can detect antibodies that may be involved in the immune response leading to HUS.
- Direct Coombs Test: This test checks for antibodies that are bound to the surface of red blood cells, indicating autoimmune causes that can lead to cell destruction.
- Genetic Testing: In cases where a hereditary form of HUS is suspected, genetic testing can identify mutations that might be responsible for the disease.
Importance of Early Diagnosis and Its Impact on Outcomes
Early diagnosis of HUS is crucial for several reasons. Timely intervention can prevent the progression of kidney damage, potentially averting the need for dialysis or transplantation. Early treatment with appropriate supportive therapies such as hydration and careful management of electrolytes can stabilize the patient’s condition.
Moreover, identifying the underlying cause of HUS, whether it’s an infection, genetic mutation, or autoimmune disorder, can influence treatment decisions and help prevent recurrence. For example, if HUS is caused by an infectious agent, managing the infection early can reduce the severity and duration of the syndrome.
Furthermore, the prognosis of HUS can vary widely, but early diagnosis generally leads to better outcomes. Patients diagnosed and treated early have a significantly lower risk of developing severe complications like chronic kidney disease and hypertension.
Overall, the diagnostic process for Hemolytic Uremic Syndrome is geared towards not only confirming the presence of the syndrome but also understanding its etiology to guide targeted and effective treatment. The sooner HUS is diagnosed and treated, the better the chances are for a full recovery.
Treatment Options for Hemolytic Uremic Syndrome (HUS)
Understanding the treatment options and preventive measures is crucial for managing this disease effectively. Here, we explore the general treatment approaches, the latest advancements in treatment, and preventive measures to avoid the onset of HUS.
General Treatment Approaches for HUS
Treatment for HUS primarily focuses on supportive care to relieve symptoms and manage complications. The general treatment approaches include:
- Fluid Replacement: To prevent dehydration and maintain fluid balance, which is crucial for kidney function.
- Electrolyte Management: Monitoring and correcting imbalances in blood electrolytes like potassium and sodium that can occur due to kidney dysfunction.
- Blood Transfusions: For patients experiencing severe anemia, transfusions of red blood cells may be necessary.
- Plasma Exchange: In some severe cases, plasma exchange (plasmapheresis) can help by removing the substances in the blood that may be causing the disease to worsen.
- Kidney Dialysis: If the kidneys are unable to function properly, temporary dialysis can support the body until kidney function is restored.
Latest Advancements in Treatment
In recent years, research has led to new insights and potential treatments for HUS:
- Eculizumab (Soliris): This is a monoclonal antibody that has shown promise in treating atypical HUS by inhibiting the complement system, part of the immune system that contributes to inflammation and cell damage in HUS.
- Genetic Testing: Advances in genetic testing allow for better identification of atypical HUS, which can be crucial for selecting the most effective treatment strategies for individual patients.
Preventative Measures to Avoid the Onset of HUS
Preventing HUS mainly involves avoiding the initial infection that can lead to the syndrome, especially infections caused by E. coli, which are commonly linked to HUS in children. Here are some preventive steps:
- Proper Food Safety: Wash fruits and vegetables thoroughly, cook meat thoroughly, and avoid unpasteurized dairy products and juices.
- Good Hygiene Practices: Wash hands regularly, especially after using the restroom, before eating, and after contact with farm animals, which can carry harmful bacteria.
- Water Safety: Ensure that drinking water is clean and safe, particularly when traveling to areas where water quality may be uncertain.
By understanding these treatment and prevention strategies, individuals can be better prepared to manage HUS and minimize its impact on health. Always consult healthcare professionals for advice tailored to your specific circumstances.
Prevention and Risk Management of Hemolytic Uremic Syndrome (HUS)
Understanding how to prevent these infections can significantly reduce the risk of developing HUS. Here are practical tips and strategies for prevention and risk management of HUS.
Tips for Preventing Infection Leading to HUS
- Maintain Good Hygiene: Regular hand washing is crucial, especially before eating or preparing food and after using the restroom. Teach children the importance of washing their hands thoroughly to minimize their risk of infection.
- Proper Food Preparation: Cook meat, particularly ground beef, to a safe internal temperature of at least 160°F (71°C) to kill E. coli bacteria. Use a food thermometer to ensure meats have reached a safe temperature.
- Avoid Raw Milk: Consume only pasteurized milk and dairy products. Raw milk can contain harmful bacteria capable of causing severe infections leading to HUS.
- Wash Fruits and Vegetables: Thoroughly wash all fruits and vegetables under running water before eating or cooking them, even if they will be peeled.
- Be Cautious with Water: Avoid swallowing water when swimming in pools, lakes, or ponds, as these can sometimes be contaminated with E. coli.
- Educate Yourself About Food Recalls: Stay informed about current food recalls and safety alerts, which can help you avoid consuming contaminated products that may be linked to E. coli outbreaks.
Monitoring and Managing At-Risk Populations
Certain populations are more at risk of developing HUS, including young children, the elderly, and individuals with weakened immune systems. Here’s how to monitor and manage these at-risk groups:
- Regular Check-Ups: Ensure that at-risk individuals attend regular medical check-ups. Early detection of symptoms can lead to timely treatment and better outcomes.
- Educate on Symptoms: Educate caregivers and at-risk populations about the symptoms of E. coli infection, which include severe stomach cramps, diarrhea (often bloody), and vomiting. Recognizing these symptoms early can prompt quicker medical attention.
- Manage Diarrheal Illness Aggressively: For those in high-risk groups, any diarrheal illness should be taken seriously and medical advice sought promptly. Dehydration is a common complication and should be addressed quickly.
- Community Awareness Programs: Implement community health programs that focus on hygiene, food safety, and the risks of HUS. Education can empower individuals to take proactive steps in preventing infections.
- Resource Availability: Ensure that resources for proper hygiene and clean water are available, especially in communities with high rates of E. coli infection.
By following these prevention tips and carefully managing at-risk populations, the incidence of HUS can be reduced, protecting public health and saving lives.
FAQs about Hemolytic Uremic Syndrome Symptoms
What are the primary symptoms of Hemolytic Uremic Syndrome (HUS)?
Hemolytic Uremic Syndrome is characterized by three main symptoms: acute kidney failure, hemolytic anemia (which leads to a low red blood cell count), and a low platelet count (thrombocytopenia). Patients may experience fatigue, pale skin, and small, unexplained bruises or bleeding.
How quickly do symptoms of HUS appear after infection?
Symptoms of HUS typically develop within 5 to 10 days after the onset of diarrhea, often caused by an E. coli infection. However, the timing can vary based on the individual and the severity of the infection.
Can HUS symptoms vary between children and adults?
Yes, symptoms of HUS can vary somewhat between children and adults. Children are more likely to experience severe symptoms like kidney impairment and neurological symptoms such as seizures. Adults might experience milder symptoms initially but can still suffer severe complications like high blood pressure and chronic kidney disease.
What are the less common symptoms of HUS?
Apart from the typical symptoms, some less common symptoms of HUS include severe abdominal pain, vomiting, and sometimes neurological symptoms like confusion, strokes, or seizures, which indicate the severity of the condition.
When should someone seek medical attention for HUS symptoms?
Immediate medical attention should be sought if there are signs of HUS such as bloody diarrhea, extreme fatigue, reduced urine output, or any symptoms of severe anemia and thrombocytopenia. Early intervention is crucial to manage symptoms effectively and prevent severe complications.
Conclusion
In summary, recognizing the symptoms and understanding the causes of Hemolytic Uremic Syndrome (HUS) is crucial for timely and effective treatment. HUS can lead to serious health complications, so it is important to be aware of its primary indicators such as sudden onset of fatigue, reduced urine output, and blood in urine.
Understanding that HUS often follows gastrointestinal infections or is linked to specific strains of E. coli can help in early diagnosis and management. If you or someone you know exhibits symptoms associated with HUS, it is essential to consult a healthcare provider immediately.
Prompt medical attention not only improves the prognosis but also minimizes the potential for severe complications. Always prioritize health and seek professional advice when concerned about symptoms related to HUS.
References
For additional information and to validate the details discussed about Hemolytic Uremic Syndrome symptoms, consider exploring these reputable sources:
- Mayo Clinic – The Mayo Clinic provides a detailed overview of Hemolytic Uremic Syndrome, covering everything from symptoms to diagnosis and prevention strategies. Visit the Mayo Clinic’s HUS page.
- Kidney Foundation – This site offers insights into how Hemolytic Uremic Syndrome affects kidney function and the long-term outlook for patients. Learn more at the Kidney Foundation.
- PubMed Health – For scientific studies and research papers on Hemolytic Uremic Syndrome, PubMed is a valuable resource for in-depth clinical information. Search for HUS studies on PubMed.
These sources are crucial for anyone looking to deepen their understanding of Hemolytic Uremic Syndrome, ensuring access to reliable and up-to-date information.