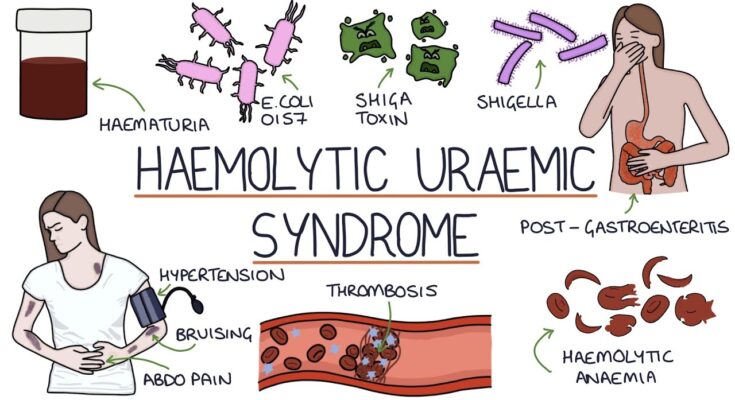
Hemolytic Uremic Syndrome Treatment: Hemolytic Uremic Syndrome (HUS) is a severe, life-threatening condition predominantly affecting the kidneys and the blood’s ability to clot.
This complex syndrome is characterized by the triad of hemolytic anemia, acute renal failure, and thrombocytopenia.
Understanding the pathways to an accurate diagnosis and effective treatment is crucial for patient outcomes.
What is Hemolytic Uremic Syndrome?
Hemolytic Uremic Syndrome (HUS) is a rare but severe condition that primarily affects the kidneys and the blood’s ability to clot. It leads to the destruction of blood cells, a sudden decrease in platelet count, and kidney failure due to damage to the very small blood vessels of the kidneys. Prompt recognition and treatment are crucial to manage the symptoms and prevent long-term damage.
Epidemiology: Who is Most at Risk?
HUS most commonly affects young children between the ages of 1 and 5 years, although it can occur at any age. Certain factors increase the risk, including having a recent upper respiratory or gastrointestinal infection. It’s also more prevalent in individuals who have a weakened immune system, making them more susceptible to infections that can lead to HUS.
The Role of E. coli Infections in Triggering HUS
The primary trigger for HUS is infection with certain strains of E. coli, particularly E. coli O157:H7. These bacteria are typically contracted through contaminated food or water and can cause severe gastrointestinal illness. The toxins produced by these strains of E. coli can damage the lining of blood vessels, leading to the characteristic symptoms of HUS. Understanding the connection between E. coli infection and HUS can help in early diagnosis and treatment, potentially mitigating severe outcomes.
Symptoms and Early Warning Signs of Hemolytic Uremic Syndrome (HUS)
Understanding the symptoms and recognizing the early warning signs are crucial for timely medical intervention.
List of Symptoms of Hemolytic Uremic Syndrome
The symptoms of HUS can vary, but typically include the following:
- Bloody Diarrhea: Often the first sign, occurring within a week of infection with toxin-producing bacteria.
- Abdominal Pain: Severe stomach cramps and discomfort are common.
- Fatigue: A feeling of tiredness or weakness, which may be due to anemia from the destruction of red blood cells.
- Decreased Urine Output: The kidneys may be unable to filter waste, leading to reduced urine production.
- Pale Skin: Resulting from anemia.
- Bruising or Bleeding: Easy bruising or unexplained bleeding can occur due to the low levels of platelets in the blood.
- Fever: Though not always present, some patients may experience a mild fever.
When to Seek Medical Attention
Immediate medical attention is essential if you or someone you know exhibits symptoms of HUS, especially after a recent episode of bloody diarrhea or exposure to a known outbreak of E. coli or other bacteria. Early stages of HUS can quickly progress to more severe complications, making prompt treatment crucial to prevent long-term damage.
Case Studies or Anecdotal Mentions for Real-life Context
- Case Study 1: A 4-year-old child developed severe abdominal pain and bloody diarrhea after consuming undercooked ground beef contaminated with E. coli. Within a week, symptoms progressed to decreased urine output. The child was diagnosed with HUS and received kidney dialysis, highlighting the importance of recognizing early symptoms and seeking prompt care.
- Anecdotal Mention: A woman in her 30s experienced mild flu-like symptoms after eating at a restaurant known to have a recent E. coli outbreak. Initially dismissing her symptoms as a minor stomach upset, she later developed severe anemia and decreased urine output, which led to the diagnosis of HUS. This case underscores the importance of monitoring symptoms following potential exposure to harmful bacteria.
These real-life examples emphasize the necessity of being vigilant about gastrointestinal symptoms, particularly when they are accompanied by signs of potential kidney issues or anemia. If you suspect HUS, contact healthcare providers immediately for the best outcomes.
Diagnostic Procedures for Hemolytic Uremic Syndrome (HUS)
Accurate diagnosis is crucial for timely and effective treatment. Here we discuss the primary diagnostic procedures used to identify HUS, including laboratory tests, imaging tools, and the differential diagnoses necessary to exclude other similar conditions.
Laboratory Tests and Findings Specific to HUS
1. Complete Blood Count (CBC): A CBC is typically the first test conducted, which can show anemia with a low platelet count—hallmarks of HUS.
2. Blood Smear: Examination under a microscope reveals damaged red blood cells (schistocytes or fragmented cells), indicating hemolysis.
3. Kidney Function Tests: Elevated creatinine and blood urea nitrogen (BUN) levels may indicate kidney impairment, a core component of HUS.
4. Stool Test: For HUS cases suspected to be caused by bacterial infections (like E.coli O157:H7), a stool sample may be analyzed to identify the presence of these bacteria.
5. Serum Complement Levels: Since atypical HUS is related to abnormal function of the complement system, measuring the levels of complement proteins helps in distinguishing it from typical, infection-related HUS.
Imaging and Other Diagnostic Tools
While HUS is mainly diagnosed through laboratory findings, imaging tools can be instrumental in assessing the extent of organ damage:
1. Renal Ultrasound: Used to check for kidney size and structure abnormalities that might occur due to HUS.
2. Echocardiogram: Occasionally used if cardiac involvement is suspected, especially in severe cases where the heart’s function may be compromised.
3. MRI or CT Scans: These are less commonly employed but may be used to assess other organs if complications are suspected beyond the kidneys.
Differential Diagnoses to Exclude Other Similar Conditions
Correctly diagnosing HUS involves ruling out other conditions that can present with similar symptoms, such as:
1. Thrombotic Thrombocytopenic Purpura (TTP): Like HUS, TTP also shows thrombocytopenia and hemolytic anemia but typically includes neurological symptoms which are less common in HUS.
2. Disseminated Intravascular Coagulation (DIC): This condition also leads to low platelet count and organ failure, but differs as it involves the widespread activation of blood clotting, which can lead to bleeding issues, unlike HUS.
3. Shiga Toxin-Producing E. coli (STEC) Infection: While STEC infection can lead to HUS, it’s crucial to confirm this as the causative agent through stool tests to ensure appropriate treatment.
4. Atypical Hemolytic Uremic Syndrome (aHUS): This is a rare, genetic variant of HUS that might require different treatment approaches, such as eculizumab, a drug targeting the complement system.
However, these diagnostic procedures play a pivotal role in both confirming the diagnosis of HUS and ruling out other similar conditions, enabling targeted therapeutic strategies.
Treatment Options for Hemolytic Uremic Syndrome
Fortunately, there are several treatment strategies available that can manage symptoms and improve outcomes for patients. Understanding these options is crucial for those diagnosed with HUS, as well as for their healthcare providers.
Current Treatment Strategies
The management of HUS primarily focuses on supportive care, which includes maintaining fluid balance, managing blood pressure, and treating any immediate complications. Here’s a breakdown of the current treatment strategies:
- Fluid Management: Adequate hydration is crucial to help manage HUS. This may involve intravenous fluids to ensure proper hydration and to help flush out toxins from the kidneys.
- Blood Transfusions: These may be necessary to manage anemia and platelet depletion that are common in HUS patients.
- Nutritional Support: Proper nutrition is essential, and in severe cases, nutritional therapy might be required to ensure the patient receives adequate nutrients.
- Medications: Use of medications to control blood pressure, relieve symptoms, and prevent further complications is a common practice in HUS treatment.
These methods aim to stabilize the patient and manage the symptoms until the acute phase of the disease resolves.
Role of Plasmapheresis and Dialysis in Management
For more severe cases of HUS, particularly those that involve significant kidney impairment, treatments like plasmapheresis and dialysis become critical:
- Plasmapheresis: This procedure involves the removal of blood plasma from the body, treating it to remove harmful substances, and then returning it to the patient’s body. This can be beneficial in removing toxins and autoantibodies that contribute to the disease progression.
- Dialysis: When the kidneys are unable to function adequately, dialysis is used to perform the critical functions of the kidneys, such as filtering waste products and excess fluid from the blood.
Both treatments are vital in managing severe cases and can be life-saving interventions.
Emerging Therapies and Clinical Trials
Research into new treatments for HUS is ongoing, and several emerging therapies and clinical trials look promising:
- Complement Inhibitors: Since the overactivation of the complement system—a part of the immune system—is often involved in HUS, drugs that inhibit this system can be effective. Eculizumab, a complement inhibitor, has shown promise in treating atypical HUS.
- Monoclonal Antibodies: These are being explored for their potential to target specific pathways involved in HUS pathogenesis.
- Gene Therapy: Early-stage research into gene therapy suggests potential for addressing the underlying genetic causes of some forms of HUS.
- Clinical Trials: Ongoing clinical trials are crucial for developing and testing new therapies. These trials help determine the efficacy and safety of new treatments, providing hope for future treatment improvements.
Staying informed about these emerging therapies and the availability of clinical trials is essential for patients and healthcare providers alike to ensure access to the most effective and advanced treatment options.
By staying updated with the latest in treatment strategies and emerging therapies, patients with Hemolytic Uremic Syndrome can improve their quality of life and potentially reduce the risk of serious complications associated with this condition.
Management of Complications of Hemolytic Uremic Syndrome (HUS)
Effective management strategies are critical for improving patient outcomes. Here’s a closer look at how these complications are managed and what the long-term outlook looks like.
Recognizing and Managing Acute Renal Failure
Acute renal failure is a common complication of HUS, requiring prompt and effective treatment to prevent long-term damage. The key to management includes:
- Early Diagnosis: Monitoring for signs of reduced urine output, swelling, and elevated blood pressure can help in early identification.
- Supportive Care: This may include fluid management to prevent fluid overload and electrolyte imbalances.
- Renal Replacement Therapy: In cases where kidney function deteriorates significantly, dialysis may be necessary to help remove toxins and excess fluids from the body.
Regular follow-ups are essential to assess kidney function and recovery, adapting the treatment plan as needed to support kidney health.
Treatment Strategies for Neurological Complications
Neurological complications in HUS, although less common, can be severe, including seizures and strokes. Management strategies include:
- Monitoring: Close observation in a hospital setting for any signs of neurological impairment.
- Medications: Use of anticonvulsants to manage seizures and other medications as necessary to reduce the risk of further neurological damage.
- Specialized Care: Access to a neurologist for ongoing assessment and intervention.
Prompt treatment can significantly reduce the risks of long-term neurological damage.
Long-term Outlook and Rehabilitation
The long-term outlook for patients with HUS varies, depending on the severity of the initial illness and the complications that develop. Key aspects of long-term care include:
- Ongoing Assessment: Regular kidney function tests and neurological assessments to monitor recovery or progression of symptoms.
- Rehabilitation Services: Physical, occupational, and speech therapy may be necessary to help those with lasting impairments regain function.
- Educational and Social Support: Resources for patients and families to help them understand the condition and cope with its consequences.
With timely and effective management, many patients recover from HUS with minimal long-term effects, but it’s crucial to have a comprehensive care plan to address any complications that arise.
Implementing these strategies requires a multidisciplinary approach and continuous evaluation to adapt the treatment as the patient’s condition evolves.
Prevention and Risk Reduction of Hemolytic Uremic Syndrome (HUS)
Preventing HUS, especially after outbreaks of E. coli, involves proactive steps and education. Understanding these measures can significantly reduce the risk of developing HUS.
Steps to Prevent HUS Following E. coli Outbreaks
- Monitor Health and Symptoms: After an E. coli outbreak, monitor yourself and your family for symptoms such as severe stomach cramps, diarrhea (often bloody), and vomiting. Early detection and treatment can prevent the progression to HUS.
- Practice Good Hygiene: Frequent and thorough hand washing with soap and water is essential, especially after using the restroom, changing diapers, and before preparing or eating food.
- Cook Meat Thoroughly: Ensure that all meat, particularly ground beef, is cooked to a safe internal temperature of at least 160°F (70°C) to kill E. coli bacteria.
- Avoid Raw Milk and Juices: Unpasteurized milk, dairy products, and juices can carry E. coli. Opt for pasteurized products to reduce the risk of infection.
- Clean and Sanitize Surfaces: Regularly clean surfaces in your kitchen, especially after they come into contact with raw meat or unwashed fruits and vegetables.
Educational Strategies for At-Risk Populations
- Public Health Information Campaigns: These campaigns should focus on spreading awareness about the sources and risks of E. coli infections and the steps to prevent them.
- Schools and Childcare Centers: Education programs in these settings can teach children about the importance of handwashing and safe eating practices.
- Community Workshops: Hosting workshops in local community centers that focus on food safety, personal hygiene, and symptom recognition can help at-risk populations understand how to protect themselves.
The Importance of Hygiene and Safe Food Practices
Maintaining high standards of hygiene and adhering to safe food practices are not just crucial in preventing HUS but are essential for overall health. These practices include:
- Proper Food Handling: Wash hands, utensils, and food surfaces often. Separate raw meats from other foods to avoid cross-contamination.
- Water Safety: Ensure your water is clean and safe to drink. This is particularly important in areas prone to water-borne diseases.
- Public Awareness: Regular updates and reminders about the importance of hygiene can reinforce safe practices and reduce the incidence of HUS.
By integrating these preventive steps and educational strategies into daily routines, individuals and communities can significantly lower their risk of developing Hemolytic Uremic Syndrome. These efforts are especially critical in areas recently affected by E. coli outbreaks, ensuring a healthier future for all.
The Future of Hemolytic Uremic Syndrome Treatment
Hemolytic Uremic Syndrome (HUS) is a serious condition primarily characterized by kidney failure, low platelet count, and destruction of red blood cells. As science progresses, the outlook on treatments for HUS looks promising, particularly with advances in genetic research and personalized medicine.
Research Advancements and Potential Future Treatments
Recent research into HUS has opened the door to innovative treatments that could potentially transform patient care. One of the most exciting developments is the use of targeted therapies that specifically address the underlying causes of HUS, rather than just managing symptoms. For instance, therapies targeting the complement system (a part of the immune system involved in inflammation) have shown potential in treating atypical HUS, which is a rarer form of the condition.
Moreover, biotechnological advancements are facilitating the development of more effective and less invasive diagnostic tools. These tools can help in identifying HUS and its variants more quickly and accurately, allowing for timely and tailored treatment interventions.
The Impact of Genetic Research on Personalized Medicine Approaches
Genetic research is particularly influential in the field of personalized medicine, which tailors medical treatment to the individual characteristics of each patient. For HUS, genetic insights have been crucial in understanding the different subtypes of the syndrome and how they respond to various treatments.
Personalized medicine approaches are expected to be particularly transformative for patients with atypical HUS, where genetic abnormalities play a significant role. By understanding a patient’s genetic profile, healthcare providers can predict the course of the disease more accurately, select the most effective therapies, and adjust treatments based on individual response and tolerance levels.
This shift towards personalized medicine not only promises better treatment outcomes but also reduces the likelihood of adverse side effects, as treatments are specifically designed to align with an individual’s unique genetic makeup.
However, the future of HUS treatment lies in the ongoing integration of advanced genetic research and personalized medical practices. These developments not only aim to provide more effective therapeutic options but also enhance the quality of life for patients suffering from HUS. As research continues to evolve, it holds the promise of bringing more innovative solutions to the forefront of healthcare.
FAQs about Hemolytic Uremic Syndrome Treatment
What is Hemolytic Uremic Syndrome (HUS)?
Hemolytic Uremic Syndrome (HUS) is a severe condition that typically occurs when an infection in the digestive system produces toxic substances that destroy red blood cells. This damage leads to kidney injury and can result in acute kidney failure.
What are the treatment options for HUS?
Treatment for HUS primarily focuses on supportive care, which includes maintaining fluid balance, managing blood pressure, and correcting electrolyte abnormalities. Dialysis may be necessary if there is significant kidney involvement. In some cases, plasma exchange or blood transfusions may also be required.
Can antibiotics be used to treat HUS?
Antibiotics are not generally recommended for treating HUS, especially if it is caused by certain bacteria like E. coli O157:H7, as they may increase the risk of releasing more toxins into the system.
Is there a specific diet recommended during HUS treatment?
Patients with HUS may need a diet that is gentle on the kidneys. This typically involves limiting sodium, potassium, and phosphorus intake. A healthcare provider or a dietitian specializing in kidney health can provide personalized guidance.
How long does recovery from HUS take?
The duration of recovery from HUS can vary significantly depending on the severity of the condition and the organs affected. While some patients may recover kidney function within a few weeks, others may have longer-term effects requiring ongoing management.
Can HUS be prevented?
Preventing HUS involves avoiding the risk factors that lead to infection by harmful bacteria, such as practicing good hygiene, properly handling and cooking meat, and avoiding raw milk and juices. Vaccines are also available for some types of bacteria that can lead to HUS.
Conclusion
In summary, the recognition, diagnosis, and treatment of Hemolytic Uremic Syndrome (HUS) are crucial for preventing its severe outcomes, including kidney failure and other life-threatening complications. This condition, often triggered by an E. coli infection, underscores the importance of vigilant hygiene practices and prompt medical attention.
Continued education and awareness are vital for healthcare professionals and the public to ensure early detection and effective management of HUS. By staying informed about the latest developments in medical research and treatment options, we can better safeguard the health of vulnerable populations, particularly children, who are most at risk. Let us commit to ongoing learning and vigilance in the battle against HUS, enhancing our collective ability to manage and overcome this serious condition.
References
For those seeking further reading and reliable sources on the topic of Hemolytic Uremic Syndrome (HUS) and its treatments, the following references are highly recommended. Each source is reputable and offers valuable insights and validation of the information discussed:
- Centers for Disease Control and Prevention (CDC) – Provides comprehensive guidelines and updates on the management of Hemolytic Uremic Syndrome. Read more about HUS on the CDC website.
- Mayo Clinic – Offers detailed descriptions of symptoms, causes, and treatment options for HUS. This resource is particularly useful for understanding the medical approach to managing this condition. Explore HUS treatments at Mayo Clinic.
- Kidney International – This journal features research articles and case studies on the latest advancements in the treatment of diseases affecting the kidneys, including Hemolytic Uremic Syndrome. Access research articles on HUS from Kidney International.
- National Kidney Foundation – Provides resources and support for patients affected by kidney diseases and related conditions like HUS. They offer educational materials that are helpful for patients and caregivers alike. Visit the National Kidney Foundation for more information on HUS.
These sources are essential for anyone interested in the medical, scientific, and practical aspects of Hemolytic Uremic Syndrome, providing a well-rounded understanding of the condition and its treatment options.