Heart Failure Symptoms: Heart failure, often referred to as congestive heart failure, is a condition where the heart is unable to pump sufficiently to maintain blood flow to meet the body’s needs.
The prevalence of heart failure is increasing globally, making it a critical area of focus for both medical research and public health initiatives.
Understanding Heart Failure
Heart failure is a significant global health concern, affecting millions of people worldwide. It occurs when the heart is unable to pump sufficiently to maintain blood flow to meet the body’s needs. The prevalence of heart failure continues to rise due to aging populations and the increasing prevalence of contributing factors such as coronary artery disease, hypertension, obesity, and diabetes.
Statistics on Prevalence
Recent studies indicate that heart failure affects approximately 26 million people globally, and the numbers are growing. In the United States alone, it is estimated that heart failure affects more than 6 million adults. This condition not only reduces life expectancy but also significantly impacts the quality of life due to its debilitating symptoms.
Impact on Quality of Life
Individuals with heart failure often experience severe physical limitations, which can lead to emotional and psychological distress. Common symptoms include breathlessness, persistent coughing or wheezing, fatigue, and swelling in the legs, ankles, and feet. These symptoms result in decreased ability to exercise, difficulty in performing daily activities, and frequent hospitalizations, which profoundly affect their overall well-being and quality of life.
How the Heart Works Normally vs. in Heart Failure
Normal Heart Function
Under normal conditions, the heart is a powerful muscle that pumps blood throughout the body efficiently. It consists of four chambers: two upper chambers (atria) and two lower chambers (ventricles). Blood flows from the body into the right atrium, then to the right ventricle, which pumps it to the lungs to pick up oxygen. The oxygen-rich blood returns to the left atrium, then to the left ventricle, which pumps it out to the body.
Heart Function During Heart Failure
In heart failure, the heart’s ability to pump blood effectively is compromised. This can be due to weakened heart muscles (systolic heart failure) or stiff and thickened heart muscles (diastolic heart failure), preventing the ventricles from filling properly with blood. As a result, the heart cannot supply sufficient blood to meet the body’s demands, leading to the accumulation of fluid in lungs, liver, around the eyes, and in the legs. This inefficiency can cause the symptoms mentioned above and exacerbates the decline in the patient’s quality of life.
However, understanding heart failure and its impact on daily living is essential for managing the condition effectively and improving outcomes for those affected. Awareness and education on the symptoms and management strategies are crucial for patients and caregivers alike.
Causes of Heart Failure
Understanding these can help in managing and preventing the condition. Here’s a detailed look at the common causes, lifestyle factors, and genetic aspects of heart failure.
Common Causes Leading to Heart Failure
Several medical conditions can lead to heart failure by affecting the heart’s ability to function efficiently:
- Coronary Artery Disease (CAD): The most common cause, CAD occurs when the major blood vessels supplying the heart with blood, oxygen, and nutrients become damaged or diseased. Plaque buildup narrows these arteries, reducing blood flow and leading to heart damage.
- High Blood Pressure (Hypertension): Chronic high blood pressure forces the heart to work harder than normal, which can weaken it over time and contribute to heart failure.
- Heart Attack: A heart attack can damage the heart muscle, affecting its pumping ability and leading to heart failure.
- Cardiomyopathy: This disease of the heart muscle can arise from various causes, including infections, alcohol abuse, and the genetic makeup of an individual, making it harder for the heart to pump blood.
- Valvular Heart Disease: Damage to or a defect in one of the four heart valves may cause the heart to work harder, which can lead to heart failure.
Lifestyle Factors Contributing to Heart Failure Risk
Lifestyle choices play a significant role in the development and progression of heart failure:
- Unhealthy Diet: A diet high in fats, sodium, cholesterol, and sugar can increase the risk of heart disease and heart failure.
- Physical Inactivity: Lack of regular exercise contributes to worsening heart health and other conditions like obesity and high blood pressure, which are risk factors for heart failure.
- Excessive Alcohol Use: Drinking too much alcohol can weaken the heart muscle, leading to cardiomyopathy and subsequent heart failure.
- Smoking: Tobacco use is a major risk factor for heart disease, including heart failure, as it damages the heart and blood vessels.
Genetic Predisposition and Family History
Genetics also play a crucial role in an individual’s risk of developing heart failure. A family history of heart disease can increase the likelihood of conditions such as cardiomyopathy, coronary artery disease, and genetic abnormalities affecting the heart. Genetic testing and counseling can be crucial for families with a history of heart issues to assess risk and take preventive measures.
However, understanding these causes and lifestyle factors is essential for both preventing heart failure and managing it effectively if it develops. Early intervention and lifestyle adjustments can significantly impact the progression of heart failure and improve quality of life.
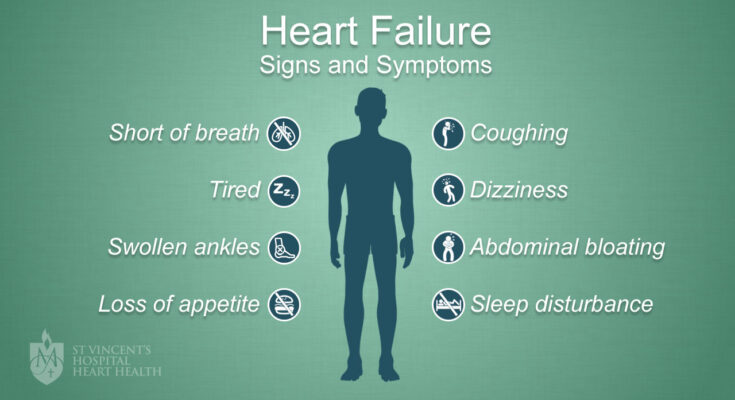
Symptoms of Heart Failure
Recognizing the early symptoms and signs of heart failure is crucial for timely management and treatment. Below, we explore the typical early symptoms of heart failure and how they can impact daily life.
Early Symptoms and Signs of Heart Failure
- Shortness of Breath (Dyspnea): This can occur during activity or while at rest. Some individuals may especially feel breathless while lying flat.
- Persistent Cough or Wheezing: Producing extra mucus, a cough or wheezing that doesn’t go away can be a sign.
- Fatigue: Feeling unusually tired all the time can be one of the first indicators of heart failure.
- Edema (Swelling): Swelling in the feet, ankles, legs, or abdomen is common, due to fluid accumulation.
- Rapid or Irregular Heartbeats: The heart might beat too quickly, which can feel like fluttering or palpitations.
- Lack of Appetite or Nausea: A feeling of being full or sick to your stomach.
- Impaired Thinking or Confusion: Reduced blood flow to the brain can affect thinking and memory.
- Increased Heart Rate: Feeling as if your heart is racing or throbbing.
Impact on Daily Life
These symptoms can severely impact an individual’s quality of life. Shortness of breath may limit your ability to perform simple activities such as walking, climbing stairs, or carrying groceries. Fatigue could make it difficult to engage in any physical activities. Swelling in the limbs might prevent fitting into regular clothes or shoes, and the nausea or lack of appetite can lead to poor nutritional intake. The emotional toll is also significant, as persistent symptoms can lead to anxiety or depression.
Importance of Monitoring Symptoms
Monitoring and recognizing changes in these symptoms are vital. Early detection and treatment can significantly improve the quality of life and potentially slow the progression of heart failure. Regular check-ups, using devices to monitor heart rate and blood pressure, and keeping a symptom diary are practical steps that can help manage the condition effectively.
Patients and caregivers should be educated on the importance of timely recognition of these symptoms and encouraged to seek medical advice if they notice worsening or new symptoms. This proactive approach is essential for managing heart failure effectively.
However, understanding these symptoms and their potential effects on daily life underscores the importance of early detection and active management of heart failure. By staying vigilant and proactive, individuals can better manage their symptoms and improve their overall health outcomes.
Diagnosing Heart Failure
Diagnosing heart failure accurately is crucial for managing the condition effectively. This section delves into the common diagnostic tests and procedures, underscores the importance of medical history and physical examination, and explains how symptoms can indicate the severity of heart failure.
Common Diagnostic Tests and Procedures
Early and accurate diagnosis of heart failure often requires a combination of various tests and procedures. These include:
- Electrocardiogram (ECG): This test records the electrical activity of the heart and can help identify irregular rhythms and areas of damage.
- Echocardiogram: This ultrasound test evaluates the mechanical function of the heart, including chamber size, valve function, and overall cardiac performance.
- Blood Tests: Certain enzymes and hormones in the blood can indicate heart failure. B-type natriuretic peptide (BNP) is a hormone typically elevated in heart failure.
- Chest X-ray: An X-ray can reveal signs of heart enlargement, fluid buildup around the heart and lungs, and other structural abnormalities.
- Cardiac MRI: This imaging test provides detailed images of the heart’s structures and blood vessels, helping in assessing the extent of damage caused by heart failure.
Role of Medical History and Physical Examination in Diagnosis
A thorough medical history and physical examination are foundational to diagnosing heart failure. During the history-taking, physicians inquire about symptoms, family history of heart disease, and risk factors such as hypertension, diabetes, and lifestyle choices. Physical examinations might reveal signs like swollen ankles, an enlarged heart, or abnormal heart sounds which are critical for diagnosing heart failure.
How Symptoms Help in Diagnosing the Severity of Heart Failure
Symptoms play a pivotal role in not only diagnosing heart failure but also in assessing its severity. Some of the symptoms that may indicate severe heart failure include:
- Dyspnea (shortness of breath): Occurs even at rest or wakes the patient during the night.
- Persistent coughing or wheezing: Often accompanied by white or pink blood-tinged phlegm.
- Edema (swelling): Usually in the legs, ankles, and feet due to fluid accumulation.
- Fatigue and weakness: Severe heart failure can make it difficult to perform everyday activities.
- Rapid or irregular heartbeats: Can feel like the heart is racing or throbbing.
By evaluating these symptoms alongside test results, healthcare providers can determine the severity of heart failure, which is crucial for effective treatment planning.
Managing Symptoms of Heart Failure
Heart failure is a chronic condition that requires comprehensive management strategies to improve quality of life and longevity. Here, we explore the lifestyle modifications, medications, and surgical options available to manage symptoms and enhance heart function effectively.
Lifestyle Modifications
Adopting healthier lifestyle habits is foundational in managing heart failure. Here are key changes recommended:
- Dietary Adjustments: Reducing salt intake to less than 2,000 milligrams per day can help minimize fluid retention and lower blood pressure. It’s also important to limit fluid intake as advised by your doctor and focus on a balanced diet rich in fruits, vegetables, and whole grains.
- Regular Physical Activity: Engaging in moderate exercise, as approved by a healthcare provider, can strengthen the heart and improve overall cardiovascular health. Walking, swimming, and light aerobic activities are generally safe and beneficial.
- Weight Management: Maintaining a healthy weight reduces strain on the heart. Regular monitoring can help detect fluid retention early.
- Avoiding Tobacco and Alcohol: Smoking cessation is critical, as tobacco use exacerbates heart failure. Limiting alcohol consumption is also advised to avoid worsening heart conditions.
- Stress Management: Techniques such as yoga, meditation, or gentle exercise can reduce stress, which may adversely affect heart health.
Medications Commonly Used to Manage Symptoms
Medications play a crucial role in managing heart failure by improving heart function and alleviating symptoms. Commonly prescribed medications include:
- ACE Inhibitors (e.g., lisinopril, enalapril): Help widen blood vessels to lower blood pressure, improve blood flow and decrease the workload on the heart.
- Beta-Blockers (e.g., carvedilol, metoprolol): Slow the heart rate and reduce blood pressure, which can improve heart function over time.
- Diuretics (e.g., furosemide, bumetanide): Assist in eliminating excess fluid in the body, reducing symptoms like swelling and shortness of breath.
- Aldosterone Antagonists (e.g., spironolactone, eplerenone): Help regulate the balance of sodium and potassium in the body, and reduce fluid accumulation.
- Digitalis (e.g., digoxin): Increases the force of the heart’s contractions, which can be beneficial in treating heart failure.
Surgical Options and Advanced Treatments for Severe Cases
In severe cases of heart failure, where lifestyle changes and medications cannot fully manage the condition, more advanced treatments and surgeries may be necessary:
- Implantable Cardioverter Defibrillators (ICDs): These devices are surgically placed to monitor heart rhythms and deliver electric pulses or shocks to maintain normal heart rhythm.
- Cardiac Resynchronization Therapy (CRT): This involves placing a special pacemaker that helps the heart chambers beat more in sync, improving the efficiency of the heart’s function.
- Ventricular Assist Devices (VADs): These mechanical devices are used to support heart function and blood flow in individuals with weakened hearts.
- Heart Transplant: In cases where the heart is severely damaged and other treatments have failed, a heart transplant may be considered as a last resort.
Each of these options requires careful consideration and consultation with a healthcare provider to determine the best course of action based on the individual’s specific condition and overall health.
By integrating these management strategies—lifestyle changes, medication, and possibly surgery—individuals with heart failure can lead fuller, more active lives despite their condition.
Preventing Heart Failure
Proactive prevention can dramatically reduce the risk of developing this condition. This article outlines key strategies to prevent heart failure, emphasizing the management of underlying health issues, the importance of regular check-ups, and the benefits of early intervention.
Managing Underlying Conditions: A Cornerstone for Prevention
A critical step in preventing heart failure is the effective management of conditions that could lead to it, such as hypertension (high blood pressure) and diabetes. Both conditions can strain the heart and damage blood vessels over time, leading to heart failure. Managing these conditions involves:
- Monitoring Blood Pressure: Regular checks and maintaining a blood pressure within recommended levels can prevent the heart from working too hard, which would otherwise lead to weakening over time.
- Controlling Blood Sugar Levels: For diabetic patients, it’s crucial to maintain blood sugar levels within target ranges to avoid the damage high sugar levels can cause to the cardiovascular system.
Incorporating lifestyle modifications such as a balanced diet, regular physical activity, and medication adherence plays a pivotal role in controlling these risk factors.
Regular Check-Ups: Early Detection and Intervention
Regular medical check-ups provide an opportunity for early detection and management of signs that might precede heart failure. During these check-ups, healthcare providers can conduct necessary screenings and tests that help in:
- Detecting Changes in Heart Function: Early detection of changes in heart function through regular echocardiograms or other diagnostic tests can be crucial.
- Monitoring Symptoms: Discussing new or worsening symptoms with a doctor can lead to adjustments in treatment before conditions worsen.
Regular interactions with healthcare professionals help in maintaining an overall health plan that prevents the onset of more severe complications.
Early Intervention: Key to Preventing Severe Heart Failure
When potential issues are identified early through regular check-ups, interventions can be more effective, preventing the progression to severe heart failure. This includes:
- Adjusting Medications: Modifying existing medication plans based on evolving health needs.
- Lifestyle Adjustments: Making immediate changes in lifestyle based on medical advice to alleviate stress on the heart.
- Educational Programs: Participating in patient education programs to better understand and manage health conditions that affect the heart.
By taking these steps, individuals can significantly reduce their risk of developing heart failure and maintain a healthier, more active lifestyle.
However, preventing heart failure involves a comprehensive approach focusing on the management of underlying conditions, regular medical check-ups, and timely intervention. By understanding and implementing these preventative measures, individuals can take significant strides in protecting their heart health.
FAQs about Heart Failure Symptoms
What are the common symptoms of heart failure?
Heart failure often presents with several noticeable symptoms. The most common ones include shortness of breath (dyspnea) when exerting yourself or while lying down, fatigue and weakness, and swelling (edema) in your legs, ankles, and feet. Additionally, rapid or irregular heartbeats, persistent cough or wheezing, and swelling of your abdomen may occur.
Can symptoms of heart failure appear suddenly?
Yes, symptoms of heart failure can appear suddenly, in what is known as acute heart failure. This may happen after a heart attack or due to a sudden cardiac event, leading to severe symptoms such as rapid breathing, severe shortness of breath, and a blue tinge to the skin, lips, and nails. Immediate medical attention is necessary in such cases.
Are heart failure symptoms different in men and women?
There can be some differences in heart failure symptoms between men and women. Women are more likely to experience shortness of breath, fatigue, and nausea as prominent symptoms. Men might experience more of the classic symptoms like chest pain. However, both genders can experience any of the symptoms associated with heart failure.
How do heart failure symptoms progress over time?
Heart failure symptoms can worsen over time if the condition is not managed properly. As the heart’s ability to pump effectively decreases, symptoms like fatigue, swelling, and difficulty breathing might increase in severity, impacting daily activities and quality of life.
What should I do if I experience symptoms of heart failure?
If you suspect you’re experiencing symptoms of heart failure, it’s crucial to seek medical advice promptly. Early diagnosis and treatment can improve the management of the condition and help prevent its progression. Keep track of your symptoms, their frequency, and their impact on your daily life to aid in discussions with your healthcare provider.
Conclusion
In summary, recognizing the symptoms of heart failure early is crucial for timely intervention and effective management of the condition. Early detection can significantly improve the quality of life and prognosis for those affected.
If you notice any signs of heart failure, such as persistent coughing, swelling in the legs, fatigue, or difficulty breathing, it is essential to seek advice from healthcare professionals.
Consulting with your doctor can lead to early diagnosis and treatment, which are vital in managing heart failure successfully. Remember, your health is important—don’t hesitate to reach out to a healthcare provider if you experience any concerning symptoms.
References
For those seeking additional information on the symptoms of heart failure or wishing to verify the details provided, the following reputable sources offer comprehensive insights:
- American Heart Association – Explore detailed articles and research on heart failure symptoms and management strategies at American Heart Association.
- Mayo Clinic – The Mayo Clinic provides a robust resource on heart failure, covering symptoms, causes, and treatment options. Visit Mayo Clinic for more information.
- National Heart, Lung, and Blood Institute (NHLBI) – For an in-depth look at heart failure, including the latest research and guidelines, the NHLBI’s official site is a valuable resource. Access it through NHLBI.
- WebMD – WebMD offers easily understandable articles that explain the symptoms of heart failure and how they differ from other conditions. Check out WebMD for user-friendly guidance.
- PubMed Central – For those interested in scientific studies and peer-reviewed articles, PubMed Central provides a wealth of information on heart failure and related topics. Visit PubMed Central to access these resources.
These sources have been chosen for their authority and accuracy in the medical field, ensuring readers receive the most reliable and up-to-date information available.