Heart Failure Treatment: Heart failure is a complex clinical syndrome characterized by the heart’s inability to pump sufficient blood to meet the body’s needs.
Understanding the diagnosis and treatment options for heart failure is crucial for improving patient outcomes and enhancing quality of life.
This comprehensive guide delves into the latest methodologies and treatment strategies, providing valuable insights for both healthcare professionals and patients.
Understanding Heart Failure
Heart failure, a complex clinical syndrome, results from any structural or functional impairment of ventricular filling or ejection of blood. This condition affects millions globally, leading to significant healthcare challenges and research focus on management and prevention strategies.
Global Prevalence and Incidence of Heart Failure
Heart failure affects an estimated 26 million people worldwide, making it a major public health issue with substantial social and economic impacts. The prevalence of heart failure is rising due to aging populations and increasing rates of conditions that predispose individuals to heart failure, such as hypertension, diabetes, and coronary artery disease.
In the United States alone, about 6.2 million adults were living with heart failure between 2013 and 2016, according to the Centers for Disease Control and Prevention (CDC). In Europe, the prevalence is similar, with about 2% of adults experiencing heart failure, a figure that rises to 10% among individuals aged 70 and above.
Emerging data from Asia and Africa suggest increasing trends in heart failure incidence and prevalence, attributed to urbanization, lifestyle changes, and enhanced clinical awareness and diagnostic capabilities. These statistics indicate a growing burden of heart failure globally, necessitating robust health systems and effective disease management protocols.
Types of Heart Failure
Understanding the types of heart failure is crucial for diagnosis and treatment. Heart failure can be classified based on the side of the heart affected or its functional capacity:
- Left-sided heart failure: The most common type, where the left ventricle fails to pump blood efficiently. This leads to fluid buildup in the lungs, causing shortness of breath and respiratory distress.
- Right-sided heart failure: Often a consequence of left-sided failure, it occurs when the right ventricle struggles to pump blood into the pulmonary circulation. Symptoms include swelling in the legs and abdomen due to fluid retention.
- Systolic heart failure: This occurs when the heart muscle cannot contract vigorously, indicating a pumping problem. The hallmark is a reduced ejection fraction.
- Diastolic heart failure: Also known as heart failure with preserved ejection fraction, this type occurs when the heart muscle is stiff and cannot relax properly, hindering its ability to fill with blood during rest.
However, each type of heart failure requires a tailored treatment approach, focusing on lifestyle changes, medication, and in some cases, surgical interventions to manage the disease and improve quality of life.
Causes and Risk Factors of Heart Failure
Understanding these factors is crucial for both prevention and management of the disease. This section delves into the primary contributors to heart failure, highlighting the roles of lifestyle choices, genetic predispositions, and comorbid conditions.
Lifestyle Influences
Lifestyle choices play a pivotal role in the development of heart failure. Key lifestyle factors that significantly increase the risk include:
- Poor Diet: Consuming high-fat, high-sodium, and calorie-dense foods can lead to conditions like obesity and hypertension, which are primary risk factors for heart failure.
- Physical Inactivity: A sedentary lifestyle contributes to the development of cardiovascular diseases by impacting weight, cholesterol levels, and overall heart health.
- Smoking and Alcohol Use: Tobacco use and excessive alcohol consumption directly damage heart muscle and blood vessels, leading to deteriorative changes in heart function.
Adopting a heart-healthy lifestyle, which involves regular physical activity, a balanced diet, and avoiding tobacco and excessive alcohol, can significantly reduce the risk of developing heart failure.
Genetic Factors
Genetics also play a crucial role in the susceptibility to heart failure. Individuals with a family history of heart disease are at a higher risk, suggesting a genetic component to the condition. Genetic disorders like hypertrophic cardiomyopathy (a condition where the heart muscle thickens abnormally) are direct risk factors for heart failure. Advances in genetic testing and personalized medicine are increasingly helping to identify individuals at risk, enabling earlier and targeted interventions.
Comorbid Conditions
Several comorbid conditions can predispose individuals to heart failure, often exacerbating the severity of the disease. These include:
- Hypertension (High Blood Pressure): Puts continuous strain on the heart, leading to wear and tear of the heart muscle.
- Coronary Artery Disease: Occurs when the major blood vessels that supply the heart with blood, oxygen, and nutrients become damaged or diseased.
- Diabetes: Especially when not well-managed, diabetes can contribute to the development of heart failure due to high blood sugar levels causing damage to the cardiovascular system.
- Obesity: Increases the workload on the heart and is often associated with other risk factors like hypertension and diabetes.
Regular check-ups and discussions with a healthcare provider can help individuals understand their personal risk factors and take proactive steps toward heart health.
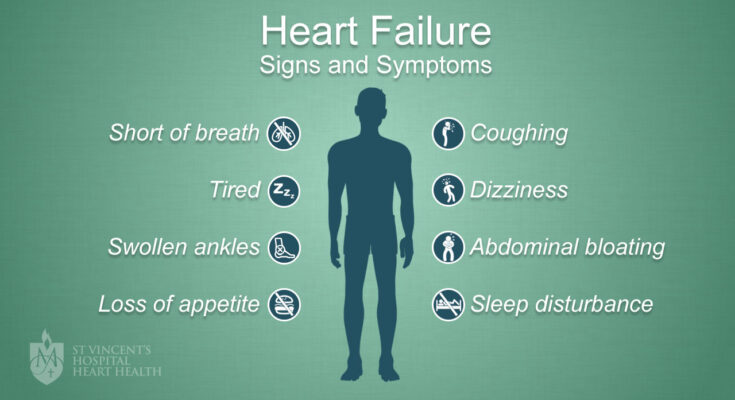
Symptoms of Heart Failure
Below, we discuss the early signs to watch out for, how symptoms can differ depending on the type of heart failure, and when it is essential to seek medical advice.
Early Signs and Symptoms of Heart Failure
The initial symptoms of heart failure might be mild and often overlooked. However, early recognition can significantly influence outcomes. Key symptoms include:
- Shortness of Breath: Often noticeable during activity or while lying down.
- Fatigue and Weakness: Simple activities that were easy before might become challenging.
- Swelling (Edema): Look for swelling in the legs, ankles, and feet, a common early sign.
- Rapid or Irregular Heartbeats: The heart may compensate by beating faster, which can lead to palpitations.
These symptoms arise because the heart struggles to maintain a normal circulatory volume and pressure, leading to congestion and reduced blood output.
Variability of Symptoms Based on Heart Failure Type
Heart failure symptoms can differ significantly depending on whether the failure is primarily on the left side, right side, or both sides of the heart:
- Left-sided Heart Failure: This is the most common type and primarily affects the left ventricle, the heart’s main pumping chamber. Symptoms include persistent coughing or wheezing, shortness of breath, and fatigue.
- Right-sided Heart Failure: This type often results from left-sided failure. It impedes blood flow to the lungs, causing fluid to back up into the venous system, leading to swelling in the extremities and organs.
- Congestive Heart Failure: When both sides are affected, symptoms can include an exacerbated combination of the symptoms of left and right-sided failure, often leading to significant fluid buildup and swelling.
Understanding the specifics of these symptoms can help distinguish the type of heart failure and direct appropriate treatment strategies.
When to Seek Medical Advice
It is crucial to seek medical attention if any symptoms of heart failure are observed, especially if they are new or have worsened. Key instances when one should seek immediate medical advice include:
- Sudden Severe Symptoms: If symptoms like severe shortness of breath, fainting, or chest pain occur, it could indicate acute heart failure or other critical conditions.
- Increasing Symptoms: An increase in the intensity or frequency of symptoms, such as more frequent swelling or episodes of breathlessness, warrants a visit to a healthcare provider.
Prompt medical evaluation can often prevent complications and lead to better management of the condition, potentially improving quality of life and outcomes for individuals with heart failure.
Diagnosing Heart Failure
The diagnosis of heart failure typically begins with a thorough evaluation of medical history and symptoms, followed by a series of diagnostic tests. The process generally includes the following steps:
- Patient History and Symptoms Assessment: Healthcare providers start by gathering detailed information about the patient’s medical history, including any existing health conditions, family history of heart disease, and a comprehensive review of symptoms such as shortness of breath, fatigue, and fluid retention.
- Physical Examination: During the physical exam, a doctor will look for signs of heart failure, including swollen limbs, fluid buildup, and irregular heart sounds.
- Diagnostic Testing: Based on the initial findings, a variety of tests are performed to confirm the diagnosis and assess the severity of the condition.
Key Tests and Procedures Used in Diagnosing Heart Failure
Several diagnostic tests are crucial in confirming heart failure and determining its type and severity. Key tests include:
- Electrocardiogram (ECG): This test records the electrical activity of the heart and helps in identifying irregular heart rhythms, which can be indicators of heart failure.
- Echocardiogram: Often considered the most important test for diagnosing heart failure, it uses ultrasound waves to produce images of the heart, allowing doctors to evaluate the heart’s size, structure, and function.
- Blood Tests: Blood tests check for levels of certain substances in the blood, such as natriuretic peptides, which increase in heart failure. Kidney function and thyroid tests are also commonly conducted.
- Chest X-ray: This test can show the size of the heart and whether there is fluid build-up around the heart and lungs.
- Cardiac MRI or CT Scan: These imaging tests provide detailed images of the heart and can help in assessing the extent of damage caused by heart failure.
The Role of Healthcare Professionals in the Diagnosis of Heart Failure
The diagnosis of heart failure involves a multidisciplinary team of healthcare professionals, each playing a pivotal role:
- Primary Care Physicians initiate the diagnostic process and manage overall patient care.
- Cardiologists specialize in heart diseases and are essential for advanced diagnostics and treatment planning.
- Nurse Practitioners often serve as primary caregivers, providing patient education and ensuring compliance with treatment protocols.
- Radiologists and Technicians perform and interpret the various imaging tests used in diagnosis.
- Laboratory Specialists conduct and analyze blood tests that support the diagnosis.
This team approach ensures comprehensive care, from initial suspicion of heart failure through to a confirmed diagnosis and treatment plan, enhancing the overall management of the condition.
By understanding the diagnostic process, the key tests involved, and the integral role of healthcare professionals, patients can feel more empowered and engaged in their treatment journey.
Treatment Options for Heart Failure
Heart failure, a chronic condition where the heart struggles to pump blood efficiently, requires a comprehensive treatment plan tailored to the individual’s specific needs. The goals of treatment generally focus on improving symptoms, slowing disease progression, and enhancing quality of life. Here, we explore the medical treatments, surgical options, and the vital role of lifestyle changes in managing heart failure.
Overview of Treatment Goals for Heart Failure
The primary objectives in treating heart failure include:
- Alleviating Symptoms: Treatments aim to reduce symptoms such as shortness of breath, swelling, and fatigue to improve daily functioning.
- Optimizing Heart Function: Enhancing the heart’s ability to pump blood effectively is crucial for maintaining adequate body functions.
- Preventing Disease Progression: Slowing or halting the progression of heart failure can significantly impact long-term health outcomes.
- Improving Survival and Quality of Life: Extending life expectancy and improving the quality of life are central goals for patients managing heart failure.
Medical Treatments
Medical treatment for heart failure involves a variety of medications that work in different ways to relieve symptoms and decrease the burden on the heart. These include:
- ACE Inhibitors: Help to relax blood vessels and reduce blood pressure, making it easier for the heart to pump blood.
- Beta Blockers: Slow the heart rate and reduce blood pressure, which decreases the heart’s workload.
- Diuretics: Commonly known as water pills, these help eliminate excess fluid in the body, reducing swelling and fluid buildup in the lungs.
- Aldosterone Antagonists: Assist in preventing salt retention and reducing the risk of worsening heart failure.
- Digitalis: Increases the strength of heart muscle contractions and tends to slow the heartbeat.
Surgical Options
In cases where medication is not sufficient, surgical interventions may be necessary:
- Coronary Bypass Surgery: Improves blood flow to the heart in patients with severe coronary artery disease.
- Heart Valve Surgery: Repairs or replaces valves that are not functioning correctly, helping to ensure blood flows in the right direction through the heart.
- Ventricular Assist Devices (VADs): Mechanical pumps that support heart function and blood flow in individuals with weakened hearts.
- Heart Transplant: Considered when all other treatments have failed and the heart is severely damaged.
The Importance of Lifestyle Changes and Management
Lifestyle changes play a crucial role in managing heart failure, helping to minimize symptoms, and improving overall health. Key lifestyle adjustments include:
- Dietary Modifications: Reducing salt intake to help prevent fluid retention and managing other dietary needs to support overall heart health.
- Regular Physical Activity: Tailored exercise programs improve cardiovascular fitness without overstraining the heart.
- Weight Management: Maintaining a healthy weight reduces the heart’s workload.
- Avoidance of Alcohol and Smoking: Both can worsen heart failure symptoms and are discouraged.
- Regular Monitoring and Check-Ups: Keeping track of heart health and symptoms can help make necessary adjustments to treatment plans promptly.
By combining medical treatments, surgical interventions, and lifestyle modifications, individuals with heart failure can lead more active and fulfilling lives while managing the symptoms and progression of the condition. Regular follow-ups with healthcare providers ensure that treatment remains optimized according to the changing needs of the patient.
Managing Heart Failure
Effective management of heart failure involves a combination of lifestyle modifications, symptom monitoring, and patient education. Here’s a comprehensive guide to each aspect:
Lifestyle Modifications
1. Diet: A heart-healthy diet is crucial for managing heart failure. This includes reducing sodium intake to help manage fluid retention and prevent bloating, a common issue in heart failure patients. Incorporate plenty of fruits, vegetables, whole grains, and lean proteins into your diet, and avoid foods high in saturated fats and cholesterol. Consult a nutritionist for a tailored eating plan that meets your specific needs.
2. Exercise: Regular physical activity can strengthen the heart and improve overall cardiovascular health. However, it’s important for heart failure patients to exercise under medical supervision. Start with low-impact activities like walking or swimming, and gradually increase intensity based on your doctor’s recommendations. Always listen to your body and avoid overexertion.
3. Weight Management: Maintaining a healthy weight is essential for reducing the burden on your heart. Monitor your weight regularly and discuss any significant changes with your healthcare provider. Weight fluctuations might indicate worsening heart failure or other health issues that need immediate attention.
Monitoring and Managing Symptoms at Home
1. Daily Monitoring: Keep a daily log of your symptoms, weight, and overall physical activities. Notable symptoms of heart failure include increased shortness of breath, rapid weight gain (more than 2-3 pounds in a day or 5 pounds in a week), and swelling in the ankles, feet, legs, or abdomen.
2. Fluid Management: Monitoring fluid intake and output is vital. Limit fluid intake as recommended by your doctor, usually around 1.5 to 2 liters per day. Keep track of all fluids consumed to avoid excess intake which can exacerbate heart failure symptoms.
3. Medication Adherence: Take your medications as prescribed and keep a schedule to ensure consistency. Adjustments to medication should only be made under a healthcare provider’s supervision.
The Role of Patient Education in Managing Heart Failure
Education is a cornerstone of effective heart failure management. Understanding the condition helps patients recognize early signs of exacerbation, which is crucial for preventing hospital admissions and complications. Heart failure education should cover:
- Understanding the Disease: Knowing what heart failure is, its causes, and its effects on the body helps patients better manage their condition.
- Recognizing Symptoms: Patients must be able to identify symptoms that indicate worsening heart failure or other complications.
- Self-Care Techniques: Education on diet, exercise, and self-monitoring practices empowers patients to take an active role in managing their health.
Engaging in educational workshops, support groups, or online forums can also provide valuable information and emotional support from others experiencing similar challenges.
However, managing heart failure effectively requires a comprehensive approach that includes lifestyle changes, vigilant symptom monitoring, and ongoing education. By taking an active role in managing their health, individuals with heart failure can significantly improve their life quality and reduce the risk of complications.
Advances in Heart Failure Treatment
Heart failure treatment has undergone significant transformations in recent years, thanks to groundbreaking advancements in medical technology and therapies. This evolution has opened new avenues for managing a condition that affects millions worldwide, improving both the quality of life and survival rates for patients.
Recent Advancements in Medical Technology and Treatment
The latest breakthroughs in medical technology have revolutionized the way heart failure is treated. From sophisticated imaging techniques that provide clearer, more detailed heart views to state-of-the-art devices that help the heart pump more efficiently, these innovations are pivotal. One of the standout developments is the use of wearable technology that monitors heart health in real-time, enabling proactive management of heart failure symptoms and preventing hospital readmissions.
Innovative Therapies and Their Impact on Treatment Outcomes
Emerging therapies have shown promising results in improving the outcomes of heart failure treatment. Advanced pharmacological treatments, such as new classes of medications that work on a molecular level to improve heart function, are now available. Additionally, stem cell and gene therapy represent the cutting edge of research, offering potential cures by addressing the underlying causes of heart failure rather than just its symptoms. These therapies not only enhance the quality of life but also significantly reduce mortality rates associated with heart failure.
The Future of Heart Failure Treatment and Ongoing Research
Looking ahead, the future of heart failure treatment is bright, with ongoing research focusing on more personalized and precise approaches. Scientists are exploring the genetic factors of heart disease to develop tailored treatments that address individual patient profiles, potentially revolutionizing heart care. Moreover, there is a continuous effort to improve existing devices and develop new biotechnological solutions to assist or even replace heart function more effectively and safely.
With each advancement, heart failure treatment becomes more promising, offering hope that future developments will continue to enhance patient care and outcomes. As research progresses, it becomes increasingly important to stay informed about new treatments and technologies that could dramatically alter the landscape of heart health.
FAQs about Heart Failure Treatment
What are the common treatments for heart failure?
Heart failure treatment typically involves a combination of medications, lifestyle changes, and sometimes surgical interventions. Common medications include diuretics to reduce fluid buildup, ACE inhibitors to lower blood pressure, and beta-blockers to decrease heart strain. Lifestyle modifications might include maintaining a heart-healthy diet, regular exercise, and quitting smoking.
Can heart failure be completely cured?
Heart failure is a chronic condition and cannot be completely cured. However, treatments can significantly improve symptoms and quality of life. The focus is often on managing symptoms and preventing the condition from worsening.
What lifestyle changes are recommended for someone with heart failure?
Key lifestyle changes for managing heart failure include following a low-sodium diet, staying physically active within your capacity, managing stress, and avoiding tobacco and excessive alcohol use. Regular monitoring of weight and fluid intake is also crucial to avoid fluid overload.
Is it safe to exercise if you have heart failure?
Exercise is not only safe but recommended for heart failure patients. It should be done under the guidance of a healthcare professional to tailor the type and intensity of exercise to the individual’s specific condition.
How often should someone with heart failure see a doctor?
The frequency of doctor visits can vary based on the severity of the condition and how well it’s being managed. Initially, frequent visits may be necessary. Once stabilized, routine check-ups every 3 to 6 months may suffice, unless new symptoms arise.
Can diet affect heart failure?
Yes, diet plays a crucial role in managing heart failure. A low-sodium diet helps prevent fluid retention and reduce the burden on the heart. Additionally, maintaining a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall heart health.
Conclusion
Recognizing the symptoms of heart failure, ensuring timely diagnosis, and adhering to effective treatment plans are crucial steps in managing this condition effectively. Heart failure can significantly impact quality of life, but with early detection and proper medical care, individuals can lead fuller, more active lives. It is essential for patients and their families to be informed about the signs of heart failure and to seek medical advice promptly when symptoms arise.
Regular check-ups with healthcare providers play a pivotal role in monitoring heart health and adjusting treatment as necessary. By maintaining a proactive approach to health and following medical advice diligently, individuals can better manage heart failure. Always prioritize your health and consult your doctor regularly to stay on top of your heart health.
References
For those interested in further exploring the treatments and management of heart failure, consulting reputable sources can deepen understanding and offer updated information. Below are several resources that provide reliable and comprehensive data on heart failure treatment:
- American Heart Association (AHA) – The AHA offers extensive materials on heart failure management, including medication guidelines, lifestyle recommendations, and treatment updates. Visit their official site here: American Heart Association – Heart Failure.
- Mayo Clinic – Recognized for its detailed patient care information, the Mayo Clinic provides insights into the causes, symptoms, and treatments of heart failure. Check out their resource page: Mayo Clinic – Heart Failure.
- National Heart, Lung, and Blood Institute (NHLBI) – Part of the National Institutes of Health, NHLBI offers in-depth research and education on heart failure. Their resources can be accessed here: NHLBI – Heart Failure.
- Journal of the American College of Cardiology – For those seeking scholarly articles and research studies, this journal features peer-reviewed papers on advanced heart failure treatments. Access their archives at: JACC – Heart Failure.
These resources are intended for those looking to validate information or delve deeper into the topic of heart failure treatment, supporting both patients and healthcare professionals in their continuous learning efforts.