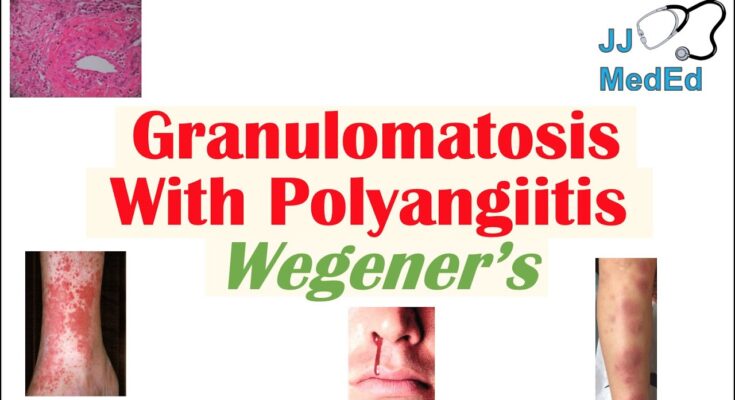
Granulomatosis with Polyangiitis Symptoms: Granulomatosis with Polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare and severe condition that primarily affects the blood vessels of the lungs, kidneys, and respiratory tract.
This systemic disorder is characterized by inflammation, which can lead to significant organ damage if not diagnosed and treated promptly.
Understanding the symptoms and causes of GPA is crucial for early detection and effective management.
What is Granulomatosis with Polyangiitis?
Granulomatosis with Polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare autoimmune disorder characterized by the inflammation of blood vessels, which restricts blood flow to various organs. This condition primarily affects the respiratory tract (sinuses, nose, trachea, lungs) and the kidneys, although it can impact other organs as well. The inflammation can lead to significant tissue damage and is marked by the formation of granulomas, which are clusters of immune cells.
Brief History and Statistics Related to Prevalence
The disease was first described in the 1930s by the German pathologist Friedrich Wegener, who identified it as a distinct pattern of inflammation involving multiple organs. The name was later changed to Granulomatosis with Polyangiitis to more accurately describe its medical characteristics without association to its original namer. The condition is rare, affecting approximately 3 out of every 100,000 people. It can occur at any age but is most commonly diagnosed in adults aged 40 to 65.
Why is GPA a Serious Medical Condition?
GPA is considered a serious medical condition due to its potential to cause rapid and irreversible organ damage if not diagnosed and treated promptly. The disease’s impact on critical organs like the lungs and kidneys can lead to life-threatening complications. Respiratory failure, kidney failure, and systemic inflammation are severe risks without appropriate management. Early and aggressive treatment is crucial and can significantly improve the prognosis, highlighting the importance of awareness and timely medical intervention for those exhibiting symptoms of GPA.
Symptoms of Granulomatosis with Polyangiitis
Recognizing the symptoms of GPA is essential for early diagnosis and effective treatment. This article outlines the symptoms from early onset to advanced stages and discusses how these symptoms can vary from person to person.
Detailed List of Early Symptoms
In the initial stages, the symptoms of GPA might be subtle and often mimic those of more common illnesses, which can make early diagnosis challenging. Here are some of the early symptoms associated with GPA:
- Persistent Sinusitis or Rhinitis: Frequent sinus infections or a chronic runny nose that does not respond to standard treatments.
- Nasal Congestion or Bleeding: Unexplained nasal congestion or nosebleeds can be early signs.
- Cough: A persistent cough that may be dry or might produce phlegm.
- Fever: Low-grade fevers that seem to have no apparent cause.
- Fatigue: General feeling of tiredness and malaise that doesn’t improve with rest.
- Joint Pain: Mild joint pain and stiffness without significant swelling.
- Eye Discomfort: Symptoms like redness, burning, or pain in the eyes.
Signs of Advanced Granulomatosis with Polyangiitis
As GPA progresses, the symptoms become more severe and more organs may be involved. Advanced symptoms include:
- Skin Lesions: Red or purple rashes, often on the limbs, that might develop into open sores.
- Kidney Involvement: Blood in the urine or other signs of kidney dysfunction, which can lead to kidney failure if untreated.
- Neurological Issues: Numbness, weakness, or tingling in various parts of the body.
- Severe Respiratory Problems: Shortness of breath, chest pain, or coughing up blood, indicating lung involvement.
- Ear Infections: Severe, recurrent ear infections that may lead to hearing loss.
- Eye Problems: Severe and worsening eye conditions like scleritis or episcleritis that can threaten vision.
Variation of Symptoms from Person to Person
The symptoms of GPA can vary significantly among individuals, influenced by the severity of the condition and the organs involved. For some, the disease may progress rapidly, leading to severe symptoms quickly, while others might experience a more gradual onset. The range of symptoms can also vary widely; some patients may experience mostly respiratory symptoms, while others may have more pronounced kidney or skin involvement.
This variation underscores the importance of personalized medical attention and treatment plans tailored to the specific manifestations of the disease in each individual.
If you or someone you know is experiencing symptoms similar to those described above, it is vital to seek medical advice for further evaluation and appropriate management.
Causes and Risk Factors of Granulomatosis with Polyangiitis (GPA)
The exact causes of GPA remain somewhat elusive, but scientific research suggests a combination of genetic and environmental factors play a role in its development.
Scientific Understanding of What Causes GPA
At its core, GPA is an autoimmune condition, which means it occurs when the immune system mistakenly attacks the body’s own tissues. In the case of GPA, the immune system targets the blood vessels. Researchers believe that an initial immune response may become abnormally sustained or uncontrolled, leading to chronic inflammation and the characteristic granulomas—masses or nodules of inflammatory cells—that define the disease.
Genetic and Environmental Factors That Might Increase Risk
Genetic Factors: Studies have identified certain genetic markers that may increase susceptibility to GPA. For instance, variations in the genes that regulate the immune system, such as those involved in the production of antibodies, could predispose individuals to develop autoimmune disorders, including GPA.
Environmental Factors: Environmental triggers are also believed to contribute to the onset of GPA. These may include:
- Infections: Some evidence suggests that bacterial or viral infections could trigger the immune system in a way that precipitates autoimmune reactions.
- Silica Exposure: Occupational exposure to silica dust has been linked with an increased risk of developing GPA.
- Hygiene Hypothesis: There’s some speculation that overly sterile environments in childhood could impair immune system development, potentially leading to heightened risks of autoimmune diseases.
Discussion of Autoimmune Aspects of the Disease
The autoimmune nature of GPA is a critical aspect of both its onset and progression. Normally, the immune system serves to protect the body from pathogens and foreign substances. However, in autoimmune diseases like GPA, the immune system’s recognition mechanisms fail, leading to attacks on healthy tissue. In GPA, this autoimmune attack primarily targets the small to medium-sized blood vessels, causing vasculitis—vessel wall inflammation.
This inflammation can lead to a range of symptoms depending on the organs affected, such as the kidneys, lungs, and upper respiratory tract. The autoimmune response in GPA is complex and involves various components of the immune system, including antibodies known as ANCA (antineutrophil cytoplasmic antibodies) which specifically target certain proteins within neutrophils, a type of white blood cell. These ANCAs are considered a hallmark of the disease and are used as a diagnostic marker.
However, understanding the causes and risk factors of GPA is crucial for developing targeted treatments and managing the disease effectively. Ongoing research continues to explore these aspects, aiming to uncover more precise interventions that can modulate the immune system’s response and provide relief to those suffering from this challenging condition.
Diagnosing Granulomatosis with Polyangiitis
Accurate diagnosis is crucial for effective management of the condition. This section explores common diagnostic tests and procedures, highlights the importance of early diagnosis, and discusses the role of medical history and physical examination in detecting GPA.
Common Diagnostic Tests and Procedures
Diagnosing GPA involves a combination of tests and procedures that help identify the characteristic signs of vessel inflammation and organ involvement:
- Blood Tests: Comprehensive blood panels are conducted to check for elevated levels of antibodies typical of GPA, such as antineutrophil cytoplasmic antibodies (ANCA). These tests also help rule out other conditions by assessing inflammation levels through ESR (erythrocyte sedimentation rate) and CRP (C-reactive protein) tests.
- Urine Tests: Urinalysis is crucial for detecting protein and red blood cells in the urine, which indicate kidney involvement—a common complication of GPA.
- Imaging Tests: Chest X-rays, CT scans, and MRIs can reveal the presence of nodules, cavities, or other abnormalities in the lungs and sinuses, which are frequently affected by GPA.
- Biopsy: A tissue biopsy, often taken from the nasal passage, lungs, or kidneys, can confirm the presence of granulomas and vasculitis, which are hallmarks of the disease.
- Endoscopy: For patients experiencing sinus or respiratory symptoms, an endoscopy might be performed to directly visualize the upper airways and check for inflammation and damage.
Importance of Early Diagnosis in Managing Symptoms
Detecting GPA at an early stage can significantly influence the outcome for patients. Early diagnosis allows for the initiation of treatment before irreversible organ damage occurs. Prompt treatment can reduce the severity of symptoms, help in the management of the disease, and improve the overall prognosis. Additionally, early intervention can prevent complications such as kidney failure and respiratory distress, which are associated with advanced GPA.
Role of Medical History and Physical Examination
A thorough medical history and physical examination are foundational in the diagnostic process of GPA. During the initial assessment, healthcare providers will:
- Review Medical History: Discuss symptoms, the duration and pattern of their occurrence, and any family history of similar diseases.
- Physical Examination: Look for signs of inflammation and damage in the nasal passages, lungs, kidneys, and other organs potentially affected by GPA. Special attention is given to skin, joints, eyes, and ear conditions.
Physicians may also assess the patient’s neurological status as GPA can affect the nervous system, presenting with symptoms such as numbness or weakness.
However, early recognition and treatment are paramount in managing this complex and potentially life-threatening condition effectively. Regular follow-ups and monitoring are essential to adjust treatment plans and manage relapses, ensuring patients with GPA maintain a high quality of life.
Treatment Options for Granulomatosis with Polyangiitis
Understanding the treatment options is crucial for managing symptoms and improving patient outcomes. Here, we explore the current treatment modalities, commonly used medications, and promising areas of emerging treatments and research.
Current Treatment Modalities
The primary goal in treating GPA is to induce and maintain remission. Treatment modalities often involve a combination of medications tailored to the severity of the disease and the organs involved. The main strategies include:
- Corticosteroids: These are used to quickly reduce inflammation.
- Immunosuppressants: These help control the immune system to prevent it from attacking healthy body tissue.
- Plasma Exchange (Plasmapheresis): This procedure removes antibodies from the blood and is used in severe cases.
- Biologic Therapies: These target specific parts of the immune system to control inflammation without broad immunosuppression.
Medications Commonly Used
Several medications are fundamental in treating GPA, and they are often used in combination to achieve the best results:
- Corticosteroids (such as Prednisone): These drugs are the first line of defense in reducing acute inflammation.
- Cyclophosphamide: An immunosuppressant that has been the cornerstone of GPA treatment, especially for severe disease.
- Rituximab (Rituxan): This biologic agent is increasingly preferred over cyclophosphamide for inducing remission.
- Methotrexate: Often used for maintenance therapy to keep the disease in remission once the acute phase is under control.
- Azathioprine (Imuran): Another common choice for maintenance therapy.
Emerging Treatments and Research
As research continues, new treatments are being explored to improve safety and efficacy for GPA patients. Emerging therapies focus on better targeted immunomodulation with fewer side effects. Some of the promising areas include:
- New Biologics: Agents like mepolizumab, which targets specific immune cells (eosinophils), are under investigation.
- Janus Kinase (JAK) Inhibitors: These small molecule drugs, which affect signaling pathways in the immune system, are being studied for their potential use in GPA.
- Stem Cell Transplantation: In cases resistant to traditional therapies, stem cell transplantation is being explored as a method to ‘reset’ the immune system.
Additionally, ongoing clinical trials aim to refine the use of existing drugs and explore combination therapies to maximize efficacy and minimize side effects.
Staying informed about the latest treatment strategies and ongoing research is essential for healthcare providers managing this complex condition.
Living with Granulomatosis with Polyangiitis
Living with Granulomatosis with Polyangiitis (GPA), formerly known as Wegener’s Granulomatosis, can be challenging. However, adopting specific lifestyle changes and home remedies can help manage symptoms and improve your quality of life. Here are some practical tips:
- Maintain a Balanced Diet: Nutrition plays a crucial role in managing inflammation and overall health. Include a variety of fruits, vegetables, lean proteins, and whole grains in your diet. Limit the intake of processed foods, sugars, and saturated fats.
- Regular Exercise: While it’s important to tailor activities to your energy levels and symptoms, regular exercise such as walking, swimming, or yoga can improve physical function and alleviate stress.
- Adequate Rest: Ensure you get enough sleep. Rest is essential for your body to recover and heal. Consider creating a relaxing bedtime routine to help manage fatigue.
- Avoid Smoking: Smoking can exacerbate symptoms and negatively impact your overall health. If you smoke, seek help to quit.
- Monitor Your Health: Keep regular appointments with your healthcare provider to monitor your condition and adjust treatments as necessary.
Managing Symptoms and Maintaining Quality of Life
Effective symptom management is key to maintaining a good quality of life with Granulomatosis with Polyangiitis. Here’s how you can manage various symptoms:
- Nasal Care: For nasal and sinus symptoms, use saline nasal sprays or rinses to keep your nasal passages moist and reduce discomfort.
- Skin Care: Use gentle, hypoallergenic products to care for your skin, particularly if you have skin lesions.
- Eye Care: Regular check-ups with an ophthalmologist are important, especially if you experience symptoms like redness, burning, or vision changes.
- Mental Health: Chronic illnesses can be taxing mentally as well as physically. Don’t hesitate to seek professional help if you feel overwhelmed.
Importance of Support Groups and Counseling
Connecting with others who understand what you’re going through can be immensely beneficial. Support groups for people with Granulomatosis with Polyangiitis provide a platform to share experiences, tips, and emotional support. These groups can be found online or may be organized by local hospitals and health organizations.
Counseling is another vital resource. Professional counselors or therapists who specialize in chronic illness can help you develop strategies to cope with the emotional and psychological challenges of living with GPA. They can provide tools to manage stress, anxiety, depression, and other mental health issues associated with chronic diseases.
Living with Granulomatosis with Polyangiitis requires careful management of your health, but with the right strategies and supports, you can maintain an active and fulfilling life. Remember, you’re not alone in this journey, and there are many resources and supportive communities to help you along the way.
FAQs about Granulomatosis with Polyangiitis Symptoms
What is Granulomatosis with Polyangiitis (GPA)?
Granulomatosis with Polyangiitis, formerly known as Wegener’s Granulomatosis, is a rare autoimmune disorder characterized by inflammation of the blood vessels, which can restrict blood flow and damage vital organs and tissues.
What are the common symptoms of GPA?
GPA primarily affects the respiratory system, kidneys, and ears. Common symptoms include persistent sinusitis, nosebleeds, shortness of breath, and a general feeling of being unwell. Kidney involvement can lead to blood in the urine and other urinary symptoms.
How does GPA affect the lungs and breathing?
In the lungs, GPA can cause coughing, wheezing, and shortness of breath. These symptoms result from inflammation and damage to the airways and lung tissues, potentially leading to respiratory infections or pulmonary nodules.
Can GPA symptoms appear suddenly?
Yes, symptoms of GPA can appear suddenly and be quite severe, or they can develop gradually over time. Early diagnosis and treatment are crucial to managing the disease effectively and preventing complications.
Are there specific symptoms that indicate a severe form of GPA?
Severe forms of GPA may manifest as rapid kidney failure, severe lung disease, or involvement of the nervous system, which can include symptoms like numbness or weakness. Prompt medical attention is necessary if these severe symptoms occur.
How are the symptoms of GPA managed or treated?
Treatment typically involves medications to reduce the immune system’s activity, like corticosteroids and immunosuppressants. These treatments aim to reduce inflammation, manage symptoms, and prevent further organ damage.
Is there a cure for GPA?
While there is no cure for GPA, effective management and treatment can lead to remission, where the disease is inactive and symptoms are absent. Regular follow-ups with healthcare providers are essential to monitor for any signs of relapse.
Conclusion
Understanding the symptoms and causes of Granulomatosis with Polyangiitis (GPA) is crucial for early detection and effective management of this complex condition. GPA, a rare autoimmune disorder, can significantly impact various organs, making timely medical intervention essential.
If you or someone you know exhibits symptoms such as persistent nasal congestion, cough, or unusual fatigue, it’s important to consult healthcare professionals. They can provide a thorough diagnosis and tailor a treatment plan that best suits the needs of the individual.
Remember, early diagnosis and professional medical advice are key to managing GPA effectively and improving the quality of life for those affected.
References
For those seeking more detailed information or looking to validate the symptoms associated with Granulomatosis with Polyangiitis (GPA), the following resources are highly recommended. These references have been selected for their credibility and comprehensive coverage of the topic:
- Mayo Clinic – Provides an in-depth overview of the symptoms, causes, and treatment options for Granulomatosis with Polyangiitis. This resource is ideal for patients looking for a trustworthy medical perspective. Read more about GPA on Mayo Clinic.
- National Health Service (NHS) – The NHS offers a detailed description of GPA, including common symptoms and advice on when to seek medical advice. Their guidance is grounded in public health expertise. Explore NHS resources on GPA.
- American College of Rheumatology – Offers comprehensive information on diagnosis and management of Granulomatosis with Polyangiitis, making it a valuable resource for both patients and healthcare professionals. Visit the American College of Rheumatology.
- MedlinePlus – A service of the U.S. National Library of Medicine, MedlinePlus provides accessible, peer-reviewed information on GPA symptoms and treatments. Learn more about GPA on MedlinePlus.
Each of these sources is well-regarded in the medical community and offers readers a wealth of information on Granulomatosis with Polyangiitis, enhancing their understanding and ability to manage this complex condition.