Granulomatosis with Polyangiitis Treatment: Granulomatosis with Polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare but severe autoimmune disease that primarily affects the respiratory tract and the kidneys.
Understanding its diagnosis and treatment is crucial for managing this potentially life-threatening condition.
Understanding Granulomatosis with Polyangiitis
Granulomatosis with Polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare autoimmune disease characterized by inflammation of blood vessels (vasculitis) that can restrict blood flow to various organs. The inflammation primarily affects the respiratory tract and the kidneys, leading to a range of health issues.
Epidemiology: Who is Most Affected?
GPA is quite rare, affecting about 3 out of every 100,000 people in the United States. It can occur at any age but is most commonly diagnosed in adults aged 40 to 65. While it can affect individuals of any ethnic background, it appears more frequently in Caucasians. Both men and women are equally likely to develop the condition.
Brief Discussion on Causes and Risk Factors
The precise causes of GPA remain unknown, but a combination of genetic and environmental factors is suspected to play a role. Possible risk factors include exposures to certain types of dust, silica, and other environmental pollutants, although no direct causation has been definitively established. Some researchers believe that infections could trigger the autoimmune response in genetically susceptible individuals, but this theory has not been conclusively proven.
However, understanding GPA requires a multifaceted approach, considering its rare nature and the complexity of its symptoms and progression. Early diagnosis and treatment are critical for managing the disease and improving patient outcomes.
Symptoms of Granulomatosis with Polyangiitis
Recognizing the symptoms early is crucial for prompt diagnosis and treatment, potentially preventing severe complications. Here, we outline the common symptoms of GPA, differentiate them from symptoms of similar conditions, and underscore the importance of early detection.
Common Symptoms of Granulomatosis with Polyangiitis
GPA can affect various organ systems, leading to a wide range of symptoms that may vary significantly among patients. However, some common symptoms include:
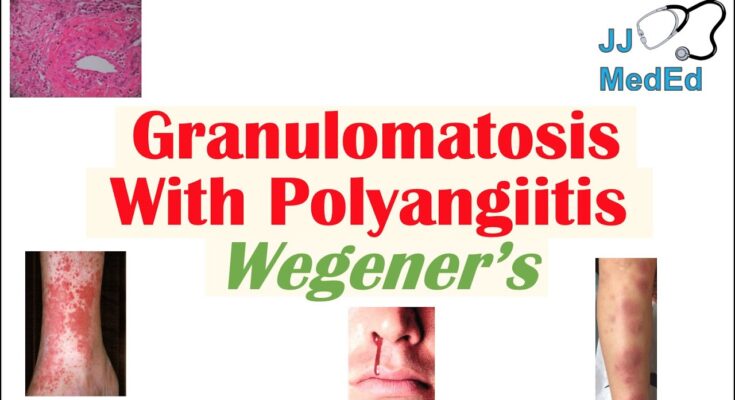
- Nasal or Sinus Symptoms: Chronic sinusitis, nosebleeds, and nasal congestion or deformity.
- Respiratory Issues: Persistent cough, often with bloody sputum, and shortness of breath.
- Renal Involvement: Blood in urine or proteinuria, which may indicate kidney involvement, a serious complication of GPA.
- Joint Pain: Arthralgia or arthritis can occur, causing pain and swelling in joints.
- Eye Problems: Redness, burning, or pain in the eyes, vision problems, and proptosis (protrusion of one or both eyes).
- Skin Lesions: Rashes, ulcers, and necrotic lesions that are often painful and can appear anywhere on the body.
- Neurological Symptoms: Numbness, weakness, or tingling in various parts of the body, due to nerve damage.
Differentiating Symptoms from Similar Conditions
GPA can mimic symptoms of other diseases, making diagnosis challenging. Conditions such as lupus, rheumatoid arthritis, and other types of vasculitis like microscopic polyangiitis and Churg-Strauss syndrome share overlapping symptoms, such as joint pain, kidney problems, and nasal or sinus issues. However, the combination of respiratory, renal, and systemic symptoms like necrotic skin lesions and eye problems are more characteristic of GPA. Moreover, GPA’s symptoms typically include a more pronounced respiratory involvement with symptoms like bloody sputum and more severe nasal deformity.
Importance of Early Symptom Recognition
Recognizing the early signs of GPA is essential for timely diagnosis and treatment. Early intervention can significantly improve outcomes by preventing irreversible damage to vital organs like the kidneys and lungs. Due to the non-specific nature of early symptoms and their similarity to those of more common diseases, GPA can often be overlooked or misdiagnosed. Patients experiencing a combination of respiratory, renal, and systemic symptoms should seek medical evaluation, particularly if symptoms persist or worsen despite initial treatments for more common illnesses.
Early diagnosis typically involves a combination of clinical evaluation, blood tests (such as ANCA testing), imaging studies, and sometimes tissue biopsy, which can confirm the presence of granulomas and vasculitis—hallmarks of the disease.
By being vigilant about the early symptoms of GPA and seeking prompt medical advice, patients can significantly improve their prognosis and manage the condition more effectively.
Diagnosing Granulomatosis with Polyangiitis
The diagnosis of GPA primarily hinges on a combination of clinical presentation, specific laboratory tests, and imaging studies. According to the American College of Rheumatology, criteria for diagnosing GPA include:
- Nasal or oral inflammation: Development of painful or purulent nasal discharge or ulcers.
- Abnormal chest X-ray: Showing the presence of nodules, fixed infiltrates, or cavities.
- Urinary sediment: Microhematuria (blood in urine) or red cell casts in urine tests.
- Granulomatous inflammation: Histological examination from biopsy showing granulomatous inflammation within the wall of an artery or in the perivascular or extravascular area.
A patient typically must meet at least two of these criteria for a probable diagnosis of GPA, coupled with clinical findings that suggest vasculitis.
Tests and Procedures Involved in Diagnosing GPA
The diagnosis of GPA involves various tests and procedures to confirm the presence of the disease and assess its severity:
- Blood Tests: These include tests for C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) to detect inflammation. Additionally, ANCA (antineutrophil cytoplasmic antibodies) tests are crucial as they are often present in patients with GPA.
- Imaging Tests: Chest X-rays and CT scans help identify lung abnormalities. MRI and CT scans of sinuses can detect sinusitis and other upper respiratory tract involvement.
- Biopsy: A tissue biopsy from affected sites such as the lungs, kidneys, or nasal mucosa is often definitive in diagnosing GPA. The biopsy is examined for evidence of granulomatous inflammation.
- Urine Analysis: To check for kidney involvement by detecting proteins and red blood cells in the urine.
Challenges in Diagnosing GPA and How to Overcome Them
Diagnosing GPA poses several challenges due to its rarity and the variability of symptoms among patients. Here are some challenges and strategies to overcome them:
- Overlap of Symptoms: GPA symptoms can mimic those of other diseases such as infections, cancer, and other types of vasculitis. To differentiate GPA from these conditions, comprehensive testing and a detailed patient history are essential.
- Limited Availability of ANCA Tests: In some regions, ANCA testing, a key diagnostic tool for GPA, might not be readily available. Establishing partnerships with larger medical centers can help in such cases.
- Biopsy Risks: Biopsies, especially of lung tissue, can be risky and may not always be feasible. Utilizing less invasive tests such as CT scans or MRIs can provide preliminary insights before proceeding to biopsy.
Efficiently diagnosing GPA requires a multidisciplinary approach involving rheumatologists, nephrologists, and pulmonologists, among others, to ensure comprehensive care and management of the disease.
By understanding the diagnostic criteria, necessary tests, and the challenges involved, healthcare providers can enhance their diagnostic accuracy for Granulomatosis with Polyangiitis, leading to better patient outcomes.
Treatment Options for Granulomatosis with Polyangiitis
Understanding the treatment options available and the necessity of personalized treatment plans is crucial for managing this complex condition effectively.
Current Treatment Modalities
The treatment of GPA primarily focuses on controlling the immune system’s abnormal response, thereby reducing inflammation and preventing organ damage. The approach to treatment often depends on the severity of the disease and the organs involved. Here’s an overview of the current treatment modalities:
- Corticosteroids: Prednisone, a type of corticosteroid, is commonly used to reduce inflammation rapidly. It is often the first line of treatment in managing acute symptoms of GPA.
- Immunosuppressants: Medications like cyclophosphamide and methotrexate help control the disease’s progression by suppressing the immune system. These drugs are crucial for patients who do not respond adequately to steroids alone.
- Biologics: Rituximab, a monoclonal antibody, is approved for treating GPA and has become a key component of therapy, especially for patients who relapse or do not tolerate traditional immunosuppressants. This medication targets specific parts of the immune system to prevent inflammation.
- Plasma Exchange: For severe cases of GPA where there is significant kidney involvement, plasma exchange (plasmapheresis) may be used. This process involves removing blood plasma containing harmful antibodies and replacing it with fresh plasma or a plasma substitute.
- Maintenance Therapy: Once remission is achieved, maintenance therapy using less aggressive drugs like azathioprine or mycophenolate mofetil is crucial to prevent relapses. This phase of treatment can last for several years.
Importance of Personalized Treatment Plans
Personalized treatment plans are vital in managing GPA due to the disease’s variability in symptoms and severity among patients. Here’s why individualized care is essential:
- Tailored to Specific Needs: Each patient’s manifestation of GPA can vary significantly—some may experience primarily respiratory symptoms, while others might have more severe kidney involvement. Treatment must be customized to address these specific needs effectively.
- Adjustments Over Time: As the disease progresses or goes into remission, treatment strategies need to be adjusted. Personalized plans allow for flexibility to increase or decrease medication dosages, switch treatments, or incorporate new therapies based on how the disease responds.
- Mitigating Side Effects: Many treatments for GPA, particularly immunosuppressants and biologics, can have significant side effects. A personalized approach helps balance the effectiveness of the treatment with minimizing adverse effects, improving the patient’s quality of life.
- Comprehensive Care Coordination: Effective management of GPA often requires a multidisciplinary approach, involving rheumatologists, nephrologists, and other specialists. Personalized treatment plans ensure all aspects of a patient’s health are considered and managed cohesively.
However, the treatment of Granulomatosis with Polyangiitis involves a range of therapies tailored to the severity and specifics of each case. A personalized treatment plan, designed and adapted to each patient’s unique needs, is essential for effective disease management and enhancing quality of life.
Managing Life with Granulomatosis with Polyangiitis
Living with Granulomatosis with Polyangiitis (GPA), formerly known as Wegener’s Granulomatosis, can be challenging, but with the right strategies and support, patients can manage their symptoms and maintain a good quality of life. Here’s how to navigate life with GPA focusing on lifestyle adjustments, the importance of regular monitoring, and accessing support systems.
Lifestyle Changes and Home Remedies
Adopting a Healthy Diet: A well-balanced diet can help manage inflammation and support immune function. Include plenty of fruits, vegetables, whole grains, and lean proteins, while limiting processed foods and sugars. Some patients may benefit from a consultation with a dietitian to address specific nutritional needs.
Regular Exercise: Engaging in regular physical activity can improve overall health and help alleviate symptoms like fatigue. However, it’s important to tailor your exercise routine to your current health status and physical abilities. Low-impact exercises such as walking, swimming, or yoga can be particularly beneficial.
Avoiding Infections: Since GPA can impact the immune system, it’s crucial to minimize infection risks. Frequent handwashing, avoiding crowded places during flu season, and staying up-to-date with vaccinations can help protect your health.
Stress Management: Chronic illness can be stressful. Techniques such as mindfulness, meditation, and deep breathing exercises can help manage stress levels. Consider joining a support group or seeking professional counseling to navigate the emotional challenges of living with GPA.
Importance of Follow-Up and Regular Monitoring
Routine Check-Ups: Regular visits to your healthcare provider are essential for monitoring the activity of the disease and the effects of medications. These check-ups typically involve blood tests, urine tests, and assessments of organ function to detect any signs of disease activity or treatment side effects.
Medication Management: Staying on top of medications is crucial. Be consistent with your treatment regimen and discuss any side effects with your doctor. Adjustments to your medication might be necessary over time based on your symptoms and test results.
Watch for Changes in Symptoms: Be vigilant about new symptoms or changes in your condition. Early detection of flare-ups can significantly impact the effectiveness of your treatment.
Support Systems and Resources for Patients and Caregivers
Finding Support Groups: Connecting with others who understand what you’re going through can be invaluable. Look for local or online support groups for people with GPA or related conditions.
Educational Resources: Educate yourself and your caregivers about GPA. Reliable sources such as the Vasculitis Foundation offer extensive information on the disease, treatment options, and living with a chronic illness.
Utilizing Caregiver Resources: Caregivers also need support. Resources like counseling, respite care, and local support services can help caregivers manage their responsibilities and maintain their well-being.
Managing life with Granulomatosis with Polyangiitis involves regular medical care, lifestyle adjustments, and leveraging support networks. By taking proactive steps and utilizing available resources, patients and caregivers can face the challenges of GPA more effectively and lead fulfilling lives.
Prognosis and Quality of Life for Granulomatosis with Polyangiitis
Understanding the prognosis and the impact of treatment can help patients and caregivers manage expectations and improve their quality of life. This section will explore the factors that influence prognosis, what patients can expect in the long term, and how treatment can affect their quality of life.
Factors Affecting the Prognosis of Granulomatosis with Polyangiitis
The prognosis of GPA can vary widely among patients and depends on several key factors:
- Disease Severity and Spread: Patients with limited disease involvement tend to have a better prognosis than those with widespread organ involvement, particularly when major organs like the kidneys are affected.
- Response to Treatment: Early diagnosis and prompt treatment significantly improve outcomes. The effectiveness of the initial treatment regimen can also influence long-term health.
- Relapses: GPA is marked by periods of remission and relapses. Frequent relapses can affect the overall prognosis by causing cumulative organ damage over time.
- General Health and Comorbid Conditions: Overall health, age, and the presence of other medical conditions can impact survival rates and quality of life in patients with GPA.
What Patients Can Expect in the Long Term
Living with GPA involves navigating a variety of challenges and adjustments over the long term:
- Monitoring and Management: Regular medical check-ups are crucial to monitor the activity of the disease and adjust treatments as necessary.
- Chronic Symptoms: Some patients may experience persistent symptoms like fatigue and joint pain, even during periods of remission.
- Lifestyle Adjustments: Patients often need to make lifestyle changes to accommodate their condition, including dietary modifications, regular exercise, and possibly changes in work or social activities to manage fatigue and other symptoms.
Impact of Treatment on Quality of Life
Treatment for GPA generally involves medications to control the immune system’s activity and prevent inflammation. The impact of these treatments on quality of life can be significant:
- Medication Side Effects: While medications like corticosteroids and immunosuppressants are effective in controlling the disease, they can also have side effects that affect quality of life, such as weight gain, increased infection risk, and mood changes.
- Improved Symptoms: Effective treatment can lead to significant improvements in symptoms and functionality, enhancing quality of life and allowing patients to engage more fully in daily activities.
- Psychological Impact: The diagnosis and ongoing management of GPA can be emotionally challenging. Support from healthcare providers, counselors, or support groups can help manage the psychological impact of living with a chronic illness.
However, the prognosis and quality of life for patients with Granulomatosis with polyangiitis depend on multiple factors, including the severity of the disease, response to treatment, and individual health status. Ongoing care and adjustments in treatment are essential to manage the disease effectively and maintain the best possible quality of life.
FAQs on Granulomatosis with Polyangiitis
What is Granulomatosis with Polyangiitis?
Granulomatosis with polyangiitis (GPA), formerly known as Wegener’s granulomatosis, is a rare autoimmune disorder characterized by inflammation of the blood vessels (vasculitis). This inflammation can restrict blood flow to various organs, leading to damage. Commonly affected areas include the sinuses, lungs, and kidneys.
What are the symptoms of Granulomatosis with Polyangiitis?
Symptoms of GPA can vary significantly but often include sinusitis, fatigue, weight loss, fever, and joint pain. More severe symptoms might involve respiratory issues like coughing, shortness of breath, and in some cases, bleeding in the lungs. Kidney involvement can also occur, potentially leading to kidney failure if untreated.
How is Granulomatosis with Polyangiitis diagnosed?
Diagnosing GPA typically involves a combination of clinical examination, blood tests (especially for ANCA antibodies), imaging tests such as X-rays or CT scans, and a biopsy of affected tissues. These tests help to confirm the presence of vasculitis and rule out other conditions with similar symptoms.
What are the treatment options for Granulomatosis with Polyangiitis?
Treatment for GPA aims to reduce inflammation and manage symptoms. Common treatments include corticosteroids like prednisone to control inflammation and immunosuppressive drugs such as cyclophosphamide or rituximab to limit the immune system’s harmful effects. Treatment plans can vary based on the severity of the disease and the organs involved.
Is Granulomatosis with Polyangiitis curable?
While there is no cure for GPA, it can be managed effectively with medical treatment. Most patients achieve remission with appropriate therapy. Ongoing monitoring and treatment adjustments are crucial to manage flare-ups and minimize organ damage.
How does Granulomatosis with Polyangiitis affect daily life?
Patients with GPA may experience periods of remission and flare-ups. The impact on daily life can vary widely. Some may lead relatively normal lives with treatment, while others might experience significant limitations, depending on which organs are affected and the severity of the symptoms.
Can lifestyle changes help manage Granulomatosis with Polyangiitis?
While lifestyle changes cannot cure GPA, they can help manage the symptoms and improve overall health. Recommended changes might include a balanced diet, regular exercise, avoiding smoking, and getting adequate rest. Additionally, it’s important for patients to closely monitor their health and report any new symptoms to their healthcare provider promptly.
What support is available for people with Granulomatosis with Polyangiitis?
Living with GPA can be challenging, but support is available. Many hospitals offer counseling or support groups for patients with vasculitis. National and international organizations, such as the Vasculitis Foundation, also provide resources, support networks, and information that can help patients navigate their condition.
Conclusion
Recognizing the symptoms of Granulomatosis with Polyangiitis (GPA), seeking timely diagnosis, and adhering to treatment plans are crucial steps in effectively managing this complex condition. Early detection and appropriate medical intervention can significantly improve the prognosis for individuals with GPA, reducing the risk of severe complications and enhancing overall quality of life.
It is equally important to support ongoing research and patient education initiatives. Continued advancements in medical research are essential for developing more effective treatments and potentially finding a cure for GPA. Furthermore, educating patients about their condition empowers them to take an active role in their health management, promoting better treatment outcomes.
We encourage healthcare professionals, researchers, and communities to keep pushing the boundaries of what we know about GPA. Through collective efforts in research and education, we can hope to see a future where this challenging disease is no longer a life-altering diagnosis.
Certainly! Here’s a SEO and readability-friendly “References” section for an article about Granulomatosis with Polyangiitis (GPA) treatment:
References
For those interested in exploring more about Granulomatosis with Polyangiitis and its treatments, below is a list of reputable sources that provide in-depth information and further validation of the treatments discussed:
- American College of Rheumatology (ACR) – Provides comprehensive guidelines and the latest research findings on the treatment of Granulomatosis with Polyangiitis. Visit ACR’s website on GPA
- Mayo Clinic – Offers detailed patient-friendly information about the diagnosis, treatment options, and management of GPA. This resource is helpful for understanding the disease from a clinical perspective. Read more about GPA at Mayo Clinic
- National Organization for Rare Disorders (NORD) – Provides insights into rare diseases, including Granulomatosis with Polyangiitis. NORD’s articles are useful for patients, families, and healthcare providers interested in the specifics of rare diseases. Explore NORD’s resources on GPA
- PubMed Central – A free full-text archive of biomedical and life sciences journal literature at the U.S. National Institutes of Health’s National Library of Medicine (NIH/NLM). It offers access to numerous scientific studies and clinical trials related to GPA. Search for GPA studies on PubMed Central
- The Lancet – One of the world’s leading medical journals, providing rigorous peer-reviewed research and review articles on various aspects of Granulomatosis with Polyangiitis, including treatment advances and clinical trials. Access The Lancet for recent studies on GPA
These sources are invaluable for anyone looking to deepen their understanding of Granulomatosis with Polyangiitis and its current treatment protocols. Whether you are a patient, a healthcare provider, or someone conducting academic research, these references offer credible and detailed insights into the condition.