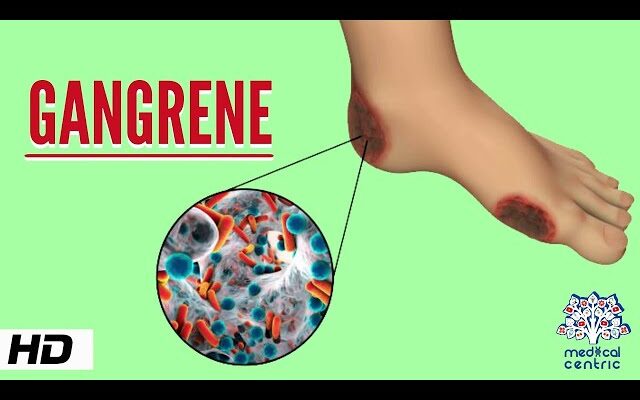
Gangrene Treatment: Gangrene is a serious condition that necessitates swift medical intervention. It occurs when the tissue in part of the body dies due to a lack of blood supply or severe bacterial infection.
Understanding the diagnosis, treatment options, and preventive measures for gangrene is critical for health practitioners and at-risk individuals.
What is Gangrene?
Gangrene is a serious medical condition characterized by the death of body tissue due to a lack of blood supply or a severe bacterial infection. When tissues in the body do not receive enough blood, they lack the oxygen and nutrients needed to survive, leading to tissue death. Gangrene can affect any part of the body but typically affects the extremities like toes, fingers, and limbs. Recognizing gangrene early is crucial because it can lead to serious complications, including the need for amputation or potentially life-threatening infections.
Types of Gangrene
There are several types of gangrene, each with distinct characteristics:
- Dry Gangrene: This type occurs when there is a slow reduction of blood flow to a specific area, usually the toes and feet. It is more common in people with vascular disease, diabetes, and autoimmune diseases. The affected area becomes dry, shriveled, and black as the tissue dies.
- Wet Gangrene: Wet gangrene develops rapidly and is more dangerous than dry gangrene. It often occurs after a severe burn, frostbite, or injury that becomes infected. The affected area becomes swollen, blistered, and emits a foul odor. Immediate treatment is critical to prevent the spread of infection.
- Gas Gangrene: Caused by a bacterial infection from Clostridium bacteria, gas gangrene produces gas within tissue and is extremely life-threatening. It commonly affects deep muscle tissue and can spread quickly. Symptoms include severe pain, swelling, and skin discoloration to a pale or purplish red.
- Internal Gangrene: This form affects internal organs, usually the intestines, gallbladder, or appendix. It occurs when blood flow to an internal organ is blocked, often due to infection or chronic health conditions.
Common Causes and Risk Factors Associated with Gangrene
Gangrene is primarily caused by a lack of blood supply, which can stem from various underlying conditions and external factors. Common causes include:
- Injuries: Physical injuries that cut off blood flow to certain areas, such as those from accidents or severe burns, can lead to gangrene.
- Infections: Certain bacterial infections can directly cause tissue death or create conditions that decrease blood flow.
- Chronic Diseases: Conditions like diabetes and peripheral arterial disease significantly increase the risk of gangrene by impairing circulation.
Risk factors that can contribute to the development of gangrene include:
- Diabetes: High blood sugar levels can damage blood vessels and reduce circulation, making tissues more susceptible to gangrene.
- Smoking: Smoking constricts blood vessels and impairs blood flow, heightening the risk of gangrene.
- Obesity: Excessive body weight can pressure blood vessels and decrease blood circulation to the extremities.
- Immunocompromise: People with weakened immune systems, whether from diseases like HIV or treatments such as chemotherapy, are more vulnerable to infections that can lead to gangrene.
However, understanding the types, causes, and risk factors of gangrene can help in early diagnosis and treatment, thereby preventing severe outcomes such as limb loss or life-threatening infections. Prompt medical attention is essential for anyone exhibiting symptoms or risk factors associated with gangrene.
Symptoms of Gangrene: Recognize the Warning Signs
Early Signs and Symptoms to Watch For
Gangrene is a serious condition that occurs when tissues in the body die due to a loss of blood supply. Recognizing the early signs of gangrene can be crucial for timely medical intervention. Initial symptoms often include:
- Change in Skin Color: The affected area may turn from red to brown and eventually black.
- Swelling or the Formation of Blisters: Early swelling or blistering can occur, filled with clear or bloody fluid.
- Sudden, Severe Pain followed by a Loss of Feeling: Gangrene may start with intense pain, which eventually leads to numbness in the affected area.
- Unpleasant Odor: As the tissue dies, the area might emit a foul smell.
- Skin Coolness: The skin on the affected area may feel cool or cold to the touch due to the reduced blood flow.
Progression of Symptoms in Different Types of Gangrene
Gangrene can manifest in different forms, each with a unique progression of symptoms:
- Dry Gangrene: This type progresses slowly. The skin shrinks and becomes dry and wrinkly, resembling mummified tissue. It usually doesn’t cause pain because it affects nerves.
- Wet Gangrene: More dangerous and rapid than dry gangrene, it typically occurs after a severe burn, frostbite, or injury. The skin may appear swollen and black with blisters or sores that ooze fluid.
- Gas Gangrene: Caused by a bacterial infection, it produces gas in tissue and is characterized by deep pain, fever, air under the skin, and a crackling sensation when the affected area is pressed.
- Internal Gangrene: It affects internal organs, often leading to severe pain and fever. Symptoms depend on the specific organs involved.
When to Seek Medical Attention
It’s imperative to seek immediate medical attention if you or someone else exhibits symptoms of gangrene. Early treatment can prevent the spread of tissue death and save limbs and lives. Key indicators that require urgent care include:
- Persistent and Unexplained Pain: Particularly if an area of the body is discolored and painful.
- Foul-smelling Discharge: Any discharge or oozing from a wound, especially with a bad odor.
- Sudden Loss of Sensation or Movement: If you experience a sudden loss of feeling or are unable to move a part of your body.
Addressing these symptoms promptly by seeking professional medical help can significantly improve outcomes. Remember, gangrene is a medical emergency, and early diagnosis and treatment are critical for preventing serious complications.
Common Diagnostic Techniques for Gangrene
Gangrene, a serious condition characterized by the death of body tissue, demands prompt and accurate diagnosis to prevent further complications. Several diagnostic techniques are commonly employed to identify this condition:
- Physical Examination: Initially, doctors look for physical signs such as swelling, discoloration, and foul-smelling sores. A physical exam is critical as it provides the first clues about the presence and type of gangrene.
- Imaging Tests: Various imaging modalities, including X-rays, MRI scans, and CT scans, play a pivotal role in diagnosing gangrene. These tests help in assessing the extent of tissue damage and detecting gas formation, particularly in cases of gas gangrene.
- Blood Tests: These can detect signs of infection and other complications arising from gangrene. Elevated white blood cell counts, for instance, often indicate the body’s response to infection.
- Tissue Biopsy: In some cases, a tissue biopsy is necessary to confirm a diagnosis of gangrene. By examining a sample of affected tissue under a microscope, healthcare providers can determine the precise cause and type of the tissue death.
- Microbial Cultures: If an infection is suspected, microbial cultures of the tissue or fluid from the affected area can help identify the pathogens involved, guiding appropriate antibiotic treatment.
The Role of Early Diagnosis in Effective Treatment
Early diagnosis of gangrene is crucial for effective treatment. The sooner the condition is identified, the better the chances of limiting damage and preventing severe outcomes, including amputation or life-threatening infections. When gangrene is detected early:
- Treatment Can Begin Immediately: This may involve surgery to remove dead tissue, antibiotics to treat infection, and other interventions to restore blood flow to the affected area.
- Prevents Further Complications: Early intervention prevents the spread of infection and protects healthy tissue from necrosis.
- Improves Recovery Outcomes: Patients diagnosed and treated early for gangrene have significantly better recovery rates and outcomes.
- Reduces Healthcare Costs: By avoiding complications and the need for more extensive treatment, early diagnosis can lead to lower healthcare costs.
However, recognizing the signs and symptoms of gangrene and undergoing the appropriate diagnostic tests are essential steps in managing this serious condition effectively. Healthcare providers and patients must work together to ensure that symptoms are promptly addressed to facilitate early diagnosis and treatment.
Treatment Options for Gangrene
Here are some effective treatment options categorized into surgical treatments, medication strategies, advanced therapies, and the importance of addressing underlying health issues.
Surgical Treatments
Debridement: This procedure involves the removal of dead tissue to prevent the spread of infection to healthy tissue. Debridement is crucial as it helps to reduce the load of infectious agents and creates a better environment for healing.
Amputation: In severe cases, where gangrene has progressed significantly, amputation of the affected limb or part may be necessary. This drastic measure is taken to save the patient’s life by stopping the infection from spreading to other parts of the body.
Revascularization: This surgical technique is used to restore blood flow to the affected areas. Revascularization can be critical for patients with gangrene caused by blocked arteries, helping to prevent tissue death by improving blood supply.
Medication Options
Antibiotics: These are essential in treating and preventing infections that may cause or exacerbate gangrene. Antibiotics are typically administered intravenously to ensure they reach high enough levels in the blood to fight the infection effectively.
Anticoagulants: Used to prevent blood clotting, anticoagulants can help treat types of gangrene that are caused by poor blood circulation. These medications help improve blood flow, which is vital in preventing further tissue death.
Advanced Therapies
Hyperbaric Oxygen Therapy (HBOT): In this treatment, patients breathe pure oxygen in a pressurized room or chamber. HBOT increases the amount of oxygen in the blood, which can help heal the gangrene by stopping the growth of bacteria that thrive in low-oxygen environments and by promoting the growth of new blood vessels.
Bioengineered Tissues and Skin Grafts: These are used to replace or repair damaged or dead tissue. This approach can be particularly beneficial in helping wounds heal and in improving function and appearance after surgical treatments like debridement or amputation.
Importance of Addressing Underlying Conditions
Managing underlying conditions such as diabetes and vascular disease is crucial in treating gangrene. These conditions can significantly impair circulation, leading to chronic wounds and increasing the risk of developing gangrene.
- Diabetes Management: Keeping blood sugar levels under control can help reduce the risk of tissue damage and improve healing processes. Regular monitoring and adherence to diabetic care are essential.
- Vascular Health: Improving vascular health can involve lifestyle changes, medication, or surgeries to remove blockages in blood vessels. Maintaining good vascular health is key to preventing gangrene in individuals at risk of blood flow issues.
Each of these treatment strategies plays a vital role in managing gangrene effectively. It is essential for patients to seek immediate medical attention if gangrene is suspected, as timely intervention can significantly improve outcomes. With a comprehensive approach that includes immediate treatment and management of underlying conditions, most patients can achieve positive results.
Recovery and Management of Gangrene
Recovering from gangrene, a serious condition where body tissue dies, requires careful management and can vary widely in its timeline and approach. This guide provides a comprehensive overview of the recovery process, including physical therapy, symptom management, and long-term health monitoring.
Recovery Process and Timelines
The recovery timeline for gangrene depends significantly on the severity of the condition and the method of treatment employed. For instance, patients who undergo surgical removal of dead tissue may experience a different recovery duration compared to those treated with antibiotics or hyperbaric oxygen therapy. Generally, recovery can range from weeks to several months. Immediate post-surgical recovery typically involves hospitalization where healthcare providers can closely monitor wound healing and prevent further infection. It’s crucial for patients to follow all medical advice and attend all follow-up appointments to ensure the best outcome.
Physical Therapy and Rehabilitation
Physical therapy plays a pivotal role in the rehabilitation process for gangrene patients, especially those who have undergone amputation. A tailored physical therapy program helps to improve strength and mobility, and can aid in adapting to prosthetics if necessary. Rehabilitation focuses on enhancing the quality of life and enabling patients to regain as much independence as possible. Regular sessions with a skilled physical therapist are essential for achieving optimal recovery.
Managing Pain and Other Symptoms Post-Treatment
Pain management is a critical aspect of post-treatment care for gangrene. Patients may experience varying degrees of pain depending on the extent of the condition and the treatment approach. Pain relief strategies might include medications, such as opioids or non-steroidal anti-inflammatory drugs (NSAIDs), and non-pharmacological methods like massage, acupuncture, or relaxation techniques. Additionally, it’s important to address other symptoms such as swelling, fatigue, and emotional distress through comprehensive care.
Long-Term Health Monitoring and Care
Long-term care for gangrene involves regular monitoring to ensure the condition does not recur and to manage any chronic effects of the disease or its treatment. Patients may need ongoing care with vascular specialists to maintain blood flow and prevent future occurrences of tissue death. Lifestyle adjustments, including dietary changes, smoking cessation, and diabetes management, are often recommended to support overall health. Regular check-ups and continuous communication with healthcare providers are vital for maintaining health and preventing further complications.
Overall, the management of gangrene is a multidimensional approach that requires a dedicated medical team and patient adherence to treatment and rehabilitation plans. With the right support, patients can achieve significant recovery and maintain a good quality of life.
Prevention of Gangrene: Essential Strategies
Understanding and implementing these preventive measures is crucial, especially for those at higher risk. This article outlines key strategies to help prevent the onset of gangrene.
Lifestyle Changes to Prevent Gangrene
Making healthy lifestyle choices plays a pivotal role in preventing gangrene. Here are some effective strategies:
- Quit Smoking: Smoking constricts blood vessels and decreases blood flow, significantly increasing the risk of gangrene. Quitting smoking can improve circulation and enhance overall vascular health.
- Healthy Diet: Eating a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help prevent diseases that impair circulation, such as diabetes and atherosclerosis.
- Regular Exercise: Engaging in regular physical activity improves blood flow and is essential in maintaining vascular health, which is key in preventing gangrene.
- Foot Care: For individuals with diabetes or peripheral arterial disease, proper foot care is essential. This includes regular inspection of the feet for injuries or infections, wearing appropriate footwear, and maintaining good hygiene.
Medical Interventions to Ward Off Gangrene
In addition to lifestyle changes, certain medical interventions can significantly reduce the risk of developing gangrene. These include:
- Management of Chronic Conditions: Effective management of conditions like diabetes, atherosclerosis, and peripheral arterial disease is critical. This may involve taking medications as prescribed and regularly monitoring blood sugar levels and blood pressure.
- Use of Blood Thinners: For those at high risk, doctors may prescribe blood thinners to prevent clot formation, which is a common precursor to gangrene.
- Surgical Options: In some cases, surgical intervention may be necessary to improve blood flow. Procedures like angioplasty or vascular bypass surgery can be employed to open blocked arteries and restore normal blood circulation.
Importance of Regular Check-Ups for At-Risk Individuals
Regular medical check-ups are vital for individuals at risk of gangrene. These check-ups can catch early signs of inadequate blood flow and other related complications before they develop into more serious conditions. At-risk individuals should have frequent appointments with their healthcare providers to monitor their health status and make timely adjustments to their treatment plans.
By adopting healthier lifestyle habits and undergoing regular medical monitoring and interventions, individuals can significantly reduce their risk of developing this serious condition. Regular consultations with healthcare providers ensure that any potential issues are addressed early, maintaining overall vascular health and preventing gangrene.
Case Studies and Real-Life Examples of Gangrene Treatment
Gangrene, a serious condition that results in the death of body tissue, often requires prompt medical intervention to prevent widespread effects and potentially save lives. Through a collection of brief case studies, we explore the effectiveness of various treatment methods and uncover valuable insights from real-life instances. Each case study sheds light on different aspects of managing gangrene, emphasizing the importance of timely medical care and tailored treatment strategies.
Case Study 1: Early Detection and Surgical Intervention
John, a 65-year-old diabetic patient, noticed a persistent, painful swelling in his foot. Upon visiting his healthcare provider, he was diagnosed with wet gangrene, a type associated with infection. Immediate action was taken to manage his condition, starting with antibiotics to tackle the infection and followed by surgical removal of the dead tissue. Post-surgery, John underwent several sessions of hyperbaric oxygen therapy, which helped promote healing and saved his foot from amputation. This case highlights the critical role of early detection and the effectiveness of combining surgical and non-surgical treatments.
Case Study 2: Non-Surgical Management and Lifestyle Adjustments
Sarah, a 52-year-old with peripheral arterial disease, developed dry gangrene on her toes. Due to her condition, surgeons opted against amputation and instead focused on enhancing blood circulation through medication and lifestyle changes, including smoking cessation and a healthier diet. Regular monitoring and careful management helped Sarah avoid surgery, illustrating that non-surgical approaches and lifestyle adjustments can be a viable option for managing certain types of gangrene.
Case Study 3: The Impact of Delayed Treatment
Michael, a 70-year-old man, initially ignored signs of discoloration and numbness in his leg. By the time he sought medical help, the gangrene had progressed significantly, necessitating the amputation of his lower leg to prevent further spread of the infection. Michael’s case serves as a sobering reminder of the dangers of delaying treatment for gangrene. It underscores the need for awareness and education on the early signs and symptoms of the condition.
Lessons Learned and Insights Gained
These cases collectively emphasize several critical insights:
- Early Detection and Prompt Treatment: The importance of recognizing early symptoms and seeking immediate care cannot be overstressed. Early intervention significantly improves outcomes.
- Individualized Treatment Approaches: Treatment should be tailored to the patient’s specific type of gangrene and overall health status, as seen in the differences between surgical and non-surgical management strategies.
- Education and Awareness: Increasing awareness about the signs and risks associated with gangrene can lead to earlier diagnosis and treatment, potentially saving limbs and lives.
- Holistic Management: Addressing underlying conditions and lifestyle factors is crucial for effective management and prevention of recurrence.
These real-life examples serve not only as educational materials but also as poignant reminders of the challenges and triumphs faced in the treatment of gangrene. They highlight the nuanced approaches required to manage such a complex medical condition effectively.
FAQs on Gangrene Treatment
What are the common treatments for gangrene?
The primary treatments for gangrene involve removing the dead tissue, preventing infection, and restoring blood flow to the affected area. This may include surgical removal of the dead tissue (debridement), antibiotics to fight infection, and procedures to improve blood flow, such as bypass surgery or angioplasty. In severe cases, amputation of the affected limb may be necessary.
Can gangrene be treated without surgery?
Non-surgical treatments for gangrene are limited but may include hyperbaric oxygen therapy, where patients breathe pure oxygen in a pressurized room to help heal the tissue. Antibiotics are also used to control and prevent infections. However, surgical intervention is often necessary to remove dead tissue and prevent the spread of the condition.
How long does it take to recover from gangrene?
Recovery time from gangrene depends on the severity of the condition and the type of treatment administered. Surgical treatments may require weeks to months of healing time, with additional rehabilitation needed if there has been significant tissue loss or amputation. Non-surgical treatments like hyperbaric oxygen therapy might require multiple sessions over several weeks.
Is gangrene contagious?
Gangrene itself is not contagious and cannot be transmitted from person to person. However, the bacterial infections that often cause gangrene can spread, particularly in hospital environments. Proper hygiene and wound care are essential to prevent the spread of infection.
What can I do to prevent gangrene from worsening?
If you suspect gangrene, seek medical attention immediately. Early treatment is crucial. Keep the affected area clean and dry, follow your healthcare provider’s instructions, and manage any underlying conditions, such as diabetes or peripheral artery disease, that can contribute to poor blood circulation.
Conclusion
In conclusion, understanding the critical importance of early diagnosis and comprehensive treatment for gangrene cannot be overstated. Detecting gangrene at its earliest stages significantly enhances the effectiveness of the treatment, potentially saving limbs and lives. Comprehensive care, which may include antibiotics, surgery, and hyperbaric oxygen therapy, is crucial for halting the progression of the disease and ensuring the best possible outcomes.
If you suspect that you or someone you know may be showing signs of gangrene, such as persistent pain, skin discoloration, or foul-smelling wounds, it is imperative to seek medical attention immediately. Prompt action not only increases the likelihood of a full recovery but also minimizes the risk of complications. Remember, your health and well-being are paramount, and timely medical intervention is key in the fight against gangrene.
References
For those seeking additional information or wishing to verify the data presented in our discussion on gangrene treatment, we recommend consulting the following reputable sources. These resources are renowned for their credibility and depth of information in the field of medical treatment and research:
- Centers for Disease Control and Prevention (CDC) – The CDC provides comprehensive guidelines and latest research findings on the prevention and treatment of gangrene. Access their resources at CDC’s Official Website.
- Mayo Clinic – Known for its patient-centric approach, the Mayo Clinic offers detailed articles on the symptoms, causes, and treatments for gangrene. Visit their dedicated gangrene section here.
- MedlinePlus – A service of the U.S. National Library of Medicine, MedlinePlus offers trusted information on numerous health conditions, including gangrene. Their resource page can be found at MedlinePlus.
- World Health Organization (WHO) – WHO provides global insights and data on various health emergencies, including infections leading to gangrene. Their publications can be accessed via WHO’s official portal.
- PubMed – A search engine comprising biomedical literature from MEDLINE, life science journals, and online books. PubMed articles can provide more scientific insight into the latest treatments for gangrene. Search relevant articles at PubMed.
Each of these resources offers peer-reviewed articles, treatment guidelines, and the latest research that can help readers understand the complexities of gangrene treatment and prevention.
By referring to these established sources, you can ensure that the information you rely on is accurate and up-to-date.