Functional Dyspepsia Symptoms: Functional dyspepsia, often referred to as non-ulcer dyspepsia or indigestion, is a common gastrointestinal disorder characterized by chronic or recurrent pain and discomfort in the upper abdomen.
This condition significantly impacts the quality of life and can lead to considerable health care expenses. Understanding its symptoms and causes is crucial for effective management and treatment.
What is Functional Dyspepsia?
Functional Dyspepsia (FD) is a common digestive disorder characterized by chronic discomfort or pain in the upper abdomen without an identifiable cause. Symptoms may include bloating, nausea, early satiety, and burning sensations in the stomach area. Unlike other gastrointestinal conditions, FD does not alter the physical structure of the digestive system, making it a functional disorder.
Epidemiology: How Common is Functional Dyspepsia?
Functional dyspepsia is widespread, affecting about 10% to 30% of the population globally. The prevalence can vary significantly based on geographical regions and diagnostic criteria. Despite its high occurrence, FD often remains underdiagnosed because its symptoms overlap with other digestive disorders.
Distinction Between Functional Dyspepsia and Other Digestive Disorders
Functional dyspepsia is distinct from other gastrointestinal conditions like gastroesophageal reflux disease (GERD) and peptic ulcers, primarily because it lacks structural abnormalities in the digestive tract. GERD, for instance, is associated with acid reflux affecting the esophagus, whereas peptic ulcers involve clear erosions in the stomach lining. Distinguishing FD from these conditions is crucial, as it influences treatment strategies. Effective diagnosis typically involves excluding these other conditions through medical tests, reinforcing the functional nature of FD.
By understanding these distinctions and epidemiological factors, patients and healthcare providers can better approach the management of functional dyspepsia, enhancing quality of life for those affected.
Symptoms of Functional Dyspepsia
Understanding the symptoms can help in managing this condition effectively. Here, we’ll explore the common and less frequent symptoms of functional dyspepsia and discuss how they might impact daily life.
Common Symptoms of Functional Dyspepsia
Functional dyspepsia is characterized by a cluster of symptoms that typically arise in the upper abdomen. The most prevalent symptoms include:
- Persistent or Recurrent Pain: Many individuals experience a gnawing or burning sensation centered in the middle part of the upper abdomen.
- Bloating: A feeling of fullness or swelling in the abdomen, often after eating, is commonly reported.
- Early Satiety: This is when you feel unusually full after a small meal, which prevents you from finishing meals.
- Nausea: While not always present, many people with functional dyspepsia report feeling nauseous, especially after eating.
- Belching and Regurgitation: These symptoms can occur as the body tries to relieve discomfort from gas or other stomach contents.
Less Common Symptoms
In addition to the more frequent symptoms, there are several less common signs that can still be indicative of functional dyspepsia:
- Vomiting: While not as common, some individuals may experience vomiting as part of their symptoms.
- Heartburn and Acid Reflux: Although these are more typical of gastroesophageal reflux disease (GERD), they can also occur in people with functional dyspepsia.
- Weight Loss: In rare cases, ongoing discomfort and early satiety can lead to unintentional weight loss.
Impact on Daily Life
The symptoms of functional dyspepsia can significantly interfere with daily activities and overall quality of life. The discomfort and pain can affect concentration, reduce productivity at work, and limit social interactions, especially those involving meals. The unpredictability of symptoms can also lead to stress and anxiety, as individuals worry about when and where symptoms may occur.
Overall, managing the symptoms of functional dyspepsia involves understanding the triggers and conditions under which symptoms worsen. Lifestyle changes, dietary adjustments, and, in some cases, medications can help alleviate the discomfort associated with this condition, thereby improving life quality.
By recognizing both the common and uncommon symptoms of functional dyspepsia and understanding their potential impact on daily life, individuals can seek appropriate treatment and make necessary adjustments to manage their condition effectively.
Causes of Functional Dyspepsia
Understanding its causes and the mechanisms behind its symptoms is crucial for effective management. This article delves into the known causes, discusses how these lead to typical symptoms, and highlights current research and theories within the medical community.
Known Causes of Functional Dyspepsia
The exact causes of functional dyspepsia are not fully understood, but several factors are commonly associated with its development:
- Gut-Brain Axis Disruption: This refers to the communication pathway between the gut and the brain, which can affect gut function and pain perception.
- Delayed Gastric Emptying: Some individuals with functional dyspepsia have slower than normal emptying of the stomach. This can cause bloating, nausea, and discomfort after eating.
- Helicobacter pylori Infection: While Helicobacter pylori does not cause functional dyspepsia in every individual, it is more commonly found in those diagnosed with this condition and could contribute to some symptoms.
- Genetic Factors: There may be genetic predispositions that affect how the body processes certain foods and signals pain.
- Dietary Habits: Consuming large meals or specific foods that irritate the stomach can trigger symptoms in susceptible individuals.
- Psychosocial Factors: Stress and anxiety are significant contributors to the manifestation of symptoms, potentially exacerbating the gut-brain axis disruption.
Impact of These Causes on Symptoms
The aforementioned factors contribute to the typical symptoms of functional dyspepsia, which include upper abdominal pain, bloating, and feeling quickly full after starting to eat. The disruption of the gut-brain axis, for instance, may enhance the perception of pain and discomfort, even when other physical signs are minimal. Delayed gastric emptying causes prolonged stomach fullness, leading to discomfort and bloating.
Current Research and Theories
Research into functional dyspepsia is ongoing and focuses on several areas:
- Microbiome Studies: Researchers are examining how the gut microbiota (the complex community of microorganisms in the digestive system) affects functional dyspepsia. Changes in gut bacteria may influence symptoms and could open new treatment avenues.
- Neurological Research: There is increasing interest in how the nerves in the stomach behave and their role in pain and motility disorders.
- Diet and Lifestyle: Studies are exploring how dietary modifications and stress reduction techniques can relieve symptoms, suggesting that lifestyle plays a pivotal role in managing functional dyspepsia.
Theories continue to evolve, but there is a consensus that a multifactorial approach is necessary to understand and treat functional dyspepsia effectively. As research progresses, it is hoped that better diagnostic tools and treatments will become available, improving quality of life for those affected by this challenging condition.
Diagnosing Functional Dyspepsia
Understanding the criteria for diagnosing this condition, the common tests involved, and the challenges faced during diagnosis can help patients and healthcare providers manage the condition more effectively.
Criteria for Diagnosing Functional Dyspepsia
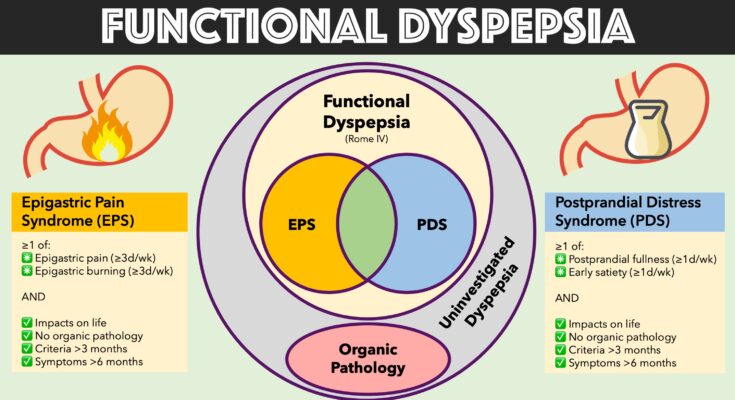
The diagnosis of functional dyspepsia typically begins with meeting the Rome IV criteria, which are internationally recognized guidelines used to identify gastrointestinal disorders. According to these criteria, patients must experience one or more of the following symptoms for at least three months, with symptom onset at least six months prior to diagnosis:
- Bothersome postprandial fullness (feeling excessively full after meals)
- Early satiation (feeling full after eating only a small amount of food)
- Epigastric pain (pain or discomfort in the upper abdomen)
- Epigastric burning (a burning sensation in the upper abdomen)
These symptoms should not be explained by another medical condition, based on thorough evaluation. Moreover, functional dyspepsia is categorized into two types: postprandial distress syndrome (PDS), which primarily involves meal-induced symptoms, and epigastric pain syndrome (EPS), which does not depend on food intake.
Common Diagnostic Tests and Procedures
To rule out other causes of the symptoms and confirm a diagnosis of functional dyspepsia, healthcare providers may recommend several tests:
- Upper Gastrointestinal Endoscopy: This is commonly performed to visually examine the stomach and duodenum for abnormalities. It is especially recommended for patients over 60 or those displaying “alarm features” like significant weight loss, persistent vomiting, or gastrointestinal bleeding.
- Helicobacter pylori Testing: Testing for H. pylori infection, a common cause of ulcers, is crucial as its eradication can improve symptoms.
- Blood Tests: Basic blood tests can help exclude anemia, liver problems, pancreatic diseases, and other conditions.
- Breath Tests: These are used to check for lactose intolerance and bacterial overgrowth which can mimic or exacerbate symptoms of dyspepsia.
These procedures help in providing a clear picture and ensuring that the symptoms are not due to other diseases like peptic ulcers or gastric cancer.
Challenges in Diagnosing Functional Dyspepsia
Diagnosing functional dyspepsia presents several challenges:
- Symptom Overlap: The symptoms of functional dyspepsia overlap significantly with those of other gastrointestinal disorders such as gastroesophageal reflux disease (GERD) and irritable bowel syndrome (IBS), making it difficult to pinpoint dyspepsia without extensive testing.
- Lack of Biomarkers: There are no specific biomarkers to definitively diagnose functional dyspepsia, which means diagnosis largely relies on symptom description and the exclusion of other diseases.
- Variability of Symptoms: Symptoms can vary widely in frequency and intensity, often influenced by factors like diet, stress, and lifestyle, complicating the diagnostic process.
By understanding these criteria, tests, and challenges, healthcare providers can approach the diagnosis of functional dyspepsia with a structured plan, improving the likelihood of an accurate diagnosis and effective management plan.
Treatment Options for Functional Dyspepsia
Managing this condition effectively involves a combination of medical interventions and lifestyle adjustments. Below, we explore the current treatment strategies, medications commonly used to alleviate symptoms, and lifestyle changes and home remedies that help manage symptoms.
Current Treatment Strategies for Functional Dyspepsia
Treating functional dyspepsia typically involves a personalized approach, as symptoms and their severity can vary widely among patients. The primary goals are to alleviate symptoms, improve quality of life, and prevent recurrence. Treatment strategies include:
- Medical Evaluation: A thorough medical evaluation is crucial to rule out other possible conditions and tailor the treatment plan to the individual’s specific symptoms.
- Medication Management: Depending on the symptoms, different medications may be prescribed to reduce discomfort and improve digestive function.
- Lifestyle and Dietary Adjustments: Modifications in daily habits and diet can significantly impact symptom management and overall digestive health.
- Psychological Therapies: Since stress and anxiety can exacerbate dyspepsia, therapies such as cognitive-behavioral therapy (CBT) are sometimes recommended.
Medications Commonly Used to Alleviate Symptoms
Several medications are available to help manage the symptoms of functional dyspepsia. These include:
- Antacids and Acid Blockers: Over-the-counter antacids can neutralize stomach acid and provide quick relief. H2-receptor antagonists and proton pump inhibitors help reduce acid production.
- Prokinetics: These drugs help increase the movement of the stomach and intestines, aiding in faster digestion and reducing symptoms.
- Antidepressants: Low doses of certain antidepressants can help modulate pain perception in the gastrointestinal tract.
- Antispasmodics: These medications can help reduce stomach muscle spasms and are often used for pain relief in functional dyspepsia.
Lifestyle Changes and Home Remedies That Help Manage Symptoms
In addition to medication, making lifestyle changes can play a crucial role in managing functional dyspepsia. Effective home remedies and adjustments include:
- Dietary Changes: Avoid foods that trigger symptoms, such as fatty and spicy foods, and eat smaller, more frequent meals.
- Increase Physical Activity: Regular exercise helps improve overall digestive function and reduce stress.
- Stress Management Techniques: Techniques such as yoga, meditation, and deep breathing can reduce stress and improve symptoms.
- Adequate Rest: Ensuring sufficient sleep each night helps the body manage stress and heal.
Implementing these treatment options can significantly improve the quality of life for those suffering from functional dyspepsia. It’s important for individuals to consult healthcare providers to create a tailored treatment plan that addresses their specific symptoms and lifestyle.
Managing Life with Functional Dyspepsia
Living with functional dyspepsia can be challenging, but with the right strategies, you can manage the symptoms and lead a comfortable life. This section provides practical tips for coping with dyspepsia in daily activities, dietary recommendations, and guidance on when to seek further medical advice.
Tips for Coping with Symptoms in Daily Activities
Functional dyspepsia often involves persistent upper abdominal discomfort, but integrating a few management strategies into your daily routine can help minimize these disruptions:
- Eat Smaller, More Frequent Meals: Consuming smaller meals more frequently can prevent the stomach from becoming overly full, reducing discomfort.
- Avoid Trigger Foods: Identify foods that exacerbate your symptoms and try to avoid them. Common triggers include spicy foods, caffeine, and fatty foods.
- Stay Upright After Eating: Remaining upright for at least 30 minutes after eating can help reduce reflux symptoms, which can exacerbate dyspepsia.
- Manage Stress: Since stress can worsen dyspepsia symptoms, consider stress-reduction techniques such as meditation, deep breathing exercises, or gentle yoga.
Dietary Recommendations
What you eat plays a crucial role in managing functional dyspepsia. Here are some dietary guidelines to help alleviate your symptoms:
- Fiber-Rich Foods: Incorporate a good amount of fiber into your diet as it helps with the overall digestive process. Foods like whole grains, fruits, and vegetables are great options.
- Limit Fat Intake: High-fat foods can slow down the stomach’s emptying process and exacerbate symptoms. Opt for lean meats, low-fat dairy products, and cooking methods that require less fat.
- Hydration: Keep well-hydrated, but be mindful of when and how much you drink. Sometimes drinking large amounts with meals can cause bloating and discomfort.
- Consider Food Preparation: How you prepare food can also impact symptoms. Grilled, baked, or steamed dishes are typically easier on the stomach than fried foods.
When to Seek Further Medical Advice
It’s important to consult with a healthcare provider if you experience any of the following situations:
- Symptoms Persist or Worsen: If dietary adjustments and lifestyle changes do not improve your symptoms, or if symptoms worsen, seek medical advice.
- Troublesome Symptoms: Symptoms such as unintentional weight loss, vomiting, or severe pain should be evaluated by a doctor promptly.
- Symptom Identification: Sometimes symptoms that seem to be dyspepsia could be signs of a more serious condition. A healthcare provider can help differentiate between functional dyspepsia and other possible diagnoses.
By understanding and implementing these strategies, you can reduce discomfort and improve your quality of life. Remember, a proactive approach to managing symptoms can make a significant difference.
FAQs on Functional Dyspepsia Symptoms
What is functional dyspepsia?
Functional dyspepsia, also known as indigestion with no clear cause, affects the stomach and gastrointestinal tract. It leads to chronic discomfort or pain in the upper abdomen, but is not linked to any observable structural abnormalities.
What are the common symptoms of functional dyspepsia?
The most common symptoms include persistent or recurring pain in the upper abdomen, a feeling of uncomfortable fullness after a meal, early satiety (feeling full after eating only a small amount of food), bloating, and nausea. Some people may also experience belching, vomiting, or acid reflux.
How do I distinguish functional dyspepsia from other digestive disorders?
Functional dyspepsia is diagnosed primarily through its symptoms and by ruling out other gastrointestinal disorders. Unlike other conditions like gastric ulcers or gastroesophageal reflux disease (GERD), functional dyspepsia does not show any structural damage to the gastrointestinal tract. A healthcare provider may perform tests to rule out other conditions before diagnosing functional dyspepsia.
Can stress exacerbate functional dyspepsia symptoms?
Yes, stress can exacerbate the symptoms of functional dyspepsia. Stress and anxiety can affect the digestive system, worsening symptoms such as pain and fullness. Managing stress through relaxation techniques, regular exercise, and adequate sleep may help alleviate symptoms.
Is there a treatment for functional dyspepsia?
While there is no cure for functional dyspepsia, symptoms can often be managed with dietary adjustments, medications, and lifestyle changes. Eating smaller, more frequent meals, avoiding trigger foods, and reducing alcohol and caffeine intake can help manage symptoms. Medications such as antacids, proton pump inhibitors, or prokinetics may also be prescribed based on individual symptoms.
When should I see a doctor for functional dyspepsia symptoms?
You should consult a healthcare provider if symptoms persist, worsen, or significantly impact your quality of life. It is also important to seek medical advice if you experience symptoms like unintended weight loss, severe pain, or vomiting blood, as these may indicate a more serious condition.
Conclusion:
Understanding the nuances of functional dyspepsia is essential for managing its symptoms effectively. By identifying common indicators such as persistent upper abdominal discomfort, bloating, and nausea, individuals can take proactive steps towards seeking medical advice. Recognizing these symptoms early is crucial as they often mirror those of more serious conditions.
Functional dyspepsia, while non-life-threatening, can significantly impact quality of life. Its causes are varied, ranging from diet and lifestyle factors to stress and gastric motility issues. Knowledge of these causes aids in personalized treatment approaches which might include dietary changes, medications, or stress management techniques.
We strongly encourage anyone experiencing symptoms indicative of functional dyspepsia to consult with healthcare providers. A professional diagnosis is vital to rule out other potential conditions and to formulate an effective treatment plan tailored to individual needs. Remember, addressing symptoms promptly with the help of a healthcare professional not only improves your health but also enhances your overall well-being.
References
For those seeking to delve deeper into the understanding of Functional Dyspepsia symptoms, here are some reputable sources that offer extensive research and insights. These references are valuable for both patients looking for information and healthcare professionals needing the latest studies and treatment modalities.
- Mayo Clinic – Functional Dyspepsia Overview
Explore a comprehensive overview of Functional Dyspepsia provided by the Mayo Clinic, a leading authority in medical education and research. This resource includes symptoms, causes, and treatment options available for managing this condition.
Read more at Mayo Clinic - National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
The NIDDK provides in-depth information on Functional Dyspepsia, including dietary recommendations and potential triggers that exacerbate symptoms. This is an essential resource for understanding the digestive disorder from a scientific and practical perspective.
Learn more on NIDDK - PubMed Central
For those interested in the latest research, PubMed Central offers a range of peer-reviewed articles on Functional Dyspepsia. This site is invaluable for accessing free full-text articles that discuss recent advances in diagnosis and treatment.
Explore studies on PubMed - International Foundation for Gastrointestinal Disorders
This site offers resources specifically tailored to patients experiencing gastrointestinal disorders, including Functional Dyspepsia. It provides patient stories, management tips, and a community forum for support and sharing personal experiences.
Visit the IFFGD - Cleveland Clinic – Digestive Diseases
The Cleveland Clinic is another trusted source for information on a variety of digestive disorders, including Functional Dyspepsia. Their resources include treatment advances, lifestyle modification tips, and preventative measures to control symptoms.
Read more at Cleveland Clinic
These resources will provide both foundational knowledge and advanced insights into Functional Dyspepsia, supporting better understanding and management of the condition.