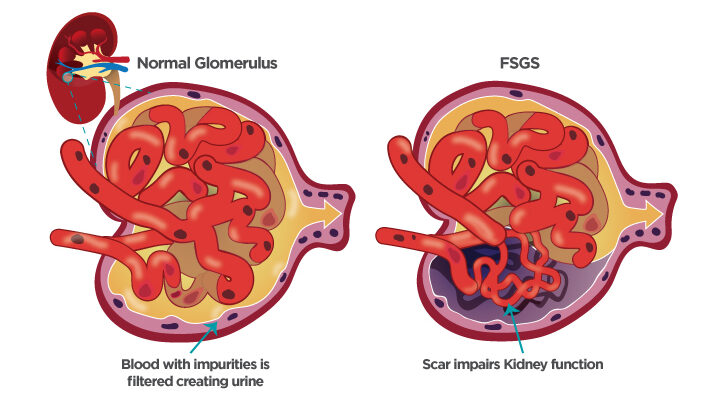
Focal Segmental Glomerulosclerosis Treatment: Focal Segmental Glomerulosclerosis (FSGS) is a complex kidney disorder marked by scarring in the kidney’s filtering units, known as glomeruli.
This condition can lead to significant kidney damage and, ultimately, kidney failure if not diagnosed and treated effectively.
Our comprehensive guide delves into the critical aspects of FSGS, including its diagnosis, treatment options, and management strategies, to provide patients and healthcare providers with the necessary tools to combat this challenging condition.
Understanding Focal Segmental Glomerulosclerosis (FSGS)
Focal Segmental Glomerulosclerosis (FSGS) is a complex kidney disorder characterized by scarring (sclerosis) in the kidney’s filtering units, known as glomeruli. The disease can lead to significant kidney damage and, ultimately, kidney failure if left untreated. This guide offers an in-depth look at FSGS, including its types, causes, prevalence, symptoms, and risk factors.
Types of Focal Segmental Glomerulosclerosis (FSGS)
FSGS is categorized into several types, each with distinct characteristics:
- Primary FSGS: Occurs without a known cause, possibly due to the body’s immune response affecting the kidneys.
- Secondary FSGS: Results from other diseases or factors such as obesity, drug use, and infections that damage the kidneys.
- Genetic FSGS: Caused by genetic mutations affecting kidney function.
- Adaptive FSGS: Develops in response to changes or damage in the kidneys, often due to other underlying conditions.
Focal Segmental Glomerulosclerosis (FSGS) Causes
The exact cause of primary FSGS remains unknown, though it’s believed to involve the body’s immune system attacking the kidneys. Secondary FSGS can be traced to a variety of factors, including:
- Obesity
- Certain infections
- Drug use
- Genetic mutations
- Diseases that affect the kidneys
Statistics on Prevalence and Demographics Affected
FSGS is a rare condition, accounting for a significant portion of cases among individuals diagnosed with nephrotic syndrome, a collection of symptoms indicating kidney damage. It affects both children and adults, with a higher incidence reported in certain demographic groups, including African Americans. The prevalence of FSGS has been increasing globally, reflecting both better diagnostic techniques and rising risk factors such as obesity.
Key Symptoms and Risk Factors Associated with FSGS
Symptoms of FSGS can include:
- Swelling in parts of the body, especially the legs and feet, due to fluid retention
- Fatigue
- Foamy urine, indicating excess protein (proteinuria)
- Poor appetite
- Weight gain
Risk factors for developing FSGS include:
- Family history of the disease
- Obesity
- Certain racial backgrounds, with higher rates in African Americans
- Use of specific drugs, including some used to treat other medical conditions
- Previous kidney diseases or infections
If you suspect you have symptoms of FSGS, consulting a healthcare professional for proper diagnosis and treatment is essential. Early intervention can significantly improve the prognosis for individuals with FSGS, highlighting the importance of awareness and education on this condition.
Diagnosis of Focal Segmental Glomerulosclerosis (FSGS)
Diagnosing FSGS accurately is crucial for the management and treatment of the condition. This article outlines the diagnostic criteria and methods for FSGS, discusses the challenges in diagnosing the disease, and highlights the importance of differential diagnosis.
Diagnostic Criteria and Methods for FSGS
To diagnose FSGS, healthcare professionals rely on a combination of clinical evaluation, laboratory testing, and kidney biopsy. Here’s a detailed look at the diagnostic criteria and methods:
- Clinical Evaluation: Initial assessment includes a patient’s medical history, symptoms, and a physical examination. Key indicators include proteinuria (high levels of protein in the urine), edema (swelling), and hypertension.
- Laboratory Testing: Blood and urine tests are essential for evaluating kidney function and the severity of proteinuria. These tests help in assessing the levels of creatinine, urea, and proteins in the body.
- Kidney Biopsy: A kidney biopsy is the gold standard for diagnosing FSGS. It involves taking a small sample of kidney tissue for microscopic examination. This procedure helps in identifying the characteristic scarring and segmental glomeruli involvement.
- Imaging Studies: While not diagnostic for FSGS specifically, imaging studies such as ultrasound or CT scans can be useful for ruling out other kidney conditions.
Challenges in Diagnosing FSGS and Solutions
Diagnosing FSGS presents several challenges, primarily due to its nonspecific symptoms and the overlap with other kidney diseases. Here’s how these challenges are addressed:
- Variability of Symptoms: FSGS can present with a range of symptoms that are not unique to the disease. A comprehensive approach combining patient history, physical examination, and laboratory findings helps in narrowing down the diagnosis.
- Kidney Biopsy Limitations: Sometimes, the biopsy may not sample the affected glomeruli due to the focal nature of the disease. Repeated biopsies or more extensive sampling may be necessary in some cases.
- Interpretation of Biopsy Results: The interpretation of biopsy findings can be complex. It often requires experienced nephropathologists to differentiate FSGS from other glomerular diseases.
Importance of Differential Diagnosis
Differential diagnosis plays a pivotal role in distinguishing FSGS from other kidney diseases, such as minimal change disease (MCD), membranous nephropathy, and IgA nephropathy. This process is crucial because the treatment and prognosis for these conditions can vary significantly. Factors considered in differential diagnosis include the pattern of proteinuria, response to steroids, and specific findings on kidney biopsy.
However, the diagnosis of FSGS involves a multifaceted approach that includes clinical evaluation, laboratory testing, kidney biopsy, and the critical role of differential diagnosis. Addressing the challenges in diagnosing FSGS is key to ensuring accurate diagnosis and optimal management of the disease. Understanding the diagnostic process helps patients and healthcare providers navigate the complexities of FSGS and contributes to better outcomes.
Treatment Options for Focal Segmental Glomerulosclerosis (FSGS)
Managing FSGS effectively requires a comprehensive approach, including medications, diet, lifestyle adjustments, and emerging therapies. Here, we delve into the variety of treatment options available for FSGS, emphasizing the significance of personalized treatment plans.
Medications:
Corticosteroids: Often the first line of defense, corticosteroids help reduce inflammation and immune response, potentially slowing the disease’s progression. Their effectiveness varies among individuals, and long-term use may lead to side effects, underscoring the need for careful monitoring.
Immunosuppressive Drugs: For patients who don’t respond well to corticosteroids, or in more aggressive cases, immunosuppressive medications may be prescribed. These drugs aim to suppress the immune system’s activity to prevent further damage to the kidneys.
Other Medications: Depending on individual symptoms and the disease’s progression, additional medications may include blood pressure drugs, cholesterol-lowering medications, and treatments to address proteinuria (excessive protein in urine), all contributing to a holistic management approach.
Role of Diet and Lifestyle Changes in Managing FSGS:
Diet and lifestyle modifications play a crucial role in managing FSGS. A balanced diet, low in sodium and saturated fats, can help control blood pressure, reduce cholesterol levels, and manage body weight, all of which are vital for patients with FSGS. Regular exercise, smoking cessation, and limiting alcohol intake are also beneficial in creating a healthier lifestyle that supports kidney health.
Cutting-edge Treatments and Therapies:
The landscape of FSGS treatment is evolving with the introduction of new therapies and technologies. Research into novel treatments such as monoclonal antibodies, which target specific pathways involved in the disease process, offers hope for more effective and targeted interventions.
Gene Therapy and Personalized Medicine Prospects in FSGS Treatment:
The future of FSGS treatment is bright with the promise of gene therapy and personalized medicine. Advances in genetic testing and understanding of the disease’s molecular basis are paving the way for treatments tailored to individual genetic profiles. These approaches aim to not only treat FSGS more effectively but also minimize side effects by targeting therapy to each patient’s specific condition.
However, managing FSGS requires a multifaceted approach, incorporating traditional medications, lifestyle changes, and cutting-edge therapies. With ongoing research and advances in personalized medicine, patients with FSGS have a hopeful outlook towards more effective and individualized treatment options.
Navigating Complications and Managing Focal Segmental Glomerulosclerosis (FSGS)
Understanding the common complications associated with FSGS and employing effective strategies for their management, monitoring, and care is essential for patients and healthcare providers alike. This article aims to provide a comprehensive guide to navigating these complexities, with a focus on preventing disease progression and enhancing the quality of life for individuals with FSGS.
Common Complications Associated with FSGS and Their Management
FSGS can lead to several complications, primarily due to its impact on kidney function. Key complications include:
- Proteinuria: Excessive protein loss in urine, a hallmark of FSGS, can lead to swelling in the legs and abdomen. Management includes the use of medications such as angiotensin-converting enzyme (ACE) inhibitors or angiotensin II receptor blockers (ARBs) to reduce proteinuria and control blood pressure.
- Chronic Kidney Disease (CKD): FSGS can progress to CKD, necessitating close monitoring of kidney function through regular blood tests, and managing underlying conditions that can worsen kidney health.
- Nephrotic Syndrome: This is characterized by high levels of protein in the urine, low levels of protein in the blood, high cholesterol, and swelling. Treatment focuses on controlling symptoms and may include diuretics, blood pressure medications, and steroids.
Monitoring and Ongoing Care for Individuals with FSGS
Ongoing care for patients with FSGS involves regular monitoring to assess the progression of the disease and the effectiveness of treatment strategies. Essential aspects of care include:
- Regular Blood and Urine Tests: These tests help track kidney function and the level of proteinuria.
- Blood Pressure Management: Maintaining optimal blood pressure is crucial in slowing down the progression of kidney damage.
- Dietary Adjustments: A diet low in sodium and saturated fats can help manage blood pressure and cholesterol levels, reducing the risk of further kidney damage.
Strategies for Preventing Disease Progression and Managing Quality of Life
Preventing the progression of FSGS and managing the quality of life requires a multifaceted approach, including:
- Healthy Lifestyle Choices: Regular physical activity, a balanced diet, and avoiding smoking can significantly impact the overall health and well-being of individuals with FSGS.
- Medication Adherence: Following the prescribed medication regimen is vital in managing symptoms and slowing disease progression.
- Mental Health Support: The chronic nature of FSGS can take a toll on mental health. Access to support groups, counseling, and stress management techniques can be beneficial.
By understanding common complications and employing strategies for monitoring, ongoing care, and lifestyle management, individuals with FSGS can lead healthier lives. It’s essential for patients and healthcare providers to work closely together to tailor care plans that address the unique needs of each individual, aiming to prevent disease progression and enhance quality of life.
FAQs on Focal Segmental Glomerulosclerosis Treatment
What is Focal Segmental Glomerulosclerosis (FSGS)?
Focal Segmental Glomerulosclerosis (FSGS) is a disease in which scar tissue develops on the parts of the kidneys that filter waste from the blood (glomeruli). FSGS can cause nephrotic syndrome and lead to chronic kidney disease and failure over time.
How is FSGS treated?
The treatment of FSGS focuses on slowing down the progression of the disease to preserve kidney function. Common treatments include:
- Corticosteroids and Immunosuppressive Drugs: To reduce proteinuria (protein in the urine) and improve kidney function.
- Angiotensin-Converting Enzyme (ACE) Inhibitors and Angiotensin II Receptor Blockers (ARBs): To lower blood pressure and reduce proteinuria.
- Plasmapheresis: In some cases, to remove harmful substances from the blood.
Is there a cure for FSGS?
Currently, there is no cure for FSGS. However, treatments can be effective in managing symptoms and slowing the progression of the disease. The choice of treatment depends on various factors, including the cause of FSGS, symptoms, and how quickly the disease is progressing.
Can diet and lifestyle changes help with FSGS treatment?
Yes, diet and lifestyle changes can support treatment outcomes and improve overall health. Recommendations may include:
- Low-salt Diet: To manage blood pressure.
- Protein Restriction: In some cases, to reduce the workload on the kidneys.
- Healthy Weight Management: To reduce the risk of further kidney damage.
- Regular Exercise: To improve cardiovascular health.
Consulting with a dietitian or a healthcare provider is crucial for personalized advice.
What are the potential side effects of FSGS treatments?
The side effects of FSGS treatments vary depending on the medication and the individual. Common side effects may include weight gain, increased susceptibility to infections, and changes in blood sugar levels. It is important to discuss the potential side effects with your healthcare provider.
Can FSGS lead to kidney failure?
Yes, without appropriate treatment, FSGS can lead to kidney failure. Early diagnosis and treatment are essential to slow down the progression of the disease and preserve kidney function.
How often should someone with FSGS see a doctor?
Regular monitoring is crucial for anyone diagnosed with FSGS. The frequency of doctor visits depends on the severity of the condition, the effectiveness of the treatment plan, and the presence of symptoms or complications. Typically, patients should expect to see their healthcare provider every 3 to 6 months.
Can FSGS recur after treatment?
FSGS can recur, especially in individuals who have had a kidney transplant. The recurrence rate varies, but it is a concern for those undergoing transplantation. Ongoing monitoring and treatment adjustments are essential for managing FSGS.
Conclusion
In this comprehensive overview, we’ve navigated through the intricate landscape of Focal Segmental Glomerulosclerosis (FSGS), a complex kidney disorder that poses significant challenges to patients and healthcare providers alike. We’ve dissected its causes, delved into the symptoms, and explored the current treatments available, alongside the promising research that continues to evolve in this field. The importance of early diagnosis cannot be overstated, as it opens the door to effective management and potentially slows the progression of the disease. Moreover, a thorough and individualized treatment plan is paramount in addressing the unique needs of each patient, enhancing their quality of life and overall health outcomes.
The journey through FSGS treatment is ever-evolving, and staying abreast of the latest developments is crucial for both patients and healthcare professionals. Advances in medical research are continually offering new hope and possibilities for treatment, making it essential to remain informed and engaged with the latest findings and therapeutic approaches.
To those navigating the challenges of FSGS, let this article serve as a reminder of the power of knowledge and the importance of a proactive approach to healthcare. By fostering open communication between patients and providers, and prioritizing early diagnosis and personalized treatment plans, we can collectively enhance the management of FSGS. Let us move forward with optimism, armed with the latest insights and a commitment to improving the lives of those affected by this condition. Together, we can make strides in the fight against FSGS, offering hope and improved care for patients around the globe.