Esophageal Varices Symptoms: Esophageal varices are enlarged or swollen veins on the lining of the esophagus, the tube that connects the throat to the stomach.
This condition is serious and can lead to life-threatening bleeding. Understanding the symptoms and causes of esophageal varices is crucial for early detection and effective management.
Understanding Esophageal Varices
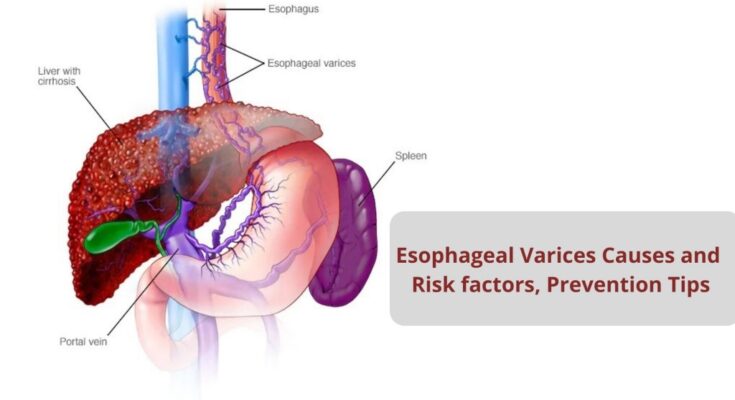
Esophageal varices are swollen veins in the lining of the lower esophagus, near the stomach. These enlarged veins are a serious concern, primarily because they result from increased pressure in the veins that carry blood to the liver, known as portal hypertension, and have a high risk of bleeding. Understanding how esophageal varices develop, their relationship with liver health, and their prevalence can help individuals grasp the seriousness of this condition and encourage proactive healthcare.
How Esophageal Varices Develop in the Body
The development of esophageal varices begins with portal hypertension, which is an increase in the pressure within the portal vein system. This system includes veins coming from the stomach, pancreas, and spleen that merge into the portal vein which then branches into smaller veins in the liver. When blockages or resistance in the liver impede the normal flow of blood, pressure builds up. This forces the blood to find alternate pathways back to the heart, often through smaller, less capable veins in the esophagus. Over time, these veins swell and can become varices.
Factors that contribute to the development of portal hypertension and, consequently, esophageal varices include chronic liver diseases such as cirrhosis. Cirrhosis involves the scarring of liver tissue which hampers the organ’s ability to function properly, leading to complications such as esophageal varices.
The Role of the Liver in Esophageal Varices
The liver plays a central role in the development of esophageal varices. As a vital organ, it processes nutrients, filters toxins, produces blood clotting factors, and performs many other critical functions. When the liver is damaged, whether by alcohol abuse, viral hepatitis, or other factors, it can lead to cirrhosis. Cirrhosis is the final stage of liver scarring that impedes blood flow through the liver, causing portal hypertension. It’s this increased pressure that forces blood into smaller vessels, like those in the esophagus, leading to varices.
Understanding the health of your liver and taking steps to prevent liver disease are essential measures in reducing the risk of developing esophageal varices. This includes moderating alcohol consumption, maintaining a healthy weight, and managing chronic conditions that can affect the liver.
Prevalence and Statistics
Esophageal varices are more common than many might think, especially among individuals with liver disease. It is estimated that about 50% of people with cirrhosis will develop esophageal varices. Furthermore, the risk of bleeding from varices is significantly high, occurring in about 30% of patients with diagnosed varices over a period of two years. The mortality rate associated with the first bleeding episode is high, emphasizing the need for early diagnosis and treatment.
Given their prevalence and the serious risk they pose, understanding esophageal varices is crucial. Individuals with liver disease or at risk of liver complications should be vigilant about monitoring their health and seeking regular medical advice to prevent or manage this condition.
However, esophageal varices are a significant health concern stemming from liver disease and portal hypertension. Their development, closely linked to the health of the liver, underscores the importance of liver care in preventive health strategies. With considerable prevalence among those with liver disease, awareness, and early intervention are key to managing the risks associated with esophageal varices.
Symptoms of Esophageal Varices
Understanding the symptoms is crucial for early detection and management. This guide will help you recognize the early signs, major symptoms, and the complications of untreated esophageal varices. We’ll also discuss when it’s critical to seek medical attention.
Early Signs and Why They Often Go Unnoticed
Esophageal varices often develop slowly, making the early signs easy to overlook. Initially, there may be no symptoms, or they might be so mild that they’re mistaken for less serious health issues. Some individuals may experience a slight discomfort or fullness in the upper abdomen, but these symptoms are frequently dismissed as indigestion or heartburn. The subtlety of these early signs contributes to the condition frequently going unnoticed until more severe symptoms appear or complications arise.
Major Symptoms to Watch Out For
As esophageal varices progress, more noticeable symptoms can emerge. Key symptoms include:
- Vomiting blood: This alarming symptom is often a sign of bleeding varices and requires immediate medical attention.
- Black, tarry stools: Also known as melena, this symptom indicates bleeding in the upper gastrointestinal tract.
- Paleness and fatigue: These could be signs of anemia, which may result from chronic blood loss.
- Jaundice: Yellowing of the skin and eyes, indicating liver dysfunction, which is a common underlying cause of esophageal varices.
Recognizing these symptoms early can be life-saving, as bleeding esophageal varices are a medical emergency.
Complications and Risks Associated with Untreated Esophageal Varices
If left untreated, esophageal varices can lead to serious complications. The most severe risk is the rupture of the varices, which can cause life-threatening bleeding. Other potential complications include:
- Shock: Due to the sudden loss of blood, leading to dangerously low blood pressure.
- Anemia: Chronic blood loss can lead to a significant decrease in red blood cells, causing fatigue and weakness.
- Infection: In severe cases, an infection can develop in the bloodstream.
Prompt treatment can help manage esophageal varices and reduce the risk of these serious complications.
When to Seek Medical Help
Immediate medical attention is critical if you experience any of the major symptoms of esophageal varices, especially vomiting blood or noticing black, tarry stools. Additionally, if you have a liver condition or are at risk for esophageal varices, regular check-ups with your healthcare provider are essential. Early diagnosis and treatment can prevent complications and significantly improve outcomes.
Understanding the symptoms and risks associated with esophageal varices is crucial for those at risk of this condition. By staying informed and vigilant, you can take the necessary steps to protect your health and seek timely medical care.
Causes of Esophageal Varices
Understanding the causes and contributing factors is crucial for prevention and management. This article explores the connection between liver disease and esophageal varices, other contributing factors and conditions, and the process of varices formation in the esophagus.
The Connection Between Liver Disease and Esophageal Varices
Liver disease is the primary cause of esophageal varices. Conditions such as cirrhosis (scarring of the liver) impede normal blood flow through the liver. This blockage increases the pressure in the portal vein (portal hypertension), which is the main vessel that carries blood from the digestive organs to the liver. The elevated pressure forces the blood to find alternative pathways back to the heart, often rerouting it through smaller, weaker vessels in the esophagus and stomach. These veins are not designed to handle such high pressure, leading to their dilation and the formation of varices.
Other Contributing Factors and Conditions
While liver disease is the predominant cause, other conditions can also contribute to the development of esophageal varices. These include:
- Blood Clotting Disorders: Conditions that cause blood clots in the portal vein or its branches can lead to increased pressure and varices.
- Parasitic Infections: Certain infections, like schistosomiasis, can damage the liver and the portal vein, leading to varices.
- Congenital Heart Conditions: Some heart conditions present from birth can affect blood flow and pressure, potentially leading to the development of esophageal varices.
It is also possible for individuals without liver disease to develop esophageal varices, though this is less common.
The Process of Varices Formation in the Esophagus
The formation of esophageal varices is a gradual process influenced by increased pressure in the portal vein system. Here’s a simplified explanation of the process:
- Increased Pressure: Liver disease or other conditions lead to increased pressure in the portal vein.
- Seeking Alternate Routes: The blood seeks alternative pathways to bypass the liver, flowing through smaller veins that connect to the esophagus.
- Vein Dilation and Weakness: The small veins in the esophagus are not designed to carry such high volumes of blood at increased pressure. Over time, this causes the veins to dilate and swell, forming varices.
- Risk of Rupture: As varices grow larger and their walls become thinner, they are at a higher risk of rupturing, which can lead to life-threatening bleeding.
However, understanding the causes and process behind the formation of esophageal varices is crucial for effective management and prevention strategies. Regular monitoring and medical interventions can help reduce the risk of complications associated with esophageal varices, particularly in individuals with liver disease or other risk factors.
Diagnosing Esophageal Varices: A Comprehensive Guide
Diagnosing this condition promptly is crucial to prevent potential complications. This guide explores common diagnostic tests and procedures, how symptoms influence the diagnosis process, and the pivotal role of endoscopy in diagnosing esophageal varices.
Common Diagnostic Tests and Procedures
- Endoscopy: The primary tool for diagnosing esophageal varices. It involves using a thin, flexible tube with a camera (endoscope) to visually inspect the esophagus, stomach, and beginning of the small intestine.
- Blood Tests: Often conducted to assess liver function and to check for signs of liver disease or portal hypertension, conditions that can lead to esophageal varices.
- Imaging Tests: Techniques like ultrasound, CT scans, or MRI can be employed to visualize the blood flow in and around the liver, detecting abnormalities that might contribute to the development of varices.
- Capsule Endoscopy: A less invasive option where the patient swallows a small, pill-sized camera that captures images of the esophagus as it passes through the digestive tract.
How Symptoms Influence the Diagnosis Process
The diagnosis process often begins when a patient presents symptoms indicative of esophageal varices. These symptoms may include vomiting blood, black or tarry stools, and signs of chronic liver disease. Recognizing these symptoms early is crucial for healthcare providers to initiate the appropriate diagnostic tests, particularly if the patient has a history of liver disease. The presence of such symptoms directs the diagnostic focus towards assessing the severity of the varices and the risk of bleeding.
The Role of Endoscopy in Diagnosing Esophageal Varices
Endoscopy stands at the forefront of diagnosing esophageal varices. It not only confirms the presence of varices but also evaluates their size, which is critical for assessing the risk of bleeding. During the procedure, doctors can also perform variceal banding or injection sclerotherapy if varices are found, treating them immediately to prevent bleeding. This direct visualization and the ability to take immediate therapeutic actions make endoscopy indispensable in managing esophageal varices.
The timely and accurate diagnosis of esophageal varices is essential for initiating appropriate treatment and preventing potential complications. Through a combination of detailed symptom analysis, blood tests, imaging procedures, and, most importantly, endoscopy, healthcare providers can effectively diagnose and manage this condition. Understanding the crucial role of these diagnostic procedures can empower patients and families navigating the complexities of esophageal varices.
Treatment Options for Esophageal Varices
Understanding the available treatment options, including non-invasive methods, medical treatments, and the latest advances, is crucial for patients and their families. This article explores the various treatment avenues for managing esophageal varices effectively.
Non-Invasive Treatment Options and Lifestyle Changes
Managing esophageal varices doesn’t always start with surgery or medication. Non-invasive treatments and lifestyle adjustments can play a pivotal role in treatment. Here’s what you need to know:
- Dietary Modifications: Implementing a low-sodium diet helps reduce the risk of further swelling in the varices.
- Limiting Alcohol and Smoking: Both alcohol and smoking can exacerbate esophageal varices. Eliminating or significantly reducing consumption is advised.
- Weight Management: Achieving and maintaining a healthy weight can reduce pressure on the veins and help manage symptoms.
- Regular Monitoring: Non-invasive imaging tests, like endoscopies, allow doctors to monitor the varices closely without surgery.
These lifestyle adjustments not only support your treatment plan but also enhance your overall health.
Medical Treatments and Procedures
When lifestyle changes are not enough to manage esophageal varices, medical interventions may be necessary. The following treatments are commonly used:
- Beta-Blockers: Medications such as propranolol or nadolol can reduce blood pressure in the veins, lessening the risk of bleeding.
- Endoscopic Variceal Ligation (EVL): This procedure involves using a special band to tie off bleeding varices.
- Endoscopic Sclerotherapy: A doctor injects a solution into the varices during an endoscopy to shrink them.
- Transjugular Intrahepatic Portosystemic Shunt (TIPS): This is a more invasive procedure that creates a new path for blood flow, reducing pressure on the varices.
These treatments and procedures are tailored to the individual’s condition and the severity of the varices.
Advances in Treatment and Research
The landscape of esophageal varices treatment is continually evolving, with research making significant strides:
- Novel Drug Therapies: Ongoing research into new medications aims to more effectively manage portal hypertension, the root cause of esophageal varices.
- Improved Endoscopic Techniques: Advances in endoscopic technology enhance the safety and effectiveness of treatments like EVL and sclerotherapy.
- Minimally Invasive Surgical Options: The development of less invasive surgical methods reduces recovery time and improves patient outcomes.
- Personalized Medicine: Tailoring treatment plans to the individual’s genetic makeup and the specific characteristics of their condition represents the future of esophageal varices management.
By staying informed about the latest treatment options and engaging in open dialogue with healthcare providers, patients can navigate the complexities of managing esophageal varices more effectively.
Preventing Esophageal Varices
While the prospect of developing esophageal varices can be daunting, there are effective strategies to prevent their formation. Understanding the importance of managing liver health and undergoing regular screenings, especially for at-risk individuals, is crucial in preventing this potentially life-threatening condition.
Strategies to Prevent the Development of Varices
1. Maintain a Healthy Liver: The most direct strategy to prevent esophageal varices is to keep your liver in good health. This involves adopting a lifestyle that supports liver function, including a balanced diet rich in fruits, vegetables, and lean protein. Avoiding excessive alcohol consumption and managing body weight can significantly reduce the risk of liver diseases that lead to varices.
2. Control Liver Diseases: For individuals already living with liver diseases, such as hepatitis or fatty liver disease, closely managing these conditions is vital. Medications and lifestyle changes prescribed by healthcare providers can slow the progression of liver damage and, consequently, the development of esophageal varices.
3. Medication Use: In some cases, doctors prescribe medications to reduce the risk of varices forming in those with known liver issues or portal hypertension. Beta-blockers, for example, are often used to lower blood pressure in the veins supplying the liver, reducing the risk of varices.
Importance of Managing Liver Health
The liver plays a critical role in processing nutrients, filtering toxins, and a host of other vital functions. Damaged liver health can lead to conditions like esophageal varices that not only pose significant health risks but also compromise the liver’s ability to perform its essential duties. By prioritizing liver health through a healthy lifestyle and proper management of liver conditions, individuals can significantly reduce the likelihood of developing complications like varices.
Regular Screenings for At-risk Individuals
Early detection of liver disease and the potential for esophageal varices is key to prevention. Regular screenings, including blood tests and imaging studies like ultrasounds, are crucial for individuals at risk of liver diseases. These screenings can detect early signs of liver dysfunction or portal hypertension, allowing for timely intervention before varices develop. High-risk groups, such as those with chronic liver disease or a history of liver issues, should adhere to a regular screening schedule as recommended by their healthcare provider.
However, while the threat of esophageal varices is significant for individuals with liver disease, a proactive approach to liver health can greatly reduce this risk. By maintaining a healthy lifestyle, managing existing liver conditions, considering preventive medications, and adhering to regular screening recommendations, at-risk individuals can protect themselves against the development of esophageal varices. This multifaceted approach emphasizes the importance of liver health in overall well-being and the prevention of serious complications.
Living with Esophageal Varices: A Comprehensive Guide
Living with esophageal varices requires careful management and lifestyle adjustments to maintain health and prevent complications. Esophageal varices are enlarged veins in the esophagus that can bleed if they rupture. Therefore, it’s crucial for individuals diagnosed with this condition to understand how lifestyle modifications, dietary recommendations, monitoring symptoms, and regular medical follow-ups play a vital role in managing their health.
Lifestyle Modifications and Diet Recommendations
Lifestyle Modifications: Implementing certain lifestyle changes can significantly reduce the risk of complications associated with esophageal varices. Here are some key modifications:
- Avoid Alcohol: Alcohol can exacerbate liver conditions and increase the risk of bleeding. Abstaining from alcohol is crucial.
- Quit Smoking: Smoking may worsen the condition of your liver and esophagus. Seeking help to quit smoking is beneficial.
- Manage Weight: Maintaining a healthy weight reduces the strain on your liver and can help manage symptoms.
- Exercise Regularly: Gentle, low-impact exercises can improve overall health without putting too much strain on your body. Consult your doctor for suitable exercises.
Diet Recommendations: A balanced diet plays a critical role in managing esophageal varices. Here are some dietary tips:
- Low-Sodium Diet: High salt intake can lead to fluid accumulation, worsening pressure in the veins. Aim for a low-sodium diet to help manage this risk.
- Eat Small, Frequent Meals: Smaller, more frequent meals can reduce pressure in the stomach and esophagus.
- High-Fiber Foods: Foods high in fiber can prevent constipation, reducing the risk of straining that can cause varices to bleed.
- Lean Proteins: Incorporate lean proteins like chicken, fish, and legumes, which are easier on the liver.
Monitoring and Managing Symptoms
Being vigilant about symptom changes is crucial for individuals with esophageal varices. Key symptoms to monitor include:
- Signs of Bleeding: Such as vomiting blood or passing black, tarry stools. These symptoms require immediate medical attention.
- Fatigue and Weakness: These can be indicators of anemia or bleeding and should be communicated to your healthcare provider.
- Abdominal Pain and Swelling: Notify your doctor if you experience increased pain or swelling, as this could indicate complications.
The Importance of Regular Medical Follow-Ups
Regular check-ups with a healthcare provider are essential for monitoring the condition of esophageal varices and making necessary adjustments to treatment plans. These appointments often include:
- Endoscopic Examinations: To monitor the size and condition of varices.
- Blood Tests: To assess liver function and overall health.
- Adjusting Medications: Based on the progression of your condition, medications may be adjusted to optimize treatment.
Living with esophageal varices requires a proactive approach to health management. Through lifestyle modifications, dietary adjustments, vigilant symptom monitoring, and regular medical follow-ups, individuals can manage their condition effectively and reduce the risk of complications. Remember, each person’s situation is unique, so it’s important to work closely with healthcare professionals to tailor these recommendations to your specific needs.
FAQs on Esophageal Varices
What Are Esophageal Varices?
Esophageal varices are swollen veins in the lining of the lower esophagus near the stomach. They are often associated with serious liver diseases and conditions that increase pressure in the veins (portal hypertension). Due to their fragile nature, they pose a risk of bleeding, which can be life-threatening.
What Causes Esophageal Varices?
The primary cause of esophageal varices is increased pressure in the portal vein system, typically due to liver cirrhosis. Cirrhosis leads to obstruction of blood flow through the liver, causing blood to back up into the portal vein system. Other causes may include blood clots in the portal vein or a parasitic infection known as schistosomiasis.
What Are the Symptoms of Esophageal Varices?
In many cases, esophageal varices don’t present any symptoms until they bleed. Signs of bleeding varices include vomiting blood, black or bloody stools, lightheadedness, and shock. It’s crucial to seek immediate medical attention if you experience these symptoms.
How Are Esophageal Varices Diagnosed?
Doctors often diagnose esophageal varices during an endoscopy, where a flexible tube with a camera (endoscope) is inserted down your throat to examine the esophagus, stomach, and the beginning of the small intestine. Other diagnostic tools might include blood tests, imaging tests such as ultrasound or CT scans to evaluate the liver and portal vein.
What Treatments Are Available for Esophageal Varices?
Treatment focuses on preventing bleeding and managing it if it occurs. Options include:
- Medications: Beta blockers can reduce portal blood pressure, lessening the risk of bleeding.
- Endoscopic Therapy: Procedures like banding or sclerotherapy help manage bleeding varices.
- Shunt Procedures: TIPS (transjugular intrahepatic portosystemic shunt) is a procedure to redirect blood flow within the liver and reduce pressure in the varices.
- Liver Transplant: In severe cases, especially for those with advanced liver disease, a liver transplant may be considered.
How Can I Prevent Esophageal Varices from Bleeding?
Preventive measures include regular medical checkups, medication to reduce portal hypertension, endoscopic surveillance to monitor the size and risk of varices, and lifestyle changes. Reducing alcohol intake and managing liver diseases effectively are crucial steps in prevention.
Can Esophageal Varices Be Cured?
While there’s no cure for esophageal varices per se, the focus is on managing the underlying liver condition and preventing complications such as bleeding. Successful management of liver disease can prevent the formation or worsening of varices.
What Is the Prognosis for Someone with Esophageal Varices?
The prognosis varies depending on the severity of the liver disease, the size of the varices, and whether bleeding occurs. Early detection and treatment of liver disease can improve outcomes and reduce the risk of developing esophageal varices.
Conclusion
In wrapping up our discussion on esophageal varices, it’s crucial to revisit the significance of recognizing the symptoms and comprehending the causes of this condition. Esophageal varices, which are enlarged veins in the esophagus, pose a severe risk of bleeding and are often a complication of liver disease. Understanding the symptoms—such as black or bloody stools, vomiting blood, and signs of shock—can be lifesaving. Equally important is an awareness of the causes, primarily cirrhosis of the liver, which underscores the necessity of addressing liver health proactively.
For individuals at risk, this knowledge serves as a powerful tool. It not only empowers you to identify potential warning signs early but also highlights the importance of regular medical consultations. Seeking advice from healthcare professionals on a regular basis is essential for monitoring liver health, managing any underlying conditions, and implementing preventive measures against complications like esophageal varices.
We encourage everyone, especially those with liver conditions or other risk factors, to prioritize their health. Regular medical advice can lead to early detection and timely intervention, significantly reducing the risks associated with esophageal varices. Your health is invaluable, and taking proactive steps to protect it is of paramount importance. Stay informed, stay vigilant, and never hesitate to seek medical advice for your well-being.
This understanding and approach towards managing esophageal varices not only enhance your quality of life but also contribute to broader health awareness and prevention efforts. Let’s prioritize health, seek regular medical advice, and support each other in maintaining a healthy, informed community.
References
For further reading and validation of the information provided regarding the symptoms of esophageal varices, we have compiled a list of reputable sources. These links lead to authoritative medical websites and publications, ensuring you have access to reliable and up-to-date information:
- Mayo Clinic offers an in-depth overview of esophageal varices, including symptoms, causes, and treatment options. A trusted resource for comprehensive health information. Visit Mayo Clinic.
- PubMed, a free search engine accessing primarily the MEDLINE database of references and abstracts on life sciences and biomedical topics, contains various research articles and studies on esophageal varices. For those interested in the scientific and research aspect, this is a goldmine of information. Search PubMed.
By consulting these sources, readers can deepen their understanding of esophageal varices, including the symptoms, causes, and available treatments. Each link leads to a resource that has been carefully selected for its credibility and authority in the field of medicine.