Endometriosis Symptoms: Endometriosis is a chronic condition that affects millions of women worldwide, significantly impacting their quality of life.
It occurs when tissue similar to the lining inside the uterus, known as the endometrium, grows outside the uterus, causing a range of symptoms and potential complications.
Understanding the symptoms and causes of endometriosis is crucial for early detection and effective management of this complex condition.
What is Endometriosis?
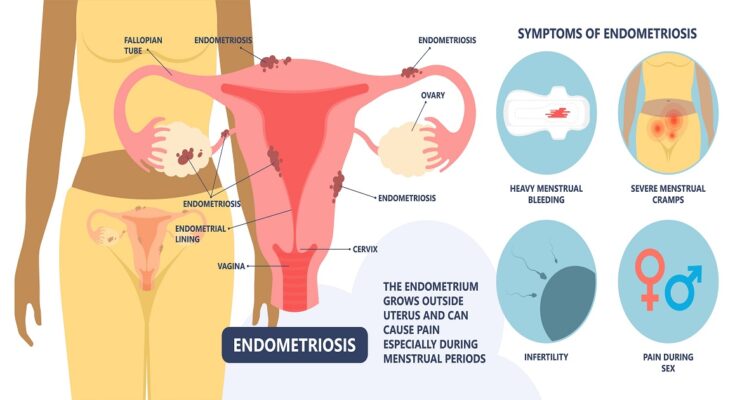
Endometriosis is a chronic, often painful condition that affects women’s reproductive organs. It occurs when the type of tissue that typically lines the inside of the uterus—known as the endometrium—begins to grow outside the uterus. This misplaced tissue can appear on the ovaries, fallopian tubes, the outer surface of the uterus, and other organs within the pelvis. Despite its abnormal location, this tissue behaves as it normally would: it thickens, breaks down, and bleeds with each menstrual cycle. However, since it has no way to exit the body, it becomes trapped, leading to various complications, including cysts, inflammation, and scar tissue.
One of the hallmarks of endometriosis is its symptomatology, which can vary significantly from one individual to another. Some women experience severe pain, especially during menstruation, sexual intercourse, or bowel movements. Others might have difficulty getting pregnant or not exhibit any symptoms at all. The severity of the condition does not necessarily correlate with the level of pain or other symptoms experienced, making diagnosis and management challenging.
Statistics on Prevalence and Demographics Affected
Endometriosis is a common gynecological condition, impacting an estimated 1 in 10 women during their reproductive years, which roughly translates to around 176 million women worldwide. While it can occur at any age, it is most commonly diagnosed in women in their 30s and 40s.
The condition does not discriminate by race or ethnicity, affecting women of all backgrounds. However, certain factors may increase a woman’s risk of developing endometriosis, including having a family history of the condition, never giving birth, experiencing menstrual periods that last longer than seven days, or having menstrual cycles shorter than 28 days.
Despite its prevalence, endometriosis is often underdiagnosed or misdiagnosed, partly due to the variability of its symptoms and their similarity to other conditions. This underscores the importance of awareness and understanding of the condition, not only among women and health practitioners but also across the wider community.
Symptoms of Endometriosis
Understanding the common symptoms associated with endometriosis is crucial for early detection and management. Here, we provide a detailed list of these symptoms, explain how they can vary, and highlight when it’s essential to see a doctor for a professional evaluation.
Common Symptoms of Endometriosis
- Pelvic Pain: The hallmark of endometriosis is pelvic pain, often associated with menstrual periods. Many women experience cramping during their menstrual cycle, but those with endometriosis typically describe menstrual pain that’s far worse than usual. This pain can also increase over time.
- Menstrual Irregularities: Heavy periods (menorrhagia) or bleeding between periods (menometrorrhagia) can be a sign of endometriosis.
- Pain During Intercourse: Pain during or after sex is another common symptom of endometriosis. This pain can affect a person’s relationships and quality of life significantly.
- Pain with Bowel Movements or Urination: Women with endometriosis may experience discomfort during bowel movements or urination, especially during menstrual periods.
- Infertility: Endometriosis can also lead to difficulties in getting pregnant. In fact, some women discover they have endometriosis only after seeking treatment for infertility.
- Other Symptoms: These can include fatigue, diarrhea, constipation, bloating, or nausea, especially during menstrual periods.
Variability of Symptoms
It’s important to note that the severity of endometriosis does not always correlate with the level of pain experienced or the range of symptoms. Some women with mild endometriosis can have severe pain, while others with advanced endometriosis may have little to no discomfort. Additionally, the type of symptoms can vary widely from one individual to another, making endometriosis a particularly challenging condition to diagnose based solely on symptom presentation.
When to See a Doctor
If you’re experiencing any of the symptoms mentioned above, especially if they interfere with your daily activities or are accompanied by fertility issues, it’s crucial to seek professional medical advice. Key signs that indicate a need for an evaluation include:
- Severe or worsening menstrual pain
- Chronic pelvic pain
- Painful intercourse that affects your relationship or well-being
- Symptoms that don’t improve with over-the-counter pain medication
- Difficulty getting pregnant after trying for six months to a year
Early diagnosis and treatment can help manage the symptoms of endometriosis and improve your quality of life. Don’t hesitate to consult your doctor if you suspect you might have endometriosis.
However, understanding the symptoms of endometriosis and recognizing when to seek professional help are essential steps in managing this complex condition. By being informed and proactive about your health, you can navigate the challenges of endometriosis more effectively.
Causes and Risk Factors of Endometriosis
Understanding the potential causes and risk factors can help in early detection and management. Here’s a comprehensive look into what may lead to the development of endometriosis and the factors that might increase one’s likelihood of being diagnosed with this condition.
Theories on the Causes of Endometriosis
While the exact cause of endometriosis remains unknown, several theories have been proposed to explain its development:
- Retrograde Menstruation: This theory suggests that during menstruation, some of the menstrual blood flows back through the fallopian tubes into the pelvic cavity instead of leaving the body. This blood contains endometrial cells, which then stick to the pelvic walls and surfaces of pelvic organs, where they grow and continue to bleed over the course of each menstrual cycle.
- Embryonic Cell Transformation: Hormones such as estrogen might transform embryonic cells — cells in the earliest stages of development — into endometrial cell implants during puberty.
- Surgical Scar Implantation: After surgeries like a hysterectomy or C-section, endometrial cells might attach to the surgical incision.
- Immune System Disorders: A malfunction in the immune system may make the body unable to recognize and destroy endometrial-like tissue that’s growing outside the uterus.
Risk Factors That Increase the Likelihood of Developing Endometriosis
Certain factors can raise the risk of developing endometriosis:
- Family History: Having a close relative with endometriosis increases your risk, suggesting a possible genetic component.
- Menstrual History: Long menstrual cycles, short menstrual cycles, heavy menstrual flow, or having your period start at an early age can increase your risk.
- Age: Endometriosis is most commonly diagnosed in women in their 30s and 40s, but it can start at any age after menstruation begins.
- Medical Conditions Related to Estrogen Production: Conditions that increase the body’s production of estrogen, or where treatment involves estrogen, can heighten the risk of developing endometriosis.
- Reproductive Tract Abnormalities: Women born with a reproductive tract anomaly that blocks or alters the flow of menstrual blood from the uterus through the vagina may have an increased risk of developing endometriosis.
If you have concerns about endometriosis, especially if you have a family history or other risk factors, consult with a healthcare professional. Early intervention can make a significant difference in managing the condition and improving quality of life.
Diagnosis of Endometriosis
Its diagnosis is crucial but can be challenging due to its varied and nonspecific symptoms. Understanding the diagnostic process, the significance of early detection, and the obstacles faced during diagnosis can empower individuals and improve outcomes.
Diagnostic Process for Endometriosis
The journey to a definitive diagnosis of endometriosis typically involves several steps. Each is designed to gather critical information about the symptoms and their impact on the individual’s health:
- Medical History Review: The first step involves a detailed discussion of the patient’s symptoms, menstrual cycles, family history of endometriosis, and any previous diagnoses or treatments.
- Pelvic Examination: A pelvic exam allows healthcare providers to feel for abnormalities, such as cysts on the reproductive organs or scars behind the uterus. However, small areas of endometriosis can be difficult to feel, making further testing necessary.
- Ultrasound: This imaging test uses high-frequency sound waves to create images of the inside of the pelvis. It can identify cysts associated with endometriosis (endometriomas), although it can’t definitively diagnose endometriosis.
- Magnetic Resonance Imaging (MRI): An MRI provides detailed images of organs and tissues. It can be particularly helpful in planning surgery for removing endometriosis lesions.
- Laparoscopy: Considered the gold standard for diagnosing endometriosis, this minimally invasive surgery involves inserting a scope through a small incision near the navel to look for endometrial tissue outside the uterus. It allows for definitive diagnosis and, in some cases, treatment.
Importance of Early Diagnosis
Early diagnosis of endometriosis is critical for several reasons. It can:
- Reduce Long-term Pain: Early treatment can manage symptoms and prevent worsening pain.
- Preserve Fertility: Endometriosis can affect fertility; diagnosing and treating it early can improve reproductive outcomes.
- Improve Quality of Life: Managing symptoms can significantly enhance an individual’s quality of life and psychological well-being.
Challenges in Diagnosing Endometriosis
Despite the structured approach to diagnosis, several challenges can impede timely identification:
- Symptom Overlap: Symptoms of endometriosis, like pelvic pain and menstrual irregularities, overlap with those of other conditions, leading to misdiagnosis or delays.
- Lack of Awareness: Both patients and healthcare providers may lack awareness of endometriosis, which can delay seeking or providing medical attention.
- Need for Surgery for Definitive Diagnosis: Since laparoscopy is required for a conclusive diagnosis, there can be hesitance due to the invasive nature of the procedure.
- Variability of Symptoms: The severity of symptoms does not always correlate with the extent of the disease, making it challenging to prioritize cases based on symptom presentation alone.
Early detection is paramount to managing symptoms, preserving fertility, and improving the quality of life. Overcoming the obstacles to diagnosis requires increased awareness and understanding among both patients and healthcare professionals. By acknowledging these challenges and emphasizing the importance of early diagnosis, we can work towards better outcomes for those affected by endometriosis.
Treatment Options for Endometriosis
Endometriosis is a chronic condition that affects millions of women worldwide. It can cause severe pain, irregular bleeding, and fertility issues. Fortunately, there are various treatment options available to manage symptoms and improve quality of life. This article explores non-surgical treatments, surgical options, and fertility treatments for women with endometriosis, especially those trying to conceive.
Non-Surgical Treatments
Non-surgical treatments are often the first line of defense against endometriosis symptoms. These include:
- Pain Management: Over-the-counter (OTC) pain relievers like ibuprofen and naproxen can help manage menstrual cramps and pain associated with endometriosis. For more severe pain, your doctor may prescribe stronger medications.
- Hormone Therapy: Hormonal treatments can help reduce or eliminate the pain of endometriosis. Birth control pills, patches, and vaginal rings can help regulate the menstrual cycle and lessen the severity of symptoms. Gonadotropin-releasing hormone (GnRH) agonists and antagonists can also be used to reduce estrogen levels, which may temporarily halt the progression of endometriosis.
- Physical Therapy: Some women find relief through physical therapy techniques, which can help alleviate pelvic pain.
Surgical Options
When non-surgical treatments are not effective, surgery may be considered to remove endometriosis implants and scar tissue. The main surgical options include:
- Laparoscopy: A minimally invasive procedure that allows the doctor to remove endometriosis implants and scar tissue. This surgery can reduce pain and improve fertility.
- Laparotomy: A more extensive surgery used in severe cases of endometriosis or when the disease has spread widely in the abdomen.
- Hysterectomy: The surgical removal of the uterus and possibly ovaries and fallopian tubes. This option is generally considered a last resort, typically for women who have completed their families or when other treatments have failed.
Fertility Treatment Options for Women with Endometriosis Trying to Conceive
Endometriosis can affect fertility, but many women with the condition can still conceive, either naturally or with assistance. Fertility treatment options include:
- Fertility Medications: Drugs that stimulate ovulation can help increase the chances of pregnancy.
- Intrauterine Insemination (IUI): A procedure where sperm is placed directly into the uterus during ovulation.
- In Vitro Fertilization (IVF): A more advanced fertility treatment where eggs are fertilized outside the body and then implanted in the uterus. IVF may be recommended if other treatments have not been successful.
It’s essential to work closely with a healthcare provider to determine the most appropriate treatment plan based on your individual symptoms, the severity of your endometriosis, and your fertility goals. With the right approach, most women with endometriosis can manage their symptoms effectively and pursue a healthy pregnancy.
Managing Endometriosis Symptoms at Home
Living with endometriosis can be challenging, but there are effective strategies you can employ at home to manage its symptoms. These involve a combination of lifestyle adjustments, home remedies, and tapping into valuable support and resources. Implementing these changes can significantly improve your quality of life and help you regain control.
Lifestyle Changes and Home Remedies
- Dietary Modifications: Adopting an anti-inflammatory diet can help reduce endometriosis symptoms. Incorporate foods rich in omega-3 fatty acids, such as salmon and flaxseeds, and increase your intake of fruits, vegetables, and whole grains. Avoid processed foods, red meat, and excessive caffeine and alcohol, as they can exacerbate symptoms.
- Regular Exercise: Engaging in regular, moderate exercise can alleviate pain and reduce stress. Activities like yoga, Pilates, and low-impact aerobic exercises can be particularly beneficial. Exercise also helps in managing estrogen levels, which can play a role in endometriosis symptoms.
- Stress Management: Techniques such as mindfulness, meditation, and deep-breathing exercises can help manage stress levels, which may, in turn, reduce the severity of symptoms. Consider setting aside time each day for these practices.
- Heat Therapy: Applying heat to the lower abdomen can ease menstrual cramps and pelvic pain. Use a heating pad or a hot water bottle for 15-20 minutes at a time to provide relief.
- Natural Supplements: Certain supplements, including omega-3 fatty acids, magnesium, and vitamin B1, may help reduce pain and inflammation. However, it’s important to consult with a healthcare provider before starting any supplements, as they can interact with other medications.
Support and Resources: The Importance of Support Groups and Counseling
- Finding Community: Joining endometriosis support groups, either in person or online, can provide invaluable emotional support and practical advice. Sharing experiences and coping strategies with others who understand what you’re going through can be incredibly reassuring and helpful.
- Professional Counseling: For some, the chronic pain and emotional distress associated with endometriosis can lead to feelings of depression and anxiety. Seeking the guidance of a therapist or counselor skilled in dealing with chronic illnesses can offer significant emotional relief and coping mechanisms.
- Educational Resources: Educate yourself about endometriosis through reputable sources. Understanding the condition better can empower you to make informed decisions about your care and communicate more effectively with healthcare providers.
- Advocacy Groups: Engaging with endometriosis advocacy groups can provide additional resources, including information on the latest research, treatment options, and strategies for advocating for your health needs.
By implementing these lifestyle changes and taking advantage of available support and resources, you can significantly improve your ability to manage endometriosis symptoms at home. Remember, it’s important to work closely with your healthcare provider to develop a personalized care plan that’s right for you.
FAQs About Endometriosis
What is endometriosis?
Endometriosis is a medical condition where tissue similar to the lining inside the uterus, called endometrium, grows outside the uterus. This can lead to pain, irregular bleeding, and, in some cases, fertility issues. Endometriosis most commonly involves the ovaries, fallopian tubes, and the tissue lining your pelvis.
What causes endometriosis?
The exact cause of endometriosis is not known. Several theories exist, including retrograde menstruation (where menstrual blood flows back through the fallopian tubes into the pelvic cavity instead of leaving the body), genetic factors, hormonal imbalances, and immune system disorders. However, no single theory explains endometriosis completely.
What are the symptoms of endometriosis?
Symptoms of endometriosis can vary but often include pelvic pain, especially associated with menstrual periods, heavy menstrual bleeding or bleeding between periods, infertility, pain with intercourse, pain with bowel movements or urination, and fatigue. It’s important to note that the severity of pain is not necessarily a reliable indicator of the extent of the condition.
How is endometriosis diagnosed?
Endometriosis can be challenging to diagnose. A doctor will typically review your medical history and symptoms and perform a pelvic examination. Ultrasound or magnetic resonance imaging (MRI) may be used to look for signs of endometriosis, but the only definitive way to diagnose endometriosis is through a surgical procedure called laparoscopy, which allows a doctor to see inside the pelvic cavity.
What are the treatment options for endometriosis?
Treatment for endometriosis may vary depending on the severity of your symptoms and whether you wish to become pregnant. Options include pain relief medications, hormone therapy (to slow endometrial tissue growth), and surgical options to remove endometrial tissue. In severe cases, a hysterectomy (removal of the uterus) may be recommended.
Can endometriosis lead to infertility?
Yes, endometriosis can interfere with fertility. Approximately 30% to 50% of women with endometriosis experience difficulty getting pregnant. Endometrial tissue outside the uterus can affect the function of the ovaries, fallopian tubes, and the uterus, making it harder for sperm and egg to meet or for an embryo to implant.
Is there a cure for endometriosis?
Currently, there is no cure for endometriosis, but the condition can be managed with a combination of treatments. Managing symptoms and preventing the progression of the condition are the primary goals of treatment.
How can I manage endometriosis-related pain?
Pain management strategies include over-the-counter pain relievers, hormone therapies, and lifestyle changes such as regular exercise and stress reduction techniques. In some cases, surgery may be necessary to remove as much endometrial tissue as possible to provide relief.
Conclusion:
We cannot stress enough the importance of seeking professional medical advice if you or someone you know experiences any of the symptoms associated with endometriosis. Early consultation with a healthcare provider can lead to a timely diagnosis, which is essential for managing symptoms and improving quality of life. Healthcare professionals can offer a range of treatments tailored to the individual’s condition and needs, from medication to manage pain and inflammation to surgery for more severe cases.
Remember, you are not alone in this journey. Numerous support groups and resources are available to provide information and support to those affected by endometriosis. Taking the step to seek help is pivotal in navigating this condition, and it’s essential to advocate for your health and well-being.
Don’t let the symptoms of endometriosis take control of your life. If you suspect you have this condition, reach out to a healthcare provider to discuss your symptoms and explore the options available for management and treatment. Your health matters, and taking action is the first step toward relief and recovery.
References
In our effort to provide comprehensive and reliable information about endometriosis symptoms, we’ve referenced several authoritative sources. Below, you’ll find a curated list of links to reputable websites and articles. These resources offer additional insights and research findings on endometriosis, enhancing your understanding of this condition. Whether you’re seeking deeper knowledge or looking for validation of the information presented, these references are invaluable.
- Mayo Clinic – Endometriosis Overview: A detailed guide by one of the leading healthcare institutions, offering insights into symptoms, causes, and treatment options for endometriosis. Read more at Mayo Clinic.
- World Health Organization (WHO) – Information on Endometriosis: WHO provides comprehensive information on endometriosis, including its impact on women’s health globally. Explore WHO’s resources.
- Endometriosis.org – Global Information and Support: An invaluable resource for those seeking in-depth information and support networks related to endometriosis. Visit Endometriosis.org.
- The Endometriosis Foundation of America (EndoFound): Offers educational content, support, and research updates on endometriosis. A great resource for both patients and healthcare professionals. Learn more at EndoFound.
- PubMed Central (PMC) – Latest Research on Endometriosis: For those interested in the scientific and medical research aspect, PMC hosts numerous studies and articles on endometriosis. Browse articles on PMC.
These resources were carefully selected for their credibility and the quality of information they provide on endometriosis. They serve as excellent starting points for anyone looking to understand more about the condition, its symptoms, and potential treatments.