Ear Infection Symptoms: Ear infections, specifically in the middle ear, are a common health issue affecting millions worldwide.
Understanding the symptoms and causes of middle ear infections is crucial for prompt and effective treatment, thereby reducing the risk of complications.
This comprehensive guide will delve into the essential aspects of middle ear infections, offering valuable insights and practical advice.
Understanding Middle Ear Infections
Middle ear infections are common conditions that affect millions of individuals worldwide, particularly children. Understanding the anatomy of the ear and the different types of middle ear infections can help in recognizing symptoms early and seeking appropriate treatment. This guide provides an overview of middle ear infections, emphasizing Acute Otitis Media (AOM) and Otitis Media with Effusion (OME), alongside relevant statistics to illustrate their prevalence.
What is a Middle Ear Infection?
A middle ear infection occurs when the area behind the eardrum, known as the middle ear, becomes inflamed and filled with fluid. The ear is divided into three parts: the outer ear, the middle ear, and the inner ear. The middle ear is connected to the back of the throat by a small tube known as the Eustachian tube. This tube helps equalize pressure and drain fluid from the middle ear. However, when it becomes swollen or blocked due to a cold, allergy, or respiratory infection, fluid can accumulate in the middle ear, leading to infection.
Types of Middle Ear Infections
There are two primary types of middle ear infections, each with its own set of characteristics and implications for health:
- Acute Otitis Media (AOM): This is the most common type of ear infection, characterized by rapid onset and symptoms such as ear pain, fever, and sometimes, an ear discharge. AOM occurs when parts of the ear become infected and swollen, trapping fluid behind the eardrum and causing pain.
- Otitis Media with Effusion (OME): Sometimes after an AOM infection has cleared, fluid can continue to accumulate in the middle ear without causing pain, fever, or acute symptoms. This condition is known as OME. While OME may not show immediate symptoms, it can affect hearing and, in some cases, lead to more serious infections if not monitored.
Incidence Rates
Middle ear infections are a prevalent health issue, especially among children. According to healthcare statistics, about 75% of children experience at least one episode of AOM by the age of 3. Furthermore, OME is most common in children aged 2 to 5 years, but it can occur at any age. These infections are a leading cause of doctor visits and antibiotic prescriptions for children, underlining their significance in pediatric health care.
However, understanding the anatomy of the ear and recognizing the types of middle ear infections are crucial steps in managing and preventing these conditions. With early detection and proper treatment, most individuals recover from middle ear infections without long-term effects on their hearing or overall health. However, given their high prevalence, especially in children, raising awareness and education on this topic remains a priority for healthcare providers and parents alike.
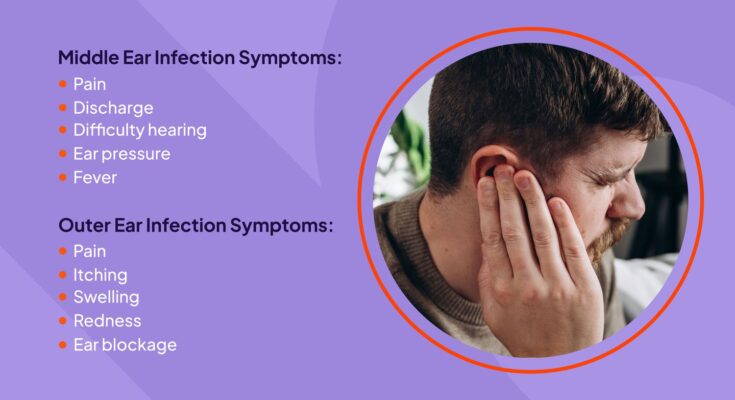
Symptoms of Ear Infections
Identifying the symptoms early can help in seeking timely medical intervention and preventing complications. Here’s a detailed list of common symptoms associated with ear infections.
Common Symptoms of Ear Infections
- Ear Pain: One of the most noticeable symptoms, ear pain can range from mild to severe and might worsen when lying down due to pressure changes.
- Difficulty Hearing: Fluid buildup in the middle ear can cause temporary hearing loss or muffling of sounds.
- Fluid Drainage from the Ear: This may be clear, yellow, or blood-tinged. It’s a sign that the ear drum might have ruptured.
- Fever: Especially common in children, a fever above 100°F (38°C) can accompany an ear infection.
- Headache and Tiredness: The infection can cause general discomfort, leading to headaches and a feeling of being unwell or fatigued.
- Trouble Sleeping: Ear pain and pressure can make it difficult to sleep, particularly for infants and young children.
- Loss of Balance: The inner ear plays a crucial role in maintaining balance, and infections can lead to dizziness or a sense of being unsteady.
When to Seek Medical Attention for Ear Infection Symptoms
While some ear infections may resolve on their own, it’s crucial to know when to seek medical attention to prevent complications.
- Persistent Symptoms: If symptoms like pain, hearing loss, or fever last for more than a day or two, it’s time to consult a healthcare provider.
- Severe Symptoms: Intense pain, high fever (above 102°F or 39°C), or sudden hearing loss should prompt an immediate medical visit.
- Symptoms in Infants: Babies and toddlers who show signs of an ear infection, such as excessive crying, difficulty sleeping, or tugging at their ears, should see a doctor.
- Fluid Drainage: If you notice fluid draining from the ear, especially if it’s pus-like or bloody, seek medical advice.
- Recurring Infections: Frequent ear infections can lead to more serious problems, including hearing issues. If ear infections recur, a healthcare provider might suggest further evaluation.
Identifying and understanding the symptoms of ear infections can greatly assist in managing the condition effectively. Always err on the side of caution and consult with a healthcare provider if you or your child exhibit signs of an ear infection. Early intervention can prevent complications and ensure a quicker recovery.
Causes of Ear Infections
Below, we delve into the main factors leading to ear infections, including bacterial and viral origins, the role of Eustachian tube dysfunction, and various risk factors that can increase susceptibility to this condition.
Bacterial and Viral Infections
The majority of ear infections are caused by bacterial or viral pathogens that invade the ear. These microorganisms can enter the ear canal due to a variety of reasons, such as a cold, flu, or respiratory infection. When bacteria or viruses reach the middle ear, they can cause inflammation and fluid buildup, leading to the painful symptoms associated with ear infections. It’s important to note that while both bacterial and viral infections can lead to ear problems, the treatment approach may differ, emphasizing the importance of proper diagnosis.
Eustachian Tube Dysfunction
A key factor in the development of middle ear infections (otitis media) is the dysfunction of the Eustachian tube. This tube connects the middle ear to the back of the throat and plays a crucial role in ventilating the middle ear, ensuring that the pressure is equalized and that fluids drain properly. When the Eustachian tube is blocked or does not function correctly, fluid can accumulate in the middle ear, creating an ideal environment for infections to develop. Factors such as allergies, colds, and sinus infections can contribute to Eustachian tube dysfunction.
Risk Factors for Ear Infections
Several factors can increase the likelihood of developing an ear infection. These include:
- Age: Young children are more prone to ear infections due to the size and shape of their Eustachian tubes and their developing immune systems.
- Seasonal Variables: Ear infections are more common during the fall and winter months when colds and flu are prevalent.
- Environmental Factors: Exposure to tobacco smoke, high levels of air pollution, and frequent attendance at daycare centers can increase the risk of ear infections.
- Genetics: There is also a genetic component, as children with a family history of ear infections are more likely to experience them.
However, understanding these causes and risk factors can help individuals take proactive steps to reduce the likelihood of ear infections, such as practicing good hygiene, avoiding exposure to known irritants, and seeking timely medical advice when experiencing symptoms of an ear infection. By addressing the root causes and contributing factors, it’s possible to minimize the impact of ear infections on health and well-being.
Diagnosing Ear Infections
Early detection and diagnosis are crucial for effective treatment and preventing complications. This section provides an overview of how ear infections are diagnosed, emphasizing the significance of recognizing symptoms and undergoing appropriate diagnostic tests and procedures.
Recognizing Symptoms
Recognizing the symptoms of an ear infection is the first step toward diagnosis. Common signs include ear pain, difficulty hearing, fluid drainage from the ear, fever, and in children, increased irritability. Some individuals might also experience dizziness or a sense of fullness in the ear. Identifying these symptoms early can lead to a quicker diagnosis and treatment.
Diagnostic Tests and Procedures
Once symptoms suggest an ear infection, healthcare professionals employ several diagnostic tests and procedures to confirm the diagnosis:
- Otoscopic Examination: This is the most common test for diagnosing ear infections. A healthcare provider uses an otoscope, a handheld device with a light and magnifying lens, to examine the outer ear and eardrum. Inflammation, fluid behind the eardrum, or perforations in the eardrum can indicate an infection.
- Tympanometry: This procedure uses a device to measure the movement of the eardrum in response to changes in air pressure. It helps to detect fluid in the middle ear, a common sign of infection.
- Hearing Tests: In cases where ear infections are recurrent or persist, hearing tests may be conducted to assess any impact on hearing ability. These tests are particularly important for children, in whom hearing problems can affect language development and learning.
- Tympanocentesis: In severe or persistent cases, a specialist might perform tympanocentesis by inserting a needle through the eardrum to draw fluid from the middle ear. The fluid can then be tested for bacteria or viruses, helping to tailor the treatment plan.
- Laboratory Tests: Although not routinely performed for every case, laboratory tests on fluid samples can identify the specific pathogens causing the infection. This information can be invaluable in selecting the most effective antibiotics when needed.
If you suspect an ear infection, consult a healthcare provider to determine the best course of action based on a proper diagnosis.
Treatment Options for Ear Infections: Comprehensive Guide
Effective treatment is crucial to alleviate symptoms and prevent complications. This comprehensive guide explores the treatment options for ear infections, focusing on antibiotics, pain management, and home remedies. Additionally, we’ll delve into the decision-making process for choosing the right treatment, emphasizing the role of the severity of symptoms.
Antibiotics: A Targeted Approach
Antibiotics are often the first line of treatment for ear infections, especially when they are caused by bacteria. However, not all ear infections require antibiotics. For example, outer ear infections (otitis externa) and middle ear infections (otitis media) caused by bacteria can be effectively treated with antibiotics. In contrast, viral infections must run their course and do not respond to this treatment.
It’s essential to use antibiotics judiciously to avoid antibiotic resistance. Doctors usually decide to prescribe antibiotics based on the age of the patient, the severity of symptoms, and the duration of the infection. In some cases, they may adopt a wait-and-see approach, especially in children older than six months with mild symptoms, to see if the infection resolves on its own.
Pain Management: Easing Discomfort
Managing pain is a critical component of treating ear infections. Over-the-counter (OTC) pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil, Motrin) can be effective in reducing fever and alleviating pain. It’s important to follow the dosage instructions on the label and consult a healthcare professional, especially when treating children.
Warm compresses or a warm washcloth applied to the affected ear can also provide relief from pain. Ensuring rest and maintaining adequate hydration are beneficial strategies to support the body’s healing process.
Home Remedies: A Gentle Support
Alongside medical treatment, certain home remedies can offer comfort and potentially speed up the recovery process. These include:
- Staying hydrated: Drinking plenty of fluids can help thin the ear secretions, making them easier to drain.
- Elevating the head: Sleeping with the head slightly elevated can reduce ear pressure and alleviate pain.
- Warm oil drops: If there is no perforation or tubes in the eardrum, warm (not hot) oil drops (such as olive or garlic oil) can provide temporary pain relief. Always consult a healthcare professional before trying this remedy.
Making the Right Treatment Decision
The decision on how to treat an ear infection largely depends on the severity of symptoms and whether the infection is bacterial or viral. For mild cases, home remedies and pain management may suffice, while more severe or persistent infections may require antibiotics.
It’s essential to consult with a healthcare provider to get an accurate diagnosis and a tailored treatment plan. They will consider factors such as the patient’s age, medical history, and the specifics of the infection to recommend the most effective treatment approach.
Prevention and Management of Ear Infections
Understanding how to prevent and manage ear infections can significantly reduce discomfort, potential complications, and the need for medical treatments. Here’s a comprehensive guide to keeping ear infections at bay and effectively managing symptoms at home.
Prevention of Ear Infections
Preventing ear infections begins with adopting simple yet effective hygiene and health practices. By focusing on hygiene, vaccinations, and avoiding common risk factors, you can significantly lower the chances of developing an ear infection.
- Maintain Good Hygiene: Regular hand washing is the cornerstone of preventing ear infections. Encourage children to wash their hands frequently to avoid the spread of bacteria and viruses that can lead to infections. Additionally, keep the ears clean but avoid inserting objects that can push wax deeper into the ear canal.
- Stay Up to Date with Vaccinations: Vaccinations play a crucial role in preventing ear infections. The pneumococcal vaccine and the flu vaccine can reduce the risk of ear infections. Consult with your healthcare provider to ensure that your vaccinations and your child’s vaccinations are up to date.
- Avoid Common Risk Factors: Exposure to tobacco smoke and other pollutants can increase the risk of ear infections. Ensure a smoke-free environment for yourself and your children. If you are prone to allergies, managing them effectively can also help prevent ear infections, as allergies can lead to inflammation and fluid buildup in the Eustachian tubes.
- Breastfeed Infants: If possible, breastfeed infants for at least the first six months. Breastfeeding has been shown to provide antibodies that help fight off infections, including ear infections.
- Practice Proper Bottle-Feeding Techniques: When bottle-feeding, ensure the baby is in an upright position. Feeding in a lying down position can allow liquid to flow into the middle ear, potentially leading to infections.
Management of Symptoms at Home
While prevention is key, if an ear infection does occur, there are several ways to manage the symptoms at home while under treatment:
- Pain Management: Over-the-counter pain relievers such as acetaminophen (Tylenol) or ibuprofen (Advil) can be used to reduce pain and fever associated with ear infections. Always follow the recommended dosages and consider consulting a healthcare provider for children.
- Warm Compresses: Applying a warm compress to the affected ear for 15-20 minutes can help relieve pain and discomfort.
- Stay Hydrated: Drinking plenty of fluids can help thin the mucus, which may ease pressure in the middle ear.
- Elevate the Head: Elevating the head while sleeping can help drain the middle ear and reduce pressure, thereby alleviating pain.
- Avoid Water in the Ear: Keep the ear dry while an infection is present. Avoid swimming and carefully dry the ears after bathing or showering.
Remember, while these tips can help manage symptoms, they do not replace the advice of a healthcare professional. If symptoms persist or worsen, it’s important to consult with a doctor who may prescribe antibiotics or other treatments to effectively address the infection.
By integrating these preventative measures and management strategies into your daily routine, you can significantly reduce the risk of ear infections and ensure a quicker, more comfortable recovery should one occur.
FAQs: Understanding Ear Infections
What is an ear infection?
An ear infection is a condition that occurs when a bacterial or viral infection affects the middle ear, the section of your ear behind the eardrum. Ear infections can cause pain and discomfort due to inflammation and buildup of fluids in the middle ear.
Are there different types of ear infections?
Yes, there are mainly three types of ear infections: Acute Otitis Media (AOM), Otitis Media with Effusion (OME), and Otitis Externa (Swimmer’s Ear). AOM involves inflammation and infection in the middle ear, OME occurs when fluid remains in the middle ear after an infection has cleared, and Otitis Externa affects the outer ear canal.
What are the symptoms of an ear infection?
Symptoms can vary depending on the type of infection but commonly include ear pain, difficulty hearing, fluid drainage from the ear, fussiness in infants, and fever. If you experience these symptoms, it’s recommended to see a healthcare provider for a diagnosis and treatment.
What causes ear infections?
Ear infections are often caused by bacterial or viral infections. These can be the result of a cold, flu, or allergy that causes congestion and swelling of the nasal passages, throat, and eustachian tubes.
Who is at risk for ear infections?
While anyone can get an ear infection, children are more likely to develop them than adults. Risk factors include attending daycare, not being breastfed, seasonal factors (ear infections are more common during fall and winter), and exposure to tobacco smoke or high levels of air pollution.
How are ear infections diagnosed?
Healthcare providers diagnose ear infections by examining the ear with an instrument called an otoscope. This examination can reveal signs of fluid in the middle ear, a bulging or perforated eardrum, and the condition of the ear canal.
What are the treatments for ear infections?
Treatment may vary based on the type and severity of the infection. Mild infections might resolve without treatment, while others may require antibiotics. Pain relievers, such as acetaminophen or ibuprofen, can help relieve pain. In some cases, particularly in children with recurrent ear infections, surgical interventions like ear tubes might be recommended.
Can ear infections be prevented?
Preventive measures include practicing good hygiene, avoiding secondhand smoke, breastfeeding infants, and getting vaccinated against the flu and pneumococcal disease. Also, avoiding close contact with sick individuals and managing allergies can help reduce the risk of ear infections.
When should I see a doctor?
You should consult a healthcare provider if you or your child experiences symptoms of an ear infection, especially if symptoms are severe, don’t improve within a few days, or if the person with the infection is an infant. Prompt medical attention can prevent complications and ensure appropriate treatment.
Conclusion:
We strongly encourage anyone who suspects they or their loved ones are experiencing symptoms of an ear infection to consult with healthcare providers as soon as possible. Professional medical advice and treatment are paramount in managing the condition effectively and preventing further health complications. Seeking timely medical consultation not only ensures the well-being of the affected individual but also contributes to overall public health by mitigating the spread of infections.
In conclusion, the early recognition of ear infection symptoms plays a pivotal role in securing effective treatment and safeguarding health. We urge everyone to be vigilant in identifying potential signs of ear infections and to prioritize consulting healthcare professionals. Taking these steps can significantly impact the management of ear infections, leading to better health outcomes and comfort for those affected.
References
For those looking to expand their understanding of ear infections and seek further validation of the information provided here, the following reputable sources are invaluable. These references are selected based on their authority in the medical field, quality of information, and accessibility to readers seeking in-depth knowledge on ear infections.
- Centers for Disease Control and Prevention (CDC): The CDC’s page on ear infections offers comprehensive insights into types, causes, symptoms, and prevention strategies, making it an essential resource for both patients and healthcare providers. Visit CDC’s Ear Infection Page
- Mayo Clinic: Known for its patient-centered approach, the Mayo Clinic provides detailed articles on ear infection symptoms, diagnosis, treatments, and home remedies, written by medical experts. Explore Mayo Clinic’s Ear Infection Guide
- American Academy of Pediatrics (AAP): The AAP offers guidelines and research articles on the management of ear infections in children, a must-read for parents and pediatric healthcare professionals. Read AAP’s Recommendations
- MedlinePlus: A service of the U.S. National Library of Medicine, MedlinePlus provides trusted health information on ear infections, including an overview of treatment options and tips for care. Check Out MedlinePlus on Ear Infections
- WebMD: WebMD offers easily digestible information on ear infections, covering everything from symptoms and causes to treatment and prevention, geared towards a general audience. Learn More at WebMD
These resources are designed to be accessible and informative for readers seeking to deepen their understanding of ear infections, offering a blend of medical expertise and practical advice.