Dural Arteriovenous Fistulas Symptoms: Dural arteriovenous fistulas (DAVFs) are rare, complex vascular conditions affecting the dural venous sinuses, which are channels that drain blood from the brain.
DAVFs occur when an abnormal connection forms between an artery and a dural vein or sinus, leading to potential complications due to irregular blood flow.
This article delves into the symptoms and causes of DAVFs, providing essential information for recognizing and understanding this condition.
What are Dural Arteriovenous Fistulas?
Dural Arteriovenous Fistulas (DAVFs) are rare, abnormal connections between the arteries and veins in the dura mater, the tough outer layer of the meninges surrounding the brain and spinal cord. These connections bypass the capillary system, which is responsible for exchanging nutrients and waste between the blood and tissues. DAVFs can lead to a range of symptoms, from headaches and ringing in the ears to more severe effects like seizures or stroke, depending on their location and the amount of blood flow involved.
Unlike other vascular disorders that may affect the brain or spinal cord, DAVFs are specifically related to the blood vessels in the dura mater. This makes them unique in their presentation and potential impact on the body. They are classified based on the location of the fistula and the type of venous drainage, which influences their symptoms and how they are treated.
How DAVF Differs from Other Vascular Disorders
DAVFs are distinct from other vascular disorders due to their specific location in the dura mater and their mechanism of forming an abnormal connection between arteries and veins. This contrasts with conditions such as:
- Aneurysms, which are bulges in blood vessels caused by weakening of the vessel wall. Aneurysms can lead to bleeding if they rupture but do not involve abnormal connections between vessels.
- Arteriovenous Malformations (AVMs), which are also abnormal connections between arteries and veins but are typically located within the brain or spinal cord tissue itself, not in the dura mater. AVMs are often congenital, meaning they are present at birth.
- Stroke, which refers to the sudden death of brain cells due to lack of oxygen, typically caused by blockage or rupture of blood vessels in the brain, not by abnormal connections.
The key difference lies in the nature and location of the abnormal connection. DAVFs involve the dura mater and can have various venous drainage patterns, which can affect symptoms and treatment options. Understanding these differences is crucial for proper diagnosis and management of each condition, highlighting the importance of accurate imaging and specialist consultation in cases of suspected vascular disorders.
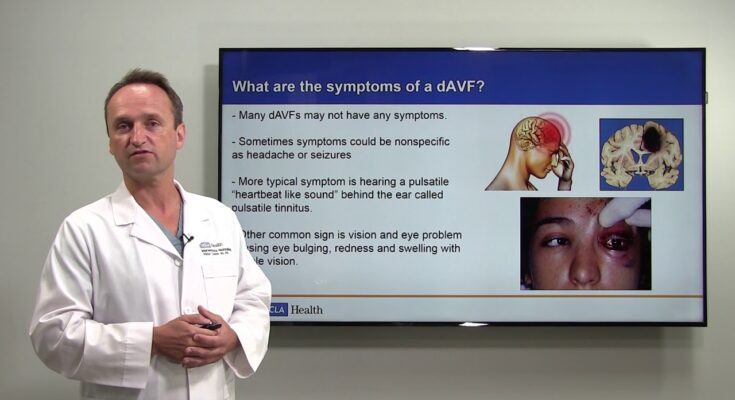
Symptoms of Dural Arteriovenous Fistulas
Understanding the symptoms of DAVFs is crucial for early detection and effective management. This section explores the common symptoms, their progression, and potential complications, supplemented by illustrative case studies and patient anecdotes.
List of Common Symptoms
The symptoms of DAVFs can vary significantly based on the location and severity of the fistula. Common symptoms include:
- Pulsatile Tinnitus: A constant, whooshing sound in one ear, synchronous with the patient’s heartbeat.
- Headaches: Persistent or severe headaches that do not respond well to typical headache remedies.
- Eye Symptoms: Redness, decreased vision, or a feeling of pressure in one or both eyes.
- Neurological Issues: Weakness, numbness, or other neurological deficits may occur, depending on the area of the brain affected.
- Seizures: In some cases, the increased pressure and altered blood flow can lead to seizures.
Progression of Symptoms and Potential Complications
If left untreated, DAVFs can lead to serious complications, including:
- Intracranial Hemorrhage: The increased pressure can cause blood vessels to rupture, leading to bleeding in the brain.
- Stroke: Reduced blood flow to parts of the brain can result in a stroke.
- Congestive Heart Failure: In severe cases, the extra burden on the heart to pump blood through the abnormal connections can lead to heart failure.
The progression of symptoms often correlates with the severity and location of the fistula. Early detection and treatment are pivotal in preventing these severe complications.
Case Studies or Patient Anecdotes
Case Study 1: A 45-year-old male presented with a 6-month history of pulsatile tinnitus in his right ear and frequent, unexplained headaches. After a detailed examination and imaging, he was diagnosed with a dural arteriovenous fistula. Treatment involved minimally invasive surgery to close off the abnormal connection, leading to the resolution of his symptoms.
Patient Anecdote: “Julia,” a 52-year-old woman, noticed a sudden onset of vision problems and a constant whooshing sound in her ears. Initially, she attributed these symptoms to stress and aging. However, after experiencing a seizure, she sought medical attention, which led to the diagnosis of a DAVF. Post-treatment, Julia’s symptoms improved significantly, highlighting the importance of seeking medical advice for persistent or unusual symptoms.
Meanwhile, awareness of these symptoms, combined with illustrative case studies, underscores the importance of early diagnosis and intervention. Patients experiencing any of the above symptoms should consult healthcare professionals promptly to ensure timely and effective treatment.
Causes of Dural Arteriovenous Fistulas
Understanding the causes and risk factors associated with DAVFs is crucial for both patients and healthcare providers. This section delves into the anatomy involved, the distinction between genetic and acquired causes, and identifies key risk factors such as age, gender, head injury, and a history of other vascular malformations.
The Anatomy Involved in DAVF
DAVFs involve the dura mater, one of the three layers of protective membranes surrounding the brain and spinal cord. Specifically, these fistulas occur when there is an abnormal connection between the dural arteries, which are meant to supply blood to the dura mater, and the dural veins, responsible for draining blood away. This abnormal bypass can lead to various neurological symptoms, depending on the location and severity of the fistula.
Genetic vs. Acquired Causes
The causes of DAVFs can be classified into genetic and acquired categories. While the exact cause of DAVFs is not always clear, some cases may be linked to genetic predispositions, suggesting that certain individuals may have an inherent vulnerability to developing these vascular anomalies. On the other hand, acquired causes refer to factors or events that occur during a person’s life, such as trauma or surgery, which might lead to the development of a DAVF.
Risk Factors
Age
Age is a significant risk factor for DAVFs, with most cases being diagnosed in adults. The risk increases with age, suggesting that the cumulative effects of aging and potential exposure to other risk factors over time may contribute to the development of DAVFs.
Gender
Research indicates a slight gender disparity in the incidence of DAVFs, with males being slightly more prone to developing these fistulas than females. However, the reasons behind this disparity are not fully understood and may involve a combination of genetic, hormonal, and environmental factors.
Head Injury
A history of head injury is another notable risk factor for the development of DAVFs. Traumatic events that cause damage to the blood vessels within the dura mater can potentially lead to the formation of a fistula. This underscores the importance of monitoring for vascular complications following significant head trauma.
History of Other Vascular Malformations
Individuals with a history of other vascular malformations are at an increased risk of developing DAVFs. This connection suggests that underlying vascular abnormalities may predispose some individuals to a broader spectrum of vascular issues, including DAVFs.
However, understanding the causes and risk factors of Dural Arteriovenous Fistulas is key to early diagnosis and effective management. By recognizing the signs and symptoms associated with DAVFs and seeking prompt medical attention, individuals can mitigate the potential complications associated with this condition.
Diagnosing Dural Arteriovenous Fistulas
Early detection and accurate diagnosis are crucial for preventing serious complications, including stroke and brain damage. In this guide, we delve into the common diagnostic tests and procedures for DAVFs, explore the challenges in diagnosing these conditions, and underscore the importance of early detection.
Common Diagnostic Tests and Procedures
- Magnetic Resonance Imaging (MRI): MRI scans are instrumental in providing detailed images of the brain’s and spinal cord’s structures. An MRI can help identify the presence of DAVFs and assess the extent of the impact on surrounding tissues.
- Computed Tomography (CT) Scan: CT scans offer a quicker way to visualize the brain and spinal cord. When combined with a contrast dye (CT angiography), they can reveal blood flow in arteries and veins, helping to detect DAVFs.
- Digital Subtraction Angiography (DSA): Considered the gold standard for diagnosing DAVFs, DSA provides a detailed view of blood vessels. This invasive procedure involves injecting a contrast dye into the bloodstream to highlight the vascular structures and abnormalities on X-ray images.
- Cerebral Angiogram: A more specific type of angiography, this procedure focuses on the blood vessels in the brain. It is particularly useful in mapping out the exact location and severity of DAVFs.
- Transcranial Doppler Ultrasound: This non-invasive test measures the blood flow velocity in the brain’s blood vessels, which can indicate the presence of DAVFs, although it’s less definitive than angiography.
Challenges in Diagnosing DAVF
Diagnosing DAVFs poses several challenges:
- Symptom Variability: Symptoms of DAVFs can range from very mild to severe and can mimic those of other neurological conditions, making it difficult to pinpoint DAVFs as the cause without comprehensive testing.
- Rare Condition: Due to their rarity, DAVFs are not always the first consideration when diagnosing vascular or neurological symptoms, potentially leading to delays in diagnosis.
- Technical Complexity: The intricate nature of the vascular system around the brain and spinal cord requires highly specialized imaging tests to diagnose DAVFs accurately, necessitating expertise and sometimes access to advanced medical facilities.
The Importance of Early Detection
Early detection of DAVFs is critical for several reasons:
- Preventing Complications: Untreated DAVFs can lead to serious complications, including bleeding in the brain (hemorrhage), stroke, and permanent neurological damage. Early diagnosis allows for timely intervention to mitigate these risks.
- Improving Outcomes: Early and accurate diagnosis enables more effective treatment planning, which can significantly improve the prognosis and quality of life for individuals with DAVFs.
- Reducing Symptom Severity: Early treatment can alleviate symptoms and prevent the progression of the condition, offering patients a better chance at maintaining their normal daily activities and overall well-being.
However, diagnosing DAVFs requires a combination of advanced imaging techniques and expert clinical assessment due to the complexity of the condition and the variability of symptoms. The challenges in diagnosing DAVFs highlight the need for heightened awareness and expertise among healthcare professionals. Early detection is paramount to preventing serious complications, improving patient outcomes, and ensuring the best possible quality of life for those affected by this condition.
Treatment Options for Dural Arteriovenous Fistulas
The treatment of DAVFs depends on various factors, including the location of the fistula, the presence of symptoms, and the risk of complications like bleeding. In this article, we’ll explore the treatment options available for DAVFs, highlighting the pros and cons of conservative management versus intervention, the types of surgical treatments, and recent advances in treatment.
Conservative Management vs. Intervention
For patients with DAVFs that present minimal symptoms and low risk of bleeding or neurological damage, conservative management may be considered. This approach typically involves regular monitoring of the condition through imaging studies to detect any changes in the fistula. However, for DAVFs with a higher risk of complications, active intervention is usually recommended to prevent stroke, brain damage, or other serious outcomes.
Surgical Treatments
Surgical treatments for DAVFs aim to disconnect the abnormal arteriovenous connection. There are two main surgical options:
- Endovascular Embolization: This minimally invasive procedure involves threading a catheter through the blood vessels to the site of the fistula and injecting materials to block the abnormal blood flow. Embolization can reduce the risk of bleeding and alleviate symptoms. It’s often the first line of treatment due to its lower risk compared to open surgery.
- Surgery: In some cases, particularly when embolization is not successful or feasible, open surgery may be necessary. The procedure involves exposing the dura mater and physically disconnecting or removing the fistula. Surgery offers a high chance of cure but comes with greater risks, such as infection and damage to nearby brain tissue.
Recent Advances in Treatment
The field of neurosurgery is constantly evolving, and recent advances have significantly improved the treatment outcomes for patients with DAVFs. Techniques in endovascular therapy have seen substantial enhancements, including the development of new embolic materials and improved imaging technology, allowing for more precise treatment with fewer complications. Additionally, the integration of stereotactic radiosurgery offers a non-invasive alternative for treating certain DAVFs, especially those that are difficult to access surgically.
While conservative management may be appropriate for some, others may require more aggressive intervention through embolization or surgery. With ongoing advancements in medical technology and surgical techniques, the prognosis for patients with DAVFs continues to improve, offering hope for better outcomes and quality of life.
Living with Dural Arteriovenous Fistulas
Living with dural arteriovenous fistulas (DAVFs) can be a challenging experience, requiring patients to make significant lifestyle adjustments and seek out appropriate support and resources. This comprehensive guide aims to provide valuable insights into managing life with DAVFs, focusing on lifestyle adjustments, management strategies, and available support resources to help patients navigate their condition effectively.
Lifestyle Adjustments and Management
When diagnosed with a dural arteriovenous fistula, making certain lifestyle adjustments can significantly impact your overall well-being and manage your symptoms more effectively. Here are key strategies to consider:
- Maintain a Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain optimal health and support your body’s healing process.
- Regular Exercise: While intense activities may need to be moderated, engaging in light to moderate exercise, as recommended by your healthcare provider, can improve cardiovascular health and overall fitness.
- Stress Management: Techniques such as meditation, yoga, or deep-breathing exercises can help reduce stress, which is particularly important as stress can exacerbate symptoms.
- Avoid Certain Activities: Depending on the severity and location of your DAVF, your doctor may advise against activities that increase cranial pressure, such as heavy lifting or straining.
- Medication Adherence: If medication has been prescribed to manage symptoms or reduce the risk of complications, it’s crucial to take it exactly as directed by your healthcare provider.
Support and Resources for Patients
Navigating life with a DAVF doesn’t have to be a solitary journey. A range of support and resources are available to assist you through this challenging time:
- Healthcare Team: Your primary care provider, neurologist, and other specialists are valuable sources of information and support. Don’t hesitate to reach out to them with questions or concerns.
- Support Groups: Connecting with others who are also living with DAVFs can provide emotional support, practical advice, and a sense of community. Look for online forums or local support groups in your area.
- Educational Materials: Reputable websites, pamphlets, and books can offer insights into your condition, treatment options, and strategies for managing symptoms.
- Counseling Services: Professional counselors or therapists specializing in chronic illness can help you cope with the emotional and psychological aspects of living with a DAVF.
By making informed lifestyle adjustments, adhering to treatment plans, and utilizing available support resources, patients can lead fulfilling lives despite their condition. Always consult with your healthcare provider before making any significant changes to your lifestyle or treatment plan to ensure they are safe and appropriate for your specific situation.
Prevention and Awareness of Dural Arteriovenous Fistulas
Preventing DAVFs might not always be possible due to their association with genetic predispositions and spontaneous occurrences, certain strategies can significantly reduce risks and enhance early detection through heightened awareness and education. This section delves into the preventive measures for DAVFs and underscores the crucial role of awareness and education in managing this condition effectively.
Strategies for Prevention
- Maintain Healthy Blood Pressure: High blood pressure can stress the walls of your blood vessels, increasing the risk of vascular problems like DAVFs. Managing your blood pressure through diet, exercise, and medication can reduce this risk.
- Avoid Smoking: Smoking is a significant risk factor for vascular diseases. Quitting smoking can improve your overall vascular health and reduce the risk of developing conditions like DAVFs.
- Head Injury Prevention: While not all DAVFs are preventable, minimizing the risk of head injuries can potentially reduce the likelihood of their development. This includes wearing appropriate safety gear during high-risk activities and ensuring homes are safe to prevent falls, especially in the elderly.
- Regular Check-ups: Regular medical check-ups can help identify potential health issues that could increase the risk of developing vascular conditions, including DAVFs. Early detection of related conditions can lead to better management and outcomes.
The Importance of Awareness and Education
Awareness and education about DAVFs are vital for several reasons:
- Early Detection: Understanding the symptoms of DAVFs, such as pulsatile tinnitus, headaches, or neurological deficits, can prompt earlier consultation with healthcare providers, leading to timely diagnosis and treatment.
- Reducing Stigma: Educating the public about DAVFs can reduce the stigma associated with this and other vascular conditions, encouraging individuals to seek help sooner.
- Empowering Patients: Knowledge about DAVFs empowers patients and their families to make informed decisions regarding their health care options, enhancing their ability to manage the condition effectively.
- Promoting Research and Support: Increased awareness can lead to more support for research into DAVFs, potentially leading to new treatments and better outcomes for patients.
However, while the prevention of DAVFs may not always be entirely within one’s control, adopting a healthy lifestyle and taking precautions against head injuries can mitigate some risk factors. Moreover, awareness and education play pivotal roles in ensuring early detection, reducing stigma, empowering patients, and fostering an environment conducive to advancing research and support for those affected by DAVFs.
FAQs on Dural Arteriovenous Fistulas Symptoms
What is a Dural Arteriovenous Fistula (DAVF)?
A Dural Arteriovenous Fistula (DAVF) is a rare vascular disorder where there is an abnormal connection between the arteries and veins in the dura mater, the protective covering of the brain. This condition can lead to significant neurological symptoms due to abnormal blood flow.
What are the common symptoms of DAVF?
Symptoms of DAVF can vary widely depending on the location and severity of the fistula. Common signs include pulsatile tinnitus (a ringing or buzzing in the ears), headache, dizziness, visual disturbances, and, in severe cases, neurological deficits or stroke-like symptoms.
Can DAVF cause seizures?
Yes, in some cases, DAVFs can lead to seizures. This is more likely when the fistula results in significant pressure or irritation to the surrounding brain tissue or leads to cerebral hemorrhage.
How does DAVF affect vision?
DAVFs located near the eye can affect vision by causing symptoms such as blurred vision, double vision, or even vision loss. This happens due to the increased pressure and congestion in the ocular vessels.
Is hearing loss a symptom of DAVF?
Hearing loss can occur with DAVFs, particularly when the abnormal vascular connection is close to the auditory nerves or structures involved in hearing. Pulsatile tinnitus is more common, but hearing loss can also occur as a consequence of altered blood flow.
Can DAVF symptoms worsen over time?
Yes, without treatment, the symptoms of DAVF can progressively worsen. The increased pressure and altered blood flow can lead to further damage to the brain and its surrounding structures, potentially leading to more severe neurological symptoms.
Are there any specific symptoms that indicate a high-risk DAVF?
Symptoms such as sudden onset of severe headache, neurological deficits (e.g., weakness, numbness, difficulty speaking), and signs of a stroke are indicative of a high-risk DAVF. These symptoms require immediate medical attention as they may signify brain hemorrhage or significant brain injury.
Conclusion
It is crucial to comprehend that DAVFs can stem from a variety of causes, including genetic predispositions, head injuries, or infections. This knowledge empowers individuals to assess their risk levels and monitor their health more vigilantly.
We strongly encourage anyone experiencing suspicious symptoms not to dismiss them lightly. Seeking medical advice promptly can make a significant difference in the outcomes of DAVF treatment. Early diagnosis and intervention are key to preventing complications and improving the quality of life for those affected by this condition.
In conclusion, the journey to understanding and managing Dural Arteriovenous Fistulas begins with awareness and education. By recognizing the symptoms and understanding the causes, individuals can take proactive steps toward safeguarding their neurological health. Remember, your health is in your hands, and seeking medical advice for any concerning symptoms is always a wise decision.