Dry Macular Degeneration Symptoms: Dry macular degeneration is a common eye condition marked by the gradual deterioration of the macula, a part of the retina responsible for clear vision directly in your line of sight.
Understanding the symptoms and causes of this condition is essential for early detection and management.
This comprehensive guide aims to provide valuable insights into dry macular degeneration, emphasizing its symptoms, causes, and the importance of early intervention.
Understanding Dry Macular Degeneration
Dry macular degeneration is a chronic eye condition that primarily affects older adults, leading to vision loss in the center of the visual field. This article aims to shed light on the prevalence, risk factors, and distinctions between dry and wet forms of macular degeneration, making the information accessible and informative for readers seeking to understand this eye condition.
Statistics on Prevalence and Risk Factors
Dry macular degeneration accounts for approximately 85% to 90% of cases of age-related macular degeneration (AMD), making it the most common form of the condition. The prevalence of AMD increases significantly with age, particularly affecting individuals over the age of 50. According to the American Macular Degeneration Foundation, it is estimated that millions of people worldwide suffer from some form of AMD, emphasizing the global impact of this condition.
Risk factors for developing dry macular degeneration include age, genetics, smoking, high blood pressure, obesity, and prolonged exposure to sunlight without adequate eye protection. Lifestyle choices, such as diet and exercise, also play a crucial role in managing and potentially reducing the risk of AMD. A diet rich in antioxidants and omega-3 fatty acids, alongside regular physical activity, can help mitigate some risk factors.
Distinction Between Dry and Wet Macular Degeneration
Understanding the difference between dry and wet macular degeneration is crucial for recognizing symptoms and seeking timely treatment. Dry macular degeneration is characterized by the presence of drusen—tiny yellow deposits beneath the retina. Over time, these deposits can cause the macula, the part of the retina responsible for sharp and central vision, to thin and deteriorate, leading to a gradual loss of vision.
In contrast, wet macular degeneration, which evolves from the dry form in about 10% of cases, involves the growth of abnormal blood vessels under the retina. These vessels can leak fluid and blood, causing rapid and severe vision loss. While wet AMD is less common, it accounts for a significant proportion of cases with severe vision loss.
The transition from dry to wet AMD underscores the importance of regular eye examinations for early detection and management of the condition. While there is no cure for dry macular degeneration, lifestyle adjustments and certain supplements may slow progression and preserve vision for a longer period.
However, understanding dry macular degeneration, its prevalence, risk factors, and how it differs from wet macular degeneration, is essential for early detection and management. Regular eye exams and adopting a healthy lifestyle can significantly impact the quality of life for those affected by this condition. By spreading awareness and information, we can support early detection and contribute to the overall management of macular degeneration.
Symptoms of Dry Macular Degeneration
Recognizing the early and advanced symptoms of dry macular degeneration is crucial for managing its progression and mitigating its impact. This article outlines the symptoms at different stages and discusses how they can gradually affect everyday activities.
Early Symptoms and Signs
Dry macular degeneration often begins subtly, without immediate impact on vision. Early detection is key, as it can lead to better management of the condition. Here are the early symptoms to watch out for:
- Slight Blurriness in Central Vision: Initially, you might notice a mild blurriness in your central vision when performing tasks that require seeing fine details, such as reading or sewing.
- Need for More Light: You may find yourself needing brighter light when doing close-up work.
- Difficulty Adapting to Low Light: Transitioning from bright to dimly lit environments becomes challenging, affecting activities like entering a dimly lit restaurant from the outdoors.
- Decreased Color Intensity: Colors might seem less vibrant than before, making it harder to distinguish between certain shades.
- Slight Distortion of Straight Lines: Straight lines, such as door frames and telephone poles, may appear slightly bent or wavy.
Advanced Symptoms
As dry macular degeneration progresses to more advanced stages, the symptoms become more pronounced and can significantly impact daily life:
- Increased Blurriness and Blind Spots: Central vision becomes increasingly blurry, and blind spots (scotomas) may develop, making it difficult to recognize faces, read, drive, or perform other activities that require sharp vision.
- Difficulty with Detailed Tasks: Tasks that require detailed vision, such as threading a needle or reading small print, become increasingly difficult, affecting one’s ability to perform everyday tasks independently.
- Need for High-Contrast and Magnification: There’s a greater reliance on high-contrast visuals and magnification devices to read, cook, or engage in hobbies.
The Gradual Progression and Its Impact on Daily Life
The progression from early to advanced symptoms of dry macular degeneration can be gradual, often taking place over several years. This slow advancement allows some individuals to adapt to changes in their vision; however, it can also make it challenging to recognize the need for timely medical consultation and intervention.
The impact on daily life can be profound. Activities that were once straightforward, like reading, driving, and even recognizing the faces of loved ones, become challenging. This can lead to a decrease in independence and quality of life, with significant emotional and psychological effects, including frustration, anxiety, and depression.
Early detection and management are essential to slow the progression of dry macular degeneration. Regular eye exams, lifestyle changes (such as diet and smoking cessation), and the use of low vision aids can help maintain independence and quality of life.
However, understanding the symptoms of dry macular degeneration and recognizing their progression is the first step toward managing this condition. By staying informed and proactive about eye health, individuals can better navigate the challenges posed by this condition and maintain their quality of life.
Causes and Risk Factors of Dry Macular Degeneration
Understanding the causes and risk factors associated with DMD is crucial for prevention and management. This article explores the various factors contributing to the development of DMD, including the aging process, genetics, lifestyle choices, and underlying health conditions.
The Aging Process and Its Effect on the Retina
Aging is the most significant risk factor for Dry Macular Degeneration. As individuals age, the tissues in the retina, specifically in the macula, thin and pigment deposits increase, leading to the condition. The macula is responsible for sharp, central vision required for activities like reading and driving. The natural aging process can cause the macula to deteriorate, affecting vision over time.
Genetic Factors Contributing to DMD
Research indicates that genetics play a substantial role in the likelihood of developing DMD. Certain genes have been identified that increase the risk of the condition. Individuals with a family history of Dry Macular Degeneration are at a higher risk, suggesting the importance of genetic factors in its development.
Lifestyle and Environmental Factors
Lifestyle choices and environmental factors can significantly impact the risk of developing Dry Macular Degeneration. Exposure to certain environmental factors, such as UV light, and personal habits like diet, exercise, and smoking, can influence the likelihood of DMD.
Smoking and Its Impact on Eye Health
Smoking is a major risk factor for Dry Macular Degeneration. It increases the risk of DMD significantly, as the harmful substances in cigarettes can affect the blood supply to the retina, accelerating the aging process of the eye and increasing the risk of vision loss.
Diet and Nutrition’s Role in Preventing DMD
A diet rich in antioxidants, vitamins, and minerals can help reduce the risk of developing Dry Macular Degeneration. Foods high in omega-3 fatty acids, lutein, zeaxanthin, vitamins C and E, and zinc have been shown to support eye health and may lower the risk of DMD. Adopting a diet that includes a variety of fruits, vegetables, and fish can contribute to the prevention of this condition.
The Significance of Sunlight Exposure and Eye Protection
Excessive exposure to sunlight, particularly UV rays, can damage the eyes and contribute to the development of Dry Macular Degeneration. Wearing sunglasses that block 100% of UV rays and a hat with a brim can protect the eyes from harmful sunlight, potentially reducing the risk of DMD.
Underlying Health Conditions That Increase Risk
Certain underlying health conditions, such as hypertension (high blood pressure), high cholesterol, obesity, and cardiovascular disease, can increase the risk of developing Dry Macular Degeneration. These conditions may affect the blood vessels in the eyes, leading to compromised eye health. Managing these health issues through lifestyle changes and medication can help reduce the risk of DMD.
However, Dry Macular Degeneration is influenced by a combination of aging, genetic, lifestyle, and health factors. Understanding these risk factors and adopting preventive measures can help individuals protect their eye health and potentially reduce the risk of developing DMD. Regular eye examinations are essential for early detection and management of the condition.
Diagnostic Approaches to Eye Health
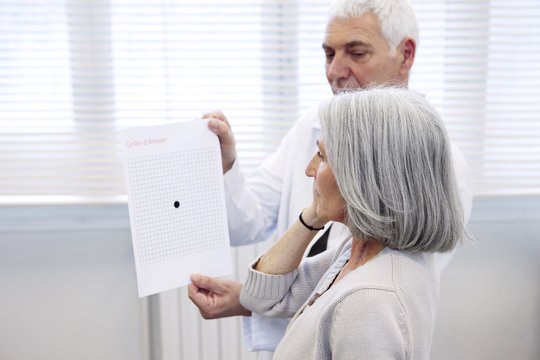
When it comes to maintaining optimal eye health, understanding the significance of diagnostic approaches is paramount. These strategies not only facilitate the early detection of potential eye conditions but also contribute significantly to preventing visual impairments. This article delves into the essential components of eye health diagnostics, including the pivotal role of routine eye exams, the utilization of advanced diagnostic tools, and the importance of discussing symptoms with an eye care professional.
Routine Eye Exams and Their Importance
Routine eye exams are the cornerstone of preventive eye care. These assessments serve not just to update eyeglass or contact lens prescriptions but also to detect early signs of eye diseases that could potentially lead to vision loss. It’s recommended that adults undergo a comprehensive eye exam every one to two years, depending on one’s age, risk factors, and whether they currently wear glasses or contacts. For children, eye exams at key developmental stages are crucial to ensure the proper vision development and to address any issues that could affect learning and daily activities.
Routine exams typically involve a series of tests to evaluate your vision and check for eye diseases. Some of these tests include a visual acuity test, which measures how clearly each eye is seeing, and a pressure test, which checks for glaucoma by measuring the pressure inside your eyes.
List of Advanced Diagnostic Tools and Tests
Advancements in technology have led to the development of sophisticated tools and tests that provide in-depth insights into eye health, allowing for early detection and management of diseases. Some of these advanced diagnostic tools include:
- Optical Coherence Tomography (OCT): This non-invasive imaging test uses light waves to take cross-section pictures of your retina, helping in the detection of conditions such as glaucoma, macular degeneration, and diabetic eye disease.
- Fundus Fluorescein Angiography: By injecting a special dye into your bloodstream, this test allows for the examination of blood flow in the retina and choroid, aiding in the diagnosis of retinal disorders.
- Corneal Topography: This test maps the surface curvature of the cornea, providing valuable information for the diagnosis and treatment of a variety of eye conditions, including astigmatism and corneal deformations.
- Visual Field Test: This test measures all areas of your eyesight, including your peripheral vision, and is used to detect blind spots which can originate from eye diseases such as glaucoma.
Discussing Symptoms with an Eye Care Professional
An open and honest dialogue with your eye care professional is critical. Discussing symptoms you’re experiencing, no matter how minor they may seem, can be the key to early detection of eye conditions. Symptoms such as changes in vision, eye pain, flashes of light, or sudden onset of floaters can indicate serious issues that require immediate attention.
Remember, early diagnosis and treatment are often critical for preventing vision loss. Therefore, being proactive about eye health, scheduling routine eye exams, and utilizing advanced diagnostic tools when necessary, are essential steps in maintaining good eye health.
However, leveraging diagnostic approaches in eye care not only aids in the early detection and treatment of eye diseases but also plays a significant role in preserving vision. By understanding the importance of routine eye exams, familiarizing oneself with advanced diagnostic tools, and communicating effectively with eye care professionals, individuals can significantly contribute to their overall eye health and wellbeing.
Managing Symptoms and Slowing Progression
Taking care of your eyes is crucial for maintaining vision and overall health. Whether you’re dealing with a specific eye condition or aiming to prevent future issues, there are several strategies to manage symptoms and slow progression. This guide will explore lifestyle modifications, nutritional supplements, adaptive devices, and the importance of regular monitoring and medical check-ups.
Lifestyle Modifications for Better Eye Health
1. Protect Your Eyes from UV Light: Wearing sunglasses that block 100% of UV rays can protect your eyes from harmful sunlight, reducing the risk of conditions like cataracts and macular degeneration.
2. Quit Smoking: Smoking increases the risk of eye diseases, including cataracts and age-related macular degeneration. Quitting can significantly reduce these risks.
3. Limit Screen Time: Reducing exposure to screens can prevent eye strain and dry eyes. Take regular breaks using the 20-20-20 rule: every 20 minutes, look at something 20 feet away for at least 20 seconds.
4. Maintain a Healthy Weight: Being overweight increases the risk of diabetes and other health conditions that can lead to vision loss.
Nutritional Supplements and Their Effectiveness
Nutritional supplements can play a role in eye health. Here are some key nutrients:
1. Omega-3 Fatty Acids: Found in fish oil, they can help relieve dry eye symptoms.
2. Lutein and Zeaxanthin: These antioxidants, found in leafy greens and other vegetables, may reduce the risk of chronic eye diseases.
3. Vitamin C and E: These vitamins can protect your eyes against damaging free radicals and support healthy tissues.
It’s important to consult with a healthcare provider before starting any supplement regimen, as they can advise on the right types and amounts for your specific needs.
Adaptive Devices and Aids for Low Vision
For those with low vision, adaptive devices can significantly improve quality of life:
1. Magnifying Glasses: For reading and close tasks.
2. Large Print Materials: Easier to read than standard texts.
3. Talking Devices: Such as watches and books, offer auditory assistance.
4. High-Contrast and Large-Button Devices: Improve ease of use for phones and keyboards.
Exploring these options with a specialist can help identify the best tools for individual needs.
Regular Monitoring and Medical Check-Ups
Regular eye exams are vital for early detection and management of eye conditions. Adults should have a comprehensive eye exam at least once every two years, or more frequently if recommended by an eye care professional. These check-ups can catch conditions like glaucoma and diabetic retinopathy in their early stages when they’re most treatable.
By integrating these practices into your lifestyle, you can take proactive steps toward maintaining your eye health and slowing the progression of any existing conditions. Remember, the best approach combines preventive care with professional guidance to ensure the best outcomes for your vision and overall well-being.
FAQs on Dry Macular Degeneration
What is dry macular degeneration?
Dry macular degeneration is a chronic eye disease that affects the macula — the part of the retina responsible for clear vision in your direct line of sight. This condition leads to a gradual loss of central vision, primarily affecting reading, driving, and recognizing faces. It’s termed “dry” because it does not involve leaking blood vessels, distinguishing it from the “wet” form of macular degeneration.
What causes dry macular degeneration?
The exact cause of dry macular degeneration is unknown. However, the condition is primarily associated with aging and the thinning of macular tissues. Genetic factors, smoking, and exposure to sunlight can also increase the risk.
What are the symptoms of dry macular degeneration?
Symptoms usually develop gradually and without pain. They include blurred or reduced central vision in one or both eyes, the need for brighter light when reading or doing close work, increased difficulty adapting to low light levels, and the appearance of drusen (yellow deposits beneath the retina).
How is dry macular degeneration diagnosed?
An eye specialist (ophthalmologist) can diagnose dry macular degeneration through a comprehensive eye exam. Tests may include a visual acuity test, a dilated eye exam to examine the retina and macula, and imaging tests like optical coherence tomography (OCT) to capture detailed images of the eye structure.
Can dry macular degeneration be treated?
There is no cure for dry macular degeneration, but certain measures can help slow its progression. These include taking specific vitamins and minerals, adapting lifestyle changes such as quitting smoking, maintaining a healthy diet rich in leafy greens and fish, and protecting eyes from ultraviolet light.
How can I reduce my risk of developing dry macular degeneration?
While you cannot completely prevent dry macular degeneration, you can reduce your risk by not smoking, eating a diet high in antioxidants, maintaining normal blood pressure and cholesterol levels, and protecting your eyes from UV rays by wearing sunglasses outdoors.
Is dry macular degeneration the same as wet macular degeneration?
No, dry macular degeneration and wet macular degeneration are different. The dry form is more common and less severe, characterized by the thinning of the macula and drusen. The wet form, though less common, is more severe and involves the growth of abnormal blood vessels under the macula, leading to more significant vision loss.
How often should I have my eyes examined if I have dry macular degeneration?
If you have dry macular degeneration, it’s crucial to have regular eye exams. The frequency of these exams will depend on the severity of your condition and your doctor’s recommendations. Typically, an annual eye exam is advised, but more frequent visits may be necessary if your condition is progressing.
Conclusion
In wrapping up our discussion on dry macular degeneration, it’s paramount to underscore the significance of early symptom recognition. This condition, marked by the gradual decline in the central field of vision, can profoundly affect daily activities and quality of life. Early detection plays a crucial role in slowing the progression of the disease and preserving vision as long as possible.
Identifying the symptoms early on—such as blurred vision, the need for brighter light when reading or doing close tasks, increased difficulty adapting to low light levels, increased blurriness of printed words, a decrease in the intensity or brightness of colors, and difficulty recognizing faces—can be a signal to seek professional help. It’s vital to listen to your body and note any changes in your vision, however minor they may seem.
We strongly encourage anyone experiencing these signs or changes in their vision to seek professional advice. A healthcare provider can offer a comprehensive diagnosis and recommend a management plan tailored to your specific needs. Early intervention is key to managing dry macular degeneration effectively and can help maintain your vision and quality of life.
Remember, while the prospect of facing a condition like dry macular degeneration can be daunting, you are not alone. With the right support and early management strategies, many individuals continue to lead fulfilling lives. Don’t hesitate to reach out to healthcare professionals—they are your best resource for diagnosis, information, and support. Your vision is invaluable, and taking proactive steps towards its care is a wise and necessary investment in your overall well-being.