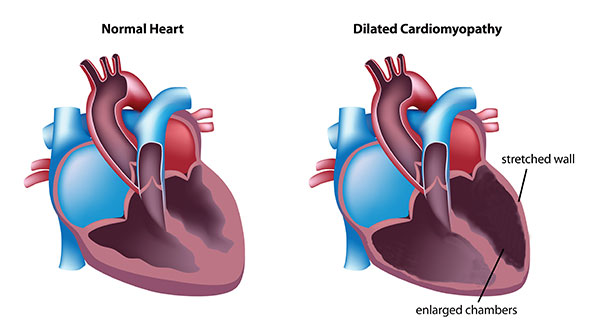
Dilated Cardiomyopathy Treatment: Dilated Cardiomyopathy (DCM) is a condition characterized by the enlargement and weakening of the heart’s left ventricle, the main pumping chamber.
This enlargement impedes the heart’s ability to pump blood efficiently, leading to a cascade of symptoms and complications that can severely impact a person’s quality of life.
Understanding Dilated Cardiomyopathy
Dilated Cardiomyopathy (DCM) is a condition that affects the heart’s ability to pump blood efficiently. In this state, the heart’s main pumping chamber, the left ventricle, becomes enlarged (dilated) and its pumping ability is weakened. This enlargement can affect the heart’s structure and function, leading to a range of symptoms including shortness of breath, fatigue, and swelling of the legs and feet. Understanding DCM involves exploring its causes, risk factors, and the demographics it affects.
Causes and Risk Factors Associated with DCM
The causes of Dilated Cardiomyopathy can be diverse and sometimes remain unidentified. However, several factors have been linked to the development of this condition:
- Genetic predisposition: DCM can be inherited, indicating a genetic component to the disease.
- Viral infections: Some viral infections can lead to heart muscle inflammation, contributing to DCM.
- Alcohol abuse: Chronic abuse of alcohol can weaken the heart muscle.
- Toxins and medications: Exposure to certain toxins and the use of specific medications can adversely affect heart function.
- Underlying conditions: Conditions like diabetes, thyroid disorders, and autoimmune diseases can increase the risk of developing DCM.
Understanding these risk factors is crucial for both preventing the onset of DCM and managing the condition effectively if diagnosed.
Statistics on Prevalence and Demographics Affected
Dilated Cardiomyopathy is not restricted to any specific demographic and can affect individuals of any age, race, or gender. However, statistics have shown certain patterns in its prevalence and impact:
- Age and gender: DCM is more commonly diagnosed in middle-aged individuals, with a slight male predominance.
- Global prevalence: The condition affects people worldwide, with variations in prevalence rates across different regions and populations.
- Impact on quality of life: The severity of DCM and its impact on an individual’s quality of life can vary greatly. Some people live a normal life with minimal symptoms, while others may experience significant health deterioration.
However, understanding the scope and impact of Dilated Cardiomyopathy is essential for healthcare professionals and patients alike. Awareness of the causes, risk factors, and demographics affected by DCM can lead to early diagnosis and improved management of the condition, ultimately enhancing the quality of life for those affected.
Symptoms and Early Detection of Dilated Cardiomyopathy
Recognizing the early signs of dilated cardiomyopathy (DCM) and understanding the importance of early detection can be crucial in managing the condition effectively. DCM is characterized by the dilation and weakening of the heart’s main pumping chamber, the left ventricle, which leads to decreased heart function and can affect individuals of any age.
Common Symptoms Associated with Dilated Cardiomyopathy
The symptoms of DCM might not be noticeable in the early stages, but as the condition progresses, they become more apparent. Common symptoms include:
- Fatigue and weakness, making daily activities more challenging.
- Shortness of breath (dyspnea), especially during exertion or even at rest, as a result of fluid buildup in the lungs.
- Swelling (edema) in the legs, ankles, and feet due to fluid retention.
- Irregular heartbeats (arrhythmias) that feel rapid, pounding, or fluttering.
- Dizziness, lightheadedness, and fainting spells due to reduced blood flow to the brain.
- Chest pain or discomfort, which may occur if the heart muscle is not receiving enough oxygen.
The Role of Early Detection in Managing DCM
Early detection of DCM is paramount for several reasons. It allows for the initiation of treatment to slow the progression of the disease, manage symptoms, and minimize complications such as heart failure or sudden cardiac arrest. Early intervention can also provide patients with a better quality of life and potentially prolong life expectancy. Lifestyle modifications, medications, and in some cases, devices like pacemakers or defibrillators, are more effective when implemented early in the disease course.
Diagnostic Tests and Screenings for Dilated Cardiomyopathy
To diagnose DCM, healthcare providers use a combination of medical history evaluation, physical examinations, and specific diagnostic tests:
- Echocardiogram: This is the primary diagnostic tool for DCM. It uses sound waves to produce images of the heart, allowing doctors to see the heart beating and pumping blood, and to measure the dilation and function of the ventricles.
- Electrocardiogram (ECG or EKG): Measures the electrical activity of the heart and can identify arrhythmias, signs of heart damage, and other abnormalities.
- MRI (Magnetic Resonance Imaging) of the heart: Provides detailed images of the heart’s structure and function, helping in the assessment of the degree of dilation and the presence of scar tissue.
- Blood tests: Can check for markers of other diseases that affect the heart and the effectiveness of the heart’s pumping action.
- Cardiac catheterization: Although less commonly used for DCM diagnosis, it can help determine if coronary artery disease is contributing to the heart’s dysfunction.
If you or someone you know is experiencing any of the symptoms mentioned, consulting with a healthcare provider for a thorough evaluation is highly recommended. Early detection and treatment can significantly impact the management of the condition and the overall well-being of those affected.
Dilated Cardiomyopathy Diagnosis
Diagnosing Dilated Cardiomyopathy (DCM) is a critical step in managing and treating the condition effectively. The process employs a variety of diagnostic methods, each playing a pivotal role in understanding the extent and impact of the disease on the heart’s structure and functionality. Here’s a closer look at these diagnostic tools and their significance.
Echocardiograms
An echocardiogram is often the cornerstone of DCM diagnosis. This non-invasive ultrasound test provides a detailed image of the heart, allowing doctors to assess the size of the heart chambers, the functioning of the heart valves, and the overall pumping efficiency of the heart. It’s crucial for detecting the dilation and weakened pumping action characteristic of DCM.
Magnetic Resonance Imaging (MRI)
Cardiac MRI offers a more detailed view of the heart’s structure and function than an echocardiogram. It’s particularly useful in assessing the extent of damage to the heart muscle and in distinguishing DCM from other conditions that could cause similar symptoms, such as myocarditis or cardiac sarcoidosis.
Electrocardiogram (ECG)
An ECG records the electrical activity of the heart and can detect irregular heart rhythms (arrhythmias), which are common in patients with DCM. It can also reveal signs of heart strain or enlargement, further supporting a diagnosis of DCM.
Blood Tests
While blood tests cannot diagnose DCM directly, they can rule out other causes of heart failure and check for conditions that may contribute to DCM, such as thyroid disease or infections. Certain biomarkers in the blood can also help assess the severity of heart failure.
The Importance of a Comprehensive Diagnosis
A thorough diagnostic evaluation is essential not only for confirming the presence of DCM but also for planning the most effective treatment strategy. Understanding the specific characteristics of the heart’s function and structure helps tailor treatment to the individual’s needs, potentially improving outcomes.
Staging and Prognosis
The diagnostic process also aids in staging the disease, which is pivotal for prognostication. Identifying the stage of DCM helps predict the likely course of the disease, including the risk of complications such as arrhythmias or heart failure. This information is invaluable for both patients and healthcare providers in managing the condition and making informed decisions about treatment and lifestyle adjustments.
However, the diagnosis of dilated cardiomyopathy involves a combination of advanced imaging techniques, electrical activity mapping, and blood analysis. This comprehensive approach not only confirms the diagnosis but also provides detailed insights into the severity and implications of the condition, guiding treatment decisions and helping to establish a prognosis.
Treatment Options for Dilated Cardiomyopathy
Dilated Cardiomyopathy (DCM) is a condition that affects the heart’s ability to pump blood effectively due to an enlarged and weakened heart muscle. Treatment for DCM is aimed at improving the heart’s function, relieving symptoms, and preventing further complications. Here is an overview of the treatment options available for DCM:
Medications
Medications play a crucial role in managing DCM by addressing various aspects of the condition:
- ACE inhibitors and angiotensin II receptor blockers (ARBs) help relax blood vessels, reducing the workload on the heart.
- Beta-blockers slow the heart rate and reduce blood pressure, further easing the heart’s workload.
- Diuretics help remove excess fluid from the body, relieving symptoms like swelling and shortness of breath.
- Digoxin can improve heart pumping function and control heart rate.
- Anticoagulants may be prescribed to prevent blood clots, a risk for many with DCM.
Non-pharmacological Treatments
Lifestyle changes and management strategies are essential for anyone diagnosed with DCM:
- Regular, moderate exercise can strengthen the heart and improve cardiovascular health, but should be discussed with a healthcare provider.
- Dietary changes, including reducing salt intake to help manage fluid retention.
- Avoiding alcohol and smoking, as these can worsen heart health.
- Monitoring and managing blood pressure and diabetes effectively to avoid further heart damage.
Surgical and Medical Procedures
For some, medications and lifestyle changes may not be enough, and more invasive treatments may be necessary:
- Pacemakers and Implantable Cardioverter Defibrillators (ICDs) can help manage irregular heartbeats and prevent sudden cardiac death.
- Cardiac resynchronization therapy (CRT) can help the heart’s chambers beat in more synchronized manner.
- In severe cases, a ventricular assist device (VAD) or a heart transplant might be considered when the heart’s function is critically reduced.
Emerging Treatments and Research Directions
Research into DCM is ongoing, with new treatments and interventions being explored. This includes genetic therapies for those with inherited forms of DCM, advanced stem cell therapies aimed at repairing damaged heart tissue, and novel medications designed to target the underlying molecular mechanisms of the disease.
While the treatment landscape for DCM is broad and varied, the best approach depends on the individual’s specific condition, symptoms, and overall health. Regular follow-ups with a healthcare provider are essential to monitor the condition and adjust treatment as needed.
Managing Dilated Cardiomyopathy
Managing Dilated Cardiomyopathy (DCM) involves a comprehensive approach that includes lifestyle adjustments, regular monitoring, and support mechanisms for both the patient and their family. Understanding and implementing these strategies can significantly improve the quality of life for individuals diagnosed with DCM and can help in managing the symptoms more effectively.
Lifestyle Adjustments and Home Care
For patients living with DCM, making certain lifestyle changes is crucial. These include:
- Dietary Changes: Adopting a heart-healthy diet that is low in sodium, saturated fats, and trans fats can help manage symptoms. It’s also important to maintain a healthy weight to reduce the strain on the heart.
- Exercise: While strenuous activity may be restricted, many patients with DCM can benefit from a tailored exercise program designed by a healthcare professional. This can help improve heart function over time.
- Limiting Alcohol and Tobacco Use: Alcohol and tobacco can exacerbate heart conditions, so limiting consumption or abstaining altogether is beneficial.
- Medication Adherence: Patients are often prescribed medications to manage DCM, and it’s essential to take them as directed by a healthcare provider.
Regular Follow-up and Monitoring
Regular check-ups with a healthcare provider are vital for monitoring the progression of DCM. During these visits, the healthcare team may perform tests to assess heart function and determine the effectiveness of the treatment plan. Adjustments to medications or lifestyle recommendations may be made based on these findings. Staying proactive in healthcare appointments allows for timely interventions, which can significantly impact the management of DCM.
Coping Strategies and Support
Living with DCM can be challenging not just for the patient but also for their family. Here are some ways to navigate these challenges:
- Education: Understanding the condition can empower patients and families to make informed decisions about care and lifestyle adjustments.
- Support Groups: Joining a support group can provide emotional support and practical advice from others who are going through similar experiences.
- Mental Health: Managing a chronic illness can be mentally taxing. Seeking support from a mental health professional can help address feelings of anxiety or depression that may arise.
- Family and Social Support: Having a strong support system can provide practical help and emotional sustenance. It’s important for families to communicate openly about the challenges and work together to find solutions.
Implementing these management strategies for DCM requires patience and persistence. By adopting a holistic approach that encompasses lifestyle modifications, regular medical care, and emotional support, patients and their families can navigate the challenges of DCM more effectively. Remember, each individual’s experience with DCM is unique, and it’s crucial to work closely with healthcare providers to tailor management strategies to the patient’s specific needs.
FAQs on Dilated Cardiomyopathy Diagnosis and Treatment
What is dilated cardiomyopathy?
Dilated cardiomyopathy (DCM) is a condition where the heart’s ability to pump blood is decreased because the heart’s main pumping chamber, the left ventricle, is enlarged and weakened. This can affect not only the heart but also the overall health and functioning of other organs due to reduced blood flow.
How is dilated cardiomyopathy diagnosed?
Diagnosing DCM typically involves a combination of patient history, physical examination, and various tests. Common diagnostic tools include echocardiograms (to visualize the heart’s structure and function), electrocardiograms (to monitor heart rhythm), MRI scans (to provide detailed images of the heart’s structure), and blood tests (to identify markers of heart failure or other related conditions). In some cases, a cardiac biopsy may be performed to determine the underlying cause of the cardiomyopathy.
What treatment options are available for dilated cardiomyopathy?
Treatment for DCM aims to improve symptoms, slow the progression of the disease, and prevent complications. Options include lifestyle changes (such as diet and exercise modifications), medications (like ACE inhibitors, beta-blockers, and diuretics to manage blood pressure and reduce heart strain), and in more severe cases, medical devices (like pacemakers or defibrillators to manage heart rhythm). In advanced stages, heart transplantation may be considered.
Can lifestyle changes really make a difference in managing DCM?
Yes, lifestyle changes play a crucial role in managing DCM. Adopting a heart-healthy diet, engaging in regular, moderate exercise (as recommended by a healthcare provider), avoiding alcohol and tobacco, and managing stress can all contribute to better heart health and improved quality of life for individuals with DCM.
Is dilated cardiomyopathy hereditary?
In some cases, DCM is hereditary, meaning it can be passed down from parents to children through genes. Genetic testing may be recommended for family members of individuals diagnosed with DCM to identify those at risk and potentially guide early intervention and management strategies.
How does the prognosis of dilated cardiomyopathy vary?
The prognosis of DCM can vary widely among individuals depending on various factors, including the cause of the cardiomyopathy, the severity of symptoms at the time of diagnosis, how well the condition responds to treatment, and the presence of any complications. While some individuals may experience a stable condition with treatment, others may see a progressive decline in heart function. Regular follow-up with a healthcare provider is essential to monitor the condition and adjust treatment as needed.
Conclusion
In conclusion, our exploration of dilated cardiomyopathy (DCM) has underscored the complexity of this heart condition and the paramount importance of personalized treatment plans.
By understanding the key points covered, including the causes, symptoms, diagnosis, and treatment options for DCM, we gain a comprehensive view of this challenging disease.
The significance of tailoring treatment plans to individual patients cannot be overstated, as it ensures that each person receives the most effective care based on their unique health profile and disease progression.