Diabetes Treatment: Diabetes is a chronic condition that affects millions worldwide, characterized by elevated levels of glucose in the blood. It is crucial to diagnose and treat this condition early to prevent complications.
This comprehensive guide delves into the diagnosis and treatment of diabetes, offering valuable insights for those affected by or at risk of this condition.
Understanding Diabetes
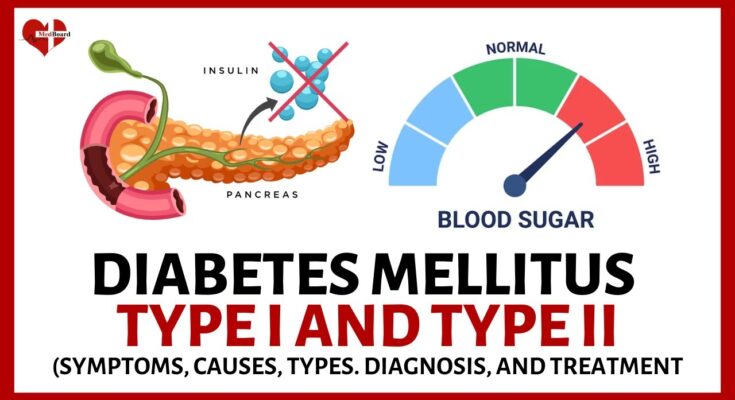
Diabetes is a chronic health condition that affects millions of people worldwide. It occurs when the body either cannot produce enough insulin or cannot effectively use the insulin it produces. Insulin is a hormone crucial for regulating blood sugar levels, and its proper functioning is essential for maintaining good health. In this section, we’ll delve into the different types of diabetes, common symptoms, risk factors, and the role of insulin in blood sugar regulation.
Types of Diabetes
There are mainly three types of diabetes: Type 1, Type 2, and Gestational Diabetes.
- Type 1 Diabetes is an autoimmune condition where the body’s immune system attacks and destroys the insulin-producing cells in the pancreas. This type often appears in childhood or adolescence but can develop at any age.
- Type 2 Diabetes is more common and usually develops in adults over the age of 45 years, but it’s increasingly occurring in younger age groups including children, adolescents, and young adults. This type is often associated with obesity and lifestyle factors.
- Gestational Diabetes occurs during pregnancy and usually disappears after giving birth. However, it increases the risk of developing Type 2 diabetes later in life.
Common Symptoms of Diabetes
The symptoms of diabetes can be subtle at first but become more noticeable over time. Common symptoms include:
- Increased thirst and hunger
- Frequent urination
- Unexplained weight loss (more common in Type 1)
- Fatigue
- Blurred vision
- Slow healing of cuts and wounds
- Tingling, pain, or numbness in the hands or feet (Type 2)
Risk Factors
Several factors can increase the risk of developing diabetes, including:
- Family history of diabetes
- Overweight or obesity
- Physical inactivity
- Age (older age increases risk)
- High blood pressure
- Abnormal cholesterol levels
- History of gestational diabetes or giving birth to a baby weighing more than 9 pounds
The Role of Insulin in Blood Sugar Regulation
Insulin plays a vital role in blood sugar regulation. When we eat, our body breaks down carbohydrates into glucose, which enters the bloodstream. In response, the pancreas releases insulin, which acts as a key to allow glucose to enter the body’s cells to be used for energy. In people with diabetes, this process is disrupted, leading to elevated blood sugar levels. Over time, high blood sugar levels can lead to serious health complications, including heart disease, kidney damage, and vision loss.
Understanding diabetes is the first step toward managing it effectively. By recognizing the types, symptoms, and risk factors associated with this condition, individuals can take proactive steps to monitor their health and seek appropriate treatment. Moreover, understanding the crucial role of insulin in regulating blood sugar levels highlights the importance of maintaining a healthy lifestyle to support the body’s insulin function and manage or prevent diabetes.
However, diabetes is a significant health challenge that requires awareness, education, and proactive management. Whether you are at risk for diabetes or already living with the condition, understanding these key aspects can help you navigate the path to better health.
Diagnosis of Diabetes: A Comprehensive Guide
Early detection and treatment of diabetes can significantly reduce the risk of developing serious complications such as heart disease, stroke, kidney failure, and blindness. This article aims to guide you through the various screening and diagnostic tests available for diabetes, explaining their importance and how to interpret their results.
Importance of Timely Diagnosis in Diabetes Management
Diagnosing diabetes early is crucial for effective management and prevention of complications. Early diagnosis allows for prompt initiation of treatment, lifestyle adjustments, and monitoring, which can greatly improve quality of life and reduce the risk of long-term complications. It’s essential to recognize the symptoms of diabetes and seek medical advice promptly.
Screening and Diagnostic Tests for Diabetes
Several tests are used to diagnose diabetes and prediabetes. These tests measure blood glucose levels and provide valuable information about how your body is managing blood sugar. The primary tests include:
- Fasting Plasma Glucose (FPG) Test
- Oral Glucose Tolerance Test (OGTT)
- Hemoglobin A1c Test
Fasting Plasma Glucose (FPG) Test
The FPG test measures your blood sugar levels after an overnight fast (not eating for at least 8 hours). It’s a simple, fast, and cost-effective test. A result of 126 mg/dL (7.0 mmol/L) or higher on two separate tests indicates diabetes.
Oral Glucose Tolerance Test (OGTT)
The OGTT is more sensitive than the FPG test for diagnosing prediabetes and gestational diabetes. It involves fasting overnight, having your blood sugar measured, drinking a sugary liquid, and then having your blood sugar checked several times over the next two to three hours. A blood sugar level of 200 mg/dL (11.1 mmol/L) or higher after two hours suggests diabetes.
Hemoglobin A1c Test
The A1c test provides a snapshot of your average blood sugar levels over the past three months. It measures the percentage of blood sugar attached to hemoglobin, the oxygen-carrying protein in red blood cells. An A1c level of 6.5% or higher on two separate tests indicates diabetes.
Interpreting Test Results and What They Mean for You
Understanding your test results is crucial for managing your health. Here’s what the results mean:
- Normal: An FPG result below 100 mg/dL, an OGTT less than 140 mg/dL after two hours, and an A1c below 5.7%.
- Prediabetes: An FPG result from 100 to 125 mg/dL, an OGTT from 140 to 199 mg/dL after two hours, and an A1c from 5.7% to 6.4%.
- Diabetes: An FPG result of 126 mg/dL or higher, an OGTT of 200 mg/dL or higher after two hours, and an A1c of 6.5% or higher.
If your results indicate diabetes or prediabetes, your healthcare provider will discuss the next steps, including lifestyle changes, medication, and monitoring your blood sugar levels. Early intervention can make a significant difference in managing diabetes and maintaining a healthy, active life.
However, timely diagnosis and understanding your diabetes screening and diagnostic test results are pivotal for effective diabetes management. If you suspect you have symptoms of diabetes or are at risk, consult your healthcare provider to discuss the best screening options for you. Early detection and management are your best strategies for living well with diabetes.
Treatment Options for Diabetes
Diabetes management is a multifaceted approach that necessitates a combination of lifestyle modifications and medication management. Tailoring a treatment plan to individual needs is crucial for effective diabetes control. This section delves into the importance of lifestyle changes, medication management, and the critical role of medication adherence in managing diabetes.
Lifestyle Modifications for Managing Diabetes
Lifestyle changes play a pivotal role in managing diabetes and can significantly impact blood sugar levels, overall health, and quality of life. Key lifestyle modifications include:
- Healthy Eating: Embrace a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Minimize processed foods and sugars to maintain stable blood sugar levels.
- Regular Exercise: Aim for at least 150 minutes of moderate aerobic activity per week, such as walking, swimming, or cycling. Exercise helps in controlling blood glucose levels, losing weight, and reducing cardiovascular risks.
- Weight Management: Achieving and maintaining a healthy weight is essential for managing diabetes. Even a modest weight loss can improve blood sugar control.
- Smoking Cessation: Smoking increases the risk of diabetes complications, including heart disease, stroke, and nerve damage. Quitting smoking can significantly reduce these risks.
- Stress Management: Stress can affect blood sugar levels. Techniques such as meditation, yoga, or deep-breathing exercises can help manage stress effectively.
Medication Management
For many people with diabetes, lifestyle changes alone are not enough to control blood sugar levels. Medication management becomes essential and can include:
- Oral Medications: Various oral medications can help manage blood sugar levels by increasing insulin production, decreasing sugar absorption, or improving insulin sensitivity.
- Insulin Therapy: Some individuals, especially those with type 1 diabetes, require insulin therapy to maintain blood sugar levels within a target range.
- Monitoring: Regular monitoring of blood sugar levels helps in adjusting medications and lifestyle changes to better manage diabetes.
The Importance of Medication Adherence
Medication adherence is critical in diabetes management. Non-adherence can lead to poorly controlled blood sugar levels, increasing the risk of complications such as kidney disease, heart disease, and vision loss. Strategies to improve adherence include:
- Understanding Medication: Knowing how your medication works and its importance can motivate adherence.
- Routine Establishment: Incorporating medication intake into a daily routine can improve consistency.
- Use of Reminders: Setting alarms or using pill organizers can help remember medication schedules.
- Open Communication: Regularly communicating with healthcare providers can address concerns and adjust treatment plans as necessary.
Effective diabetes management requires a comprehensive approach that includes lifestyle modifications, medication management, and adherence to prescribed treatments. By adopting healthy habits, taking medications as directed, and working closely with healthcare providers, individuals with diabetes can lead healthy, active lives.
Advanced Diabetes Treatment Technologies
The landscape of diabetes management is evolving rapidly, thanks to the advent of advanced diabetes treatment technologies. These innovations aim to enhance the quality of life for individuals living with diabetes by offering more precise and convenient methods of monitoring and managing their condition. In this section, we delve into three pivotal advancements: Continuous Glucose Monitoring (CGM) systems, insulin pumps and automated insulin delivery systems, and the burgeoning role of telemedicine in diabetes care.
Continuous Glucose Monitoring (CGM) Systems
Continuous Glucose Monitoring (CGM) systems represent a significant leap forward in diabetes management. Unlike traditional blood glucose meters, CGM devices provide real-time insights into glucose levels throughout the day and night. These systems track glucose levels in the interstitial fluid under the skin, offering users the ability to monitor trends and patterns in their glucose levels. This continuous feedback can empower individuals to make more informed decisions about diet, exercise, and medication. CGM systems are particularly beneficial for those requiring tight glucose control, helping to reduce the risk of both hyperglycemia and hypoglycemia by alerting users to glucose level fluctuations.
Insulin Pumps and Automated Insulin Delivery Systems
Insulin pumps and automated insulin delivery systems have transformed insulin administration, providing a more flexible and precise approach compared to traditional injections. An insulin pump is a small, wearable device that delivers short-acting insulin 24 hours a day through a catheter placed under the skin. These devices allow for customizable basal rates to match the body’s varying insulin needs throughout the day and night.
Even more revolutionary are the automated insulin delivery systems, often referred to as “artificial pancreas” systems. These integrate a CGM system with an insulin pump to automatically adjust insulin delivery based on real-time glucose readings. This technology aims to maintain glucose levels within a target range, minimizing the need for manual adjustments and significantly easing the daily burden of diabetes management.
The Potential of Telemedicine in Diabetes Care
Telemedicine has emerged as a powerful tool in diabetes care, offering the potential to dramatically improve access to diabetes management resources. Through telemedicine, patients can consult with their healthcare providers via video calls, phone calls, or messaging, making it easier to receive guidance and adjustments to their treatment plan without the need for in-person visits. This is particularly valuable for individuals in remote or underserved areas, where access to specialized diabetes care may be limited. Telemedicine also facilitates ongoing education and support for diabetes management, encouraging patient engagement and adherence to treatment plans.
Telemedicine not only enhances convenience but also holds the promise of improving diabetes outcomes by providing more timely and personalized care. As the technology and infrastructure for telemedicine continue to improve, its role in diabetes management is set to expand, offering new opportunities for patients to manage their condition effectively.
However, the introduction of advanced diabetes treatment technologies such as CGM systems, insulin pumps, automated insulin delivery systems, and telemedicine is revolutionizing diabetes care. These innovations offer the promise of improved control, convenience, and quality of life for individuals living with diabetes, marking a significant step forward in the ongoing battle against this chronic condition.
Complications and Management of Uncontrolled Diabetes
Managing diabetes effectively is crucial to prevent a range of complications that can severely impact one’s health and quality of life. Uncontrolled diabetes can lead to several serious health issues. Below, we outline some common complications associated with poorly managed diabetes, along with strategies for prevention and regular monitoring to mitigate these risks.
Common Complications of Uncontrolled Diabetes
Cardiovascular Diseases: Diabetes significantly increases the risk of various cardiovascular problems, including coronary artery disease with chest pain (angina), heart attack, stroke, and atherosclerosis (narrowing of arteries). These are among the most serious complications and are the leading cause of mortality in individuals with diabetes.
Kidney Damage (Nephropathy): The kidneys contain millions of tiny blood vessel clusters that filter waste from your blood. Diabetes can damage this delicate filtering system, leading to kidney failure or irreversible end-stage kidney disease, which may require dialysis or a kidney transplant.
Eye Damage (Retinopathy) and Potential Blindness: Diabetes can damage the blood vessels of the retina (diabetic retinopathy), potentially leading to blindness. Diabetes also increases the risk of other serious vision conditions, such as cataracts and glaucoma.
Preventive Strategies and Regular Monitoring
Prevention and regular monitoring are key to managing diabetes and avoiding its complications. Here are strategies to help manage diabetes effectively:
- Maintain Blood Sugar Levels Within Target Ranges: Regular monitoring of blood sugar levels and maintaining them within the target range can significantly reduce the risk of complications.
- Healthy Lifestyle Choices: Adopting a healthy lifestyle is critical. This includes eating a balanced diet, maintaining a healthy weight, exercising regularly, and avoiding tobacco use. These actions can help manage your diabetes and reduce the risk of complications.
- Regular Check-ups and Monitoring: Regular appointments with your healthcare provider are essential to monitor your health and manage your diabetes effectively. This includes regular screenings for cardiovascular diseases, kidney damage, and eye damage.
- Medication Adherence: If medication is prescribed, taking it as directed by your healthcare provider can help control your diabetes and prevent complications.
- Education and Support: Educating yourself about diabetes and having a support system can help you manage your diabetes more effectively. Consider joining a support group or seeking out educational resources to better understand and manage your condition.
Managing diabetes is a lifelong commitment, and by taking proactive steps to monitor and control your blood sugar levels, adopting healthy lifestyle habits, and seeking regular medical care, you can significantly reduce the risk of complications and lead a healthy, active life.
Living with Diabetes: Navigating the Challenges
Diabetes, a chronic condition affecting millions globally, has far-reaching impacts on both physical and mental health. Understanding the multifaceted challenges of living with diabetes is crucial for managing the condition effectively. This section explores the impact of diabetes on mental health and quality of life, offers strategies for coping in daily life, and underscores the importance of support from healthcare professionals and diabetes support groups.
The Impact of Diabetes on Mental Health and Quality of Life
Living with diabetes can significantly affect one’s mental health and overall quality of life. Individuals with diabetes are at a higher risk of experiencing mental health issues such as depression, anxiety, and diabetes-related distress. This can stem from the constant monitoring of blood glucose levels, dietary restrictions, and the fear of potential complications. The psychological burden of managing diabetes daily can lead to feelings of isolation and frustration, affecting an individual’s well-being and quality of life.
Strategies for Coping with Diabetes in Daily Life
Coping with diabetes requires a multifaceted approach, focusing on both physical health and mental well-being. Here are some strategies that can help:
- Education and Self-Management: Understanding diabetes and its management can empower individuals to take control of their health. Learning about nutrition, exercise, and medication management is key.
- Routine Monitoring: Regular monitoring of blood glucose levels helps in managing diabetes effectively and reduces the risk of complications.
- Healthy Lifestyle Choices: Incorporating a balanced diet, regular physical activity, and adequate sleep can significantly improve blood sugar control and overall health.
- Stress Management: Techniques such as mindfulness, meditation, and yoga can help reduce stress, which is particularly important as stress can negatively impact blood glucose levels.
The Importance of Support from Healthcare Professionals and Diabetes Support Groups
Support from healthcare professionals is vital in the effective management of diabetes. Regular consultations with doctors, dietitians, and diabetes educators can provide personalized guidance and adjustments to treatment plans as needed. Moreover, diabetes support groups offer a platform for sharing experiences, tips, and encouragement with others who understand the challenges of living with diabetes. This sense of community can alleviate feelings of isolation and provide valuable emotional support.
Living with diabetes presents unique challenges that can affect an individual’s mental health and quality of life. However, through effective coping strategies, education, and support from healthcare professionals and peer support groups, individuals with diabetes can lead fulfilling lives. Embracing a holistic approach to diabetes management not only helps in controlling the condition but also improves overall well-being.
In navigating the journey of living with diabetes, remember, you are not alone. There are numerous resources and communities ready to support you every step of the way.
Future Trends in Diabetes Treatment: Innovations on the Horizon
The landscape of diabetes treatment is on the cusp of revolutionary change, propelled by significant research advancements and emerging technologies. As the global diabetic population continues to rise, the quest for more effective, personalized, and less invasive treatments has intensified. This article delves into the most promising future trends in diabetes care, including stem cell therapy, artificial pancreas developments, and the pivotal role of personalized medicine.
Stem Cell Therapy: A New Dawn in Diabetes Care
Stem cell therapy represents one of the most exciting frontiers in diabetes treatment. This innovative approach involves using stem cells to regenerate or repair the body’s tissues or organs, offering the potential to address the root causes of diabetes. For type 1 diabetes, researchers are focusing on creating insulin-producing beta cells from stem cells to replace the ones destroyed by the body’s immune system. This could lead to a paradigm shift in treatment, moving from managing symptoms to potentially curing the disease.
Artificial Pancreas Developments: Towards Automated Insulin Delivery
The development of the artificial pancreas marks a significant technological advancement in diabetes management. This device mimics the glucose-regulating function of a healthy pancreas by automatically monitoring and adjusting blood glucose levels. It uses a continuous glucose monitor (CGM) and an insulin pump to deliver insulin as needed, based on real-time data. Current models have shown promising results in improving glycemic control and reducing the burden of daily diabetes management. Future enhancements are expected to offer even more precise control and user-friendly interfaces.
Personalized Medicine: Tailoring Diabetes Care to the Individual
Personalized medicine in diabetes care is gaining traction as a means to tailor treatment to the individual’s genetic makeup, lifestyle, and specific health needs. This approach leverages advances in genomics and data analytics to understand the unique factors affecting each person’s diabetes. By identifying genetic markers and other risk factors, healthcare providers can prescribe the most effective medications, recommend lifestyle changes, and predict potential complications. Personalized medicine aims to optimize treatment outcomes, minimize side effects, and improve the quality of life for people with diabetes.
The future of diabetes treatment is bright, with stem cell therapy, artificial pancreas developments, and personalized medicine leading the charge towards more effective, convenient, and customized care. These advancements promise to transform the lives of millions of people with diabetes, offering hope for a healthier, more manageable future. As research continues to progress, the dream of a world where diabetes can be effectively cured or managed with minimal impact on daily life moves ever closer to reality.
Conclusion
In summary, our discussion emphasized the multifaceted aspects of diagnosing and treating diabetes, highlighting the critical steps and considerations involved in effectively managing this chronic condition. We delved into the significance of early detection, the various diagnostic tests available, and the pivotal role of personalized treatment plans that cater to the individual needs of patients. Furthermore, we explored the impact of lifestyle modifications, such as diet and exercise, alongside medical interventions in controlling blood sugar levels and preventing complications associated with diabetes.
The comprehensive approach to diabetes diagnosis and treatment cannot be overstated. It is crucial for healthcare providers and patients to work hand in hand, utilizing a holistic strategy that encompasses not only medical treatments but also lifestyle adjustments. This collaborative effort is essential in achieving optimal health outcomes and enhancing the quality of life for those living with diabetes.
We strongly encourage individuals, whether at risk for diabetes or currently managing the condition, to seek professional advice and engage in regular check-ups. Regular monitoring and consultation with healthcare professionals are paramount in adapting treatment plans as needed and addressing any health concerns promptly. Taking proactive steps towards your health can significantly influence the management of diabetes, leading to a healthier and more fulfilling life.
In closing, remember that managing diabetes is a continuous journey that requires dedication and informed decisions. With the right support and a commitment to your health, diabetes can be managed effectively, allowing individuals to lead vibrant, healthy lives.