Dengue Fever Treatment: Dengue fever, a mosquito-borne viral infection, poses significant global health challenges. With millions of cases reported annually, understanding the nuances of diagnosis and treatment is essential for effective management and control of this disease.
This comprehensive guide delves into the critical aspects of diagnosing and treating dengue fever, offering insights into the latest medical advancements and practical strategies for those affected.
Understanding Dengue Fever
Dengue fever is a mosquito-borne illness that poses significant health risks in many tropical and subtropical regions around the world. Understanding how dengue fever is transmitted, along with its signs and symptoms, is crucial for prevention and early treatment. This article aims to provide a comprehensive overview of dengue fever, focusing on its transmission methods and the clinical manifestations that infected individuals may experience.
How is Dengue Fever Transmitted?
Dengue fever is primarily transmitted through the bite of an infected Aedes mosquito, notably Aedes aegypti and Aedes albopictus. These mosquitoes are daytime feeders, with peak periods of activity at dawn and dusk. When a mosquito bites a person infected with the dengue virus, the mosquito becomes a carrier of the virus. Upon biting another person, the virus is transmitted, leading to the spread of dengue fever.
It’s important to note that dengue cannot be spread directly from person to person. The transmission cycle is strictly through mosquitoes, making mosquito control and prevention measures essential in combating the disease. Areas with stagnant water are prime breeding grounds for these mosquitoes, emphasizing the importance of maintaining clean surroundings to reduce dengue transmission risks.
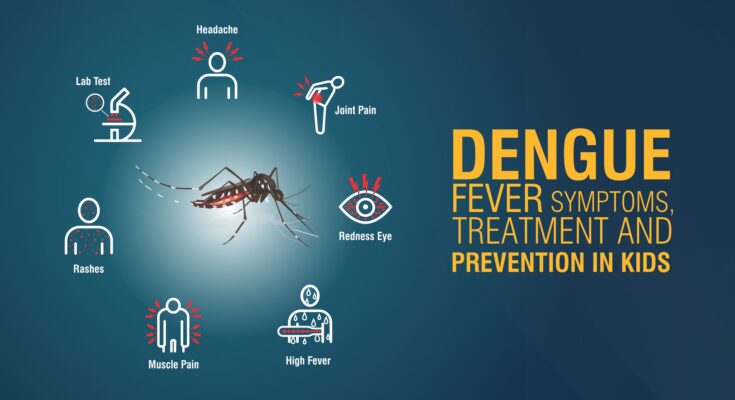
Signs and Symptoms of Dengue Fever
Dengue fever is characterized by a wide range of symptoms, which can vary from mild to severe. The onset of symptoms typically occurs 4 to 10 days after being bitten by an infected mosquito. Common signs and symptoms include:
- High Fever: A sudden, high fever that can reach up to 104°F (40°C) is often one of the first signs of dengue fever.
- Severe Headache: Individuals may experience intense headaches, primarily in the forehead area.
- Pain Behind the Eyes: A distinctive symptom of dengue fever is a deep pain behind the eyes, which may worsen with eye movement.
- Joint and Muscle Pain: Dengue fever can cause severe joint and muscle pain, often described as “breakbone fever” due to the intensity of the discomfort.
- Nausea and Vomiting: Digestive disturbances, including nausea and vomiting, are common among those infected.
- Rash: Many individuals develop a rash, which can appear a few days after the fever or simultaneously. The rash may cover much of the body, often starting on the torso and spreading to the limbs and face.
- Mild Bleeding: Symptoms may include mild bleeding from the nose or gums, or easy bruising on the skin.
In severe cases, dengue fever can progress to more serious forms, such as dengue hemorrhagic fever or dengue shock syndrome, which require immediate medical attention. These conditions are marked by severe abdominal pain, persistent vomiting, rapid breathing, bleeding gums, fatigue, restlessness, and blood in vomit or stools.
By employing effective mosquito control measures and seeking prompt medical care when symptoms are present, the impact of dengue fever can be significantly reduced.
Diagnosis of Dengue Fever
Early diagnosis can significantly improve patient outcomes, making understanding the diagnostic process vital for healthcare providers and patients alike. Below, we outline the steps involved in diagnosing dengue fever, delve into the common diagnostic tests used, and highlight the importance of medical history and travel information in the diagnosis.
List Steps in Diagnosing Dengue Fever
- Initial Evaluation: The process begins with a thorough evaluation of symptoms. Common symptoms of dengue fever include high fever, severe headache, pain behind the eyes, joint and muscle pain, fatigue, nausea, vomiting, skin rash, and mild bleeding (such as nose or gum bleed).
- Medical History and Travel Information: The healthcare provider will inquire about the patient’s medical history and any recent travel to dengue-endemic areas. This information is crucial because dengue fever is more likely in individuals who have recently visited regions where the disease is prevalent.
- Physical Examination: A detailed physical examination is conducted to check for signs of dengue fever, such as swollen glands and rash.
- Diagnostic Tests: Based on the initial evaluation, medical history, and physical examination, the healthcare provider may recommend specific diagnostic tests to confirm the presence of the dengue virus.
Common Diagnostic Tests for Dengue Fever
- Blood Tests: A complete blood count (CBC) can reveal low levels of white blood cells and platelets, common in dengue patients.
- NS1 Antigen Tests: The NS1 antigen test can detect the dengue virus as early as the first day of symptoms and up to the first seven days. This test is particularly useful for early diagnosis.
- PCR Tests: Polymerase chain reaction (PCR) tests are used to detect the genetic material of the dengue virus. This test is highly specific and can identify the presence of the virus in the first week of infection.
The Role of Medical History and Travel Information in Diagnosis
The importance of a patient’s medical history and travel information cannot be overstated in the diagnosis of dengue fever. Knowing whether a patient has recently been to a dengue-endemic area can significantly guide the diagnostic process. Additionally, understanding a patient’s medical history helps healthcare providers identify any factors that may increase the risk of severe dengue complications. Collectively, this information aids in making a prompt and accurate diagnosis, thereby facilitating timely and appropriate treatment.
However, diagnosing dengue fever involves a combination of symptom evaluation, medical history review, physical examination, and specific diagnostic tests. Early and accurate diagnosis is key to managing dengue fever effectively, highlighting the importance of awareness and understanding of the diagnostic process among healthcare providers and at-risk populations.
Treatment Options for Dengue Fever
This article explores the various treatment options for dengue fever, emphasizing home care remedies, medical treatments, and the critical importance of monitoring for severe complications like Dengue Hemorrhagic Fever (DHF) and Dengue Shock Syndrome (DSS).
Home Care and Remedies
For many individuals diagnosed with dengue fever, home care is a vital component of their treatment plan. The following home care strategies and remedies can provide relief and support recovery:
- Stay Hydrated: Dengue fever can cause dehydration, especially if vomiting or high fever is present. Drinking plenty of fluids, such as water, coconut water, or oral rehydration solutions, helps maintain hydration levels and aids the recovery process.
- Rest: Adequate rest is crucial for recovery. The body’s immune system works best when well-rested, helping to fight off the virus more effectively.
- Pain Relievers: Use over-the-counter pain relievers like acetaminophen (Tylenol) to alleviate pain and reduce fever. Avoid aspirin or ibuprofen, as these can increase bleeding risks.
- Monitor Symptoms: Keep a close eye on symptoms. If they worsen or new symptoms emerge, such as severe abdominal pain, persistent vomiting, or difficulty breathing, seek medical attention immediately.
Medical Treatments for Dengue Fever
In cases of severe dengue or complications, hospitalization may be necessary to closely monitor the patient and provide supportive care, including:
- Intravenous (IV) Fluids and Electrolyte Replacement: To prevent dehydration, especially in cases of severe vomiting or diarrhea.
- Blood Transfusion: For patients experiencing significant bleeding.
- Oxygen Therapy: For those with difficulty breathing.
It’s important to follow a healthcare provider’s advice and complete any prescribed treatment plan.
The Importance of Monitoring for Dengue Hemorrhagic Fever and Dengue Shock Syndrome
Dengue Hemorrhagic Fever (DHF) and Dengue Shock Syndrome (DSS) are severe complications of dengue fever. Early detection and treatment are crucial to prevent life-threatening outcomes. Symptoms of DHF include severe abdominal pain, persistent vomiting, rapid breathing, bleeding gums, fatigue, restlessness, and blood in vomit or stools. DSS, the more severe form, can lead to profound shock, organ failure, and even death if not promptly treated.
Monitoring for these symptoms and seeking immediate medical care if they develop is critical. Early hospitalization and aggressive supportive care can significantly improve survival rates.
Vigilance in monitoring for signs of Dengue Hemorrhagic Fever and Dengue Shock Syndrome is vital to ensuring a positive outcome. Always consult healthcare professionals for advice tailored to individual health needs and circumstances.
Preventing Dengue Fever
Preventing the spread of dengue is crucial to public health, focusing primarily on mosquito control and personal protection measures. Additionally, advancements in vaccination play a vital role in combating this disease. This section outlines effective strategies for dengue prevention, including the current status of dengue fever vaccines and recommendations for their use.
Preventive Measures: Mosquito Control and Personal Protection
Mosquito Control: Reducing mosquito populations is a cornerstone of dengue prevention. This can be achieved through:
- Eliminating Standing Water: Mosquitoes breed in standing water. Regularly emptying water from containers such as flowerpots, buckets, and barrels is essential.
- Use of Insecticides: Applying insecticides to water storage containers can help kill mosquito larvae. However, this should be done according to local health guidelines to ensure safety and effectiveness.
- Community Efforts: Community-wide efforts to clean up areas that can harbor mosquitoes, such as blocked drains and non-biodegradable litter, are effective in reducing mosquito populations.
Personal Protection: Individuals can take several steps to protect themselves from mosquito bites, including:
- Mosquito Repellents: Applying insect repellent containing DEET, picaridin, or oil of lemon eucalyptus on exposed skin and clothing.
- Protective Clothing: Wearing long-sleeved shirts and long pants, especially during peak mosquito activity times (dawn and dusk).
- Use of Mosquito Nets: Sleeping under mosquito nets, particularly those treated with insecticide, can provide significant protection.
Vaccination: Current Status of Dengue Fever Vaccines and Recommendations
Vaccination against dengue fever has emerged as a promising avenue for prevention. The development and deployment of dengue vaccines aim to reduce the incidence of dengue infections and, subsequently, the severity and mortality associated with this disease.
As of my last update, several dengue vaccines are in various stages of research, development, and approval. The World Health Organization (WHO) has provided guidelines for the use of the first dengue vaccine, Dengvaxia (CYD-TDV), which is licensed for use in several countries. It is recommended for individuals aged 9 to 45 years living in areas with high endemicity of dengue virus.
Recommendations for Vaccination:
- Target Population: The vaccine is recommended for individuals who have been previously infected with the dengue virus, as it has been shown to be more effective in such cases.
- Screening Before Vaccination: Health authorities recommend serological testing to determine past dengue infection before vaccination.
- Integration with Other Prevention Measures: Vaccination should be part of an integrated dengue prevention strategy, including mosquito control and personal protective measures.
It’s important to note that the landscape of dengue vaccination is rapidly evolving, with ongoing research aimed at developing more effective and broadly applicable vaccines. Individuals living in or traveling to dengue-endemic regions should consult healthcare providers for the most current recommendations and vaccine availability.
By adhering to these recommended practices, communities and individuals can significantly reduce the risk of dengue transmission and its associated health impacts. As the field of dengue vaccine development advances, staying informed about new recommendations and vaccine options will be crucial for ongoing dengue prevention efforts.
When to Seek Medical Help for Dengue Fever
Recognizing the signs of severe Dengue and understanding the importance of early medical intervention are crucial steps in preventing these adverse outcomes. This guide will help you identify when to seek medical help and underscore the significance of prompt action.
Identifying Signs of Severe Dengue Fever
Severe Dengue Fever, also known as Dengue Hemorrhagic Fever, can develop rapidly, and early recognition of its signs is vital. If you or someone you know is experiencing any of the following symptoms, it’s essential to seek medical attention immediately:
- Sudden, high fever that can last from 2 to 7 days, often accompanied by severe headaches, pain behind the eyes, muscle and joint pains, and fatigue.
- Skin rash, which appears two to five days after the onset of fever.
- Bleeding, such as nosebleeds, bleeding gums, or easy bruising, indicating a potential for more severe bleeding complications.
- Severe abdominal pain, persistent vomiting, and rapid breathing. These symptoms may suggest shock, organ impairment, or severe dehydration.
- Changes in blood pressure, leading to lightheadedness or fainting. These could signal the onset of Dengue Shock Syndrome, a life-threatening complication.
The Importance of Early Medical Intervention
Early medical intervention can significantly reduce the risk of developing severe complications from Dengue Fever. When Dengue symptoms are caught early, healthcare providers can closely monitor the patient’s condition, manage symptoms, and prevent progression to more serious stages. Treatment in the early phases can involve hydration, pain relief measures, and careful observation of vital signs and blood parameters.
The timely treatment of Dengue Fever is essential for several reasons:
- Preventing severe complications: Early intervention can prevent complications such as Dengue Hemorrhagic Fever and Dengue Shock Syndrome, which can be fatal.
- Reducing the risk of transmission: Seeking medical help not only benefits the affected individual but also helps in controlling the spread of the disease. Early diagnosis and management can reduce the number of mosquitoes carrying the Dengue virus by limiting their access to infected blood.
- Improving outcomes: Patients who receive prompt medical care generally have better health outcomes and a quicker recovery compared to those who delay treatment.
If you suspect you or someone you know is showing signs of severe Dengue, don’t hesitate to seek medical attention immediately. Awareness and prompt action can make a significant difference in the fight against this potentially life-threatening illness.
Living with Dengue Fever
This article aims to provide valuable insights into managing Dengue Fever symptoms at home and understanding its long-term effects, including strategies for dealing with recurrent infections.
Managing Dengue Fever Symptoms at Home
When diagnosed with Dengue Fever, the primary goal is to alleviate symptoms and prevent complications. Here’s how you can manage the illness at home:
- Stay Hydrated: Dengue can cause dehydration, especially if fever and vomiting are present. It’s essential to drink plenty of fluids, including water, soups, and oral rehydration solutions, to stay hydrated.
- Rest: Your body needs energy to fight off the virus. Ensure you get ample rest, as fatigue is a common symptom of Dengue.
- Fever and Pain Management: Over-the-counter pain relievers like acetaminophen (Tylenol) can help reduce fever and alleviate pain. However, avoid aspirin or ibuprofen, as they can increase the risk of bleeding.
- Monitor Symptoms: Keep a close eye on symptoms. Seek immediate medical attention if you experience severe abdominal pain, persistent vomiting, rapid breathing, or bleeding from the nose or gums.
Long-term Effects of Dengue Fever
For some individuals, Dengue Fever can have lingering effects even after recovery. Fatigue and depression can persist for weeks or months. Joint pain is another long-term complaint reported by some. It’s important to consult healthcare providers if post-recovery symptoms do not improve, as they can advise on the best course of action to mitigate these long-term effects.
Managing Recurrent Dengue Infections
Re-infection with Dengue virus can happen and may result in a more severe form of the disease known as severe dengue or dengue hemorrhagic fever. To manage and reduce the risk of recurrent infections:
- Prevent Mosquito Bites: Use mosquito repellents, wear long-sleeved shirts and long pants, and ensure window and door screens are intact to prevent mosquitoes from entering your home.
- Eliminate Mosquito Breeding Sites: Regularly empty standing water from containers such as flowerpots and buckets to reduce mosquito breeding grounds.
- Community Efforts: Participate in community cleanup efforts to reduce mosquito habitats collectively.
By following the recommended home care strategies and taking preventive measures against mosquito bites, individuals can recover more comfortably and reduce the risk of recurrent infections. Always consult a healthcare provider for personalized advice and treatment options. Remember, prevention is key in combating Dengue Fever and safeguarding your health and that of your community.
FAQs about Dengue Fever Treatment
1. What is the first step in treating Dengue fever?
The initial approach to treating Dengue fever involves resting, staying hydrated, and taking acetaminophen (Tylenol) to alleviate pain and fever. It is crucial to avoid aspirin and non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, as they can increase the risk of bleeding complications.
2. When should someone with Dengue fever seek hospital care?
Hospitalization is recommended if symptoms worsen or if signs of severe Dengue, such as severe abdominal pain, persistent vomiting, rapid breathing, bleeding gums, fatigue, or blood in vomit, appear. Early detection and supportive care in a hospital can significantly reduce the risk of complications and fatality.
3. Can Dengue fever be treated at home?
Mild cases of Dengue fever can often be managed at home with proper care, including adequate fluid intake to avoid dehydration, rest, and the use of fever-reducing medications. However, it is essential to monitor symptoms closely and seek medical advice if symptoms worsen or do not improve within a few days.
4. Are there any effective home remedies for Dengue fever?
While no home remedy can cure Dengue fever, certain practices can help manage symptoms. Hydration is crucial; drinking water, coconut water, or herbal teas can help. Papaya leaf extract has also been cited for its potential to increase platelet count, although scientific evidence is limited. Always consult with a healthcare provider before trying any home remedies.
5. How long does it take to recover from Dengue fever?
Recovery time varies depending on the severity of the disease. Most individuals start to feel better within a week or two after the onset of symptoms. However, it is common to feel tired and somewhat depressed for weeks to months following recovery. Complete recovery can take up to six weeks.
6. Is there a vaccine for Dengue fever?
Yes, there is a vaccine for Dengue fever, known as Dengvaxia (CYD-TDV), approved in several countries for individuals aged 9 to 45 living in areas where Dengue is endemic. The vaccine is administered in three doses over 12 months. However, it is recommended only for those who have been previously infected with the Dengue virus, as it can increase the risk of severe Dengue in those who have not been previously infected.
Conclusion:
Preventive measures play a critical role in the fight against Dengue Fever. These include using insect repellent, wearing long-sleeved shirts and long pants, and ensuring living areas are free from standing water where mosquitoes breed. Public health campaigns and community efforts are also vital in raising awareness and reducing the risk of Dengue transmission.
We urge our readers to take proactive steps in protecting themselves and their loved ones from Dengue Fever. If you or someone you know exhibits symptoms associated with Dengue, such as high fever, severe headache, pain behind the eyes, joint and muscle pain, nausea, vomiting, swollen glands, or rash, seek medical advice immediately. Early detection and treatment are crucial for a positive outcome.
Together, by taking preventive actions and seeking timely medical care for symptoms, we can significantly reduce the impact of Dengue Fever on our communities. Let’s join hands in making our environment safer and in promoting health and wellbeing for all.