Delirium Symptoms: Delirium, often characterized by a sudden change in brain function, presents a complex interplay of symptoms that can significantly affect an individual’s cognitive abilities, emotional state, and overall health.
Understanding the symptoms and causes of delirium is crucial for early detection and effective management of this acute medical condition.
This article aims to provide a comprehensive overview of delirium, highlighting its key symptoms, potential causes, and the importance of timely intervention.
Understanding Delirium: A Comprehensive Guide
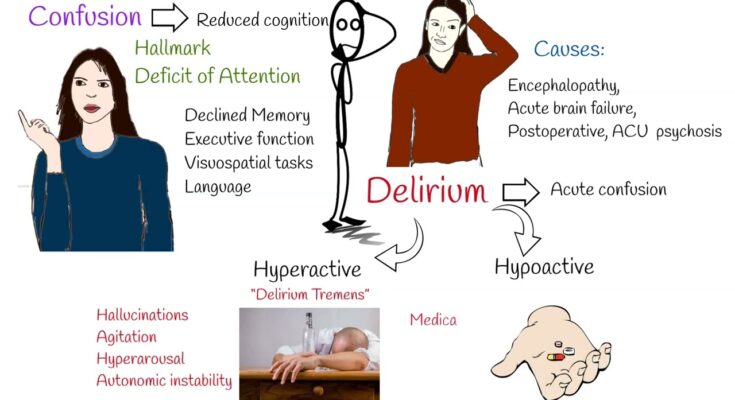
Delirium, often misunderstood and misdiagnosed, is a serious disturbance in mental abilities that results in confused thinking and reduced awareness of the environment. Unlike dementia, which develops gradually over time, delirium comes on suddenly, usually within hours or days. It’s crucial to distinguish delirium from similar conditions such as depression or dementia, as each requires a different approach to care. Delirium typically involves rapid changes in brain function that can be alarming both to the patient and to those around them.
What Makes Delirium Unique?
The hallmark of delirium is a significant fluctuation in cognitive function, characterized by confusion, disorientation, and an inability to focus or think clearly. Patients may also experience hallucinations, delusions, and extreme shifts in mood and behavior. These symptoms set delirium apart from other cognitive disorders, which tend to have a more steady progression. Understanding this distinction is vital for healthcare providers to administer the appropriate interventions promptly.
The Importance of Recognizing Delirium Symptoms
Recognizing the symptoms of delirium is crucial for both patients and healthcare providers. Early identification and treatment can significantly impact the patient’s recovery trajectory. For healthcare providers, understanding the signs of delirium allows for the quick implementation of treatment strategies that can mitigate symptoms and address the underlying cause. For patients and families, awareness of delirium symptoms can prompt timely medical attention, reducing the risk of long-term cognitive and physical decline.
For patients, delirium can be frightening and disorienting, affecting their ability to communicate their needs or participate in their care. Family members and caregivers play a critical role in recognizing changes in the patient’s mental status and advocating for their care. Healthcare providers should also be vigilant for delirium signs in patients, especially those at higher risk, such as the elderly, those with previous cognitive impairments, or those undergoing surgery or receiving palliative care.
Symptoms of Delirium: A Comprehensive Guide
Understanding the symptoms of delirium is crucial for early identification and management. This guide aims to provide caregivers and family members with the knowledge needed to recognize these signs promptly.
Common Symptoms of Delirium
Delirium symptoms can vary widely among individuals but generally fall into several categories:
- Confusion and Disorientation: One of the most noticeable signs is a sudden difficulty in understanding time, place, or identity. The individual may not know where they are, the current date, or even recognize familiar faces.
- Changes in Cognitive Function: This includes difficulty with memory, attention, and thinking processes. The person might have trouble following conversations, be easily distracted, or unable to remember recent events.
- Altered Levels of Consciousness: This can range from hyperalertness to drowsiness or lethargy. Some may experience rapid shifts between these states throughout the day.
- Hallucinations and Delusions: Visual or auditory hallucinations can occur, where the person sees or hears things that aren’t there. Delusions, or false beliefs, may also develop, such as thinking they are being persecuted.
- Emotional Disturbances: Rapid changes in mood are common, including anxiety, depression, irritability, or even euphoria without a clear reason.
- Speech and Language Difficulty: The individual might ramble, make little sense, or have trouble finding the right words. Their speech can be unusually slow or rapid.
- Physical Changes: These may include changes in sleep patterns, appetite, and energy levels. There might also be an increase in falls or a noticeable decline in personal hygiene.
Identifying Delirium Symptoms: Tips for Caregivers and Family Members
Recognizing delirium early is essential for effective management and treatment. Here are some tips to help identify the symptoms:
- Monitor for Sudden Changes: Keep an eye out for rapid changes in behavior, mood, or cognitive function. Delirium typically develops over a short period, often hours to days.
- Create a Baseline: Understand the individual’s normal behavior and mental function to better identify any deviations that might indicate delirium.
- Pay Attention to Communication: Difficulty in expressing thoughts coherently or understanding what is being said can be a key sign of delirium.
- Observe Physical and Emotional State: Look for signs of lethargy, restlessness, or emotional instability that deviate from the person’s usual demeanor.
- Check for Environmental Factors: Sometimes, changes in the environment can trigger delirium. Ensure the individual is in a familiar, calm setting and check for any potential stressors.
- Consult Healthcare Professionals: If you suspect delirium, seek medical advice promptly. Early intervention can make a significant difference in recovery.
However, understanding and recognizing the symptoms of delirium can greatly assist caregivers and family members in providing the necessary support and ensuring timely medical intervention. Awareness and education are key components in improving outcomes for those affected by this complex condition.
Causes of Delirium
Recognizing these causes is crucial for prevention, early detection, and treatment. Below, we delve into the primary causes of delirium, spanning medical conditions, environmental factors, and the vulnerability of certain populations.
Medical Conditions Leading to Delirium
Several medical conditions are known to precipitate delirium. These include:
- Infections: The body’s response to infection can affect brain function, leading to symptoms of delirium. Urinary tract infections, pneumonia, and sepsis are common culprits.
- Surgery: Postoperative delirium can occur, particularly in older adults or those with pre-existing cognitive impairments. The stress of surgery, anesthesia, and pain medications can contribute to this condition.
- Medication Side Effects: Many medications can cause delirium, especially if used in large doses or in sensitive individuals. These include sedatives, narcotics, and medications with anticholinergic properties.
Environmental Factors
The environment plays a significant role in the development of delirium, particularly:
- Hospitalization: The unfamiliar surroundings, disrupted sleep patterns, and the stress of hospital stays can trigger delirium, especially in intensive care units.
- Lack of Sleep: Sleep deprivation can exacerbate or lead to delirium symptoms, highlighting the importance of adequate rest for mental health.
Vulnerable Populations
Certain groups are more susceptible to delirium, including:
- The Elderly: Age-related changes in brain function and a higher likelihood of underlying health conditions make older adults particularly vulnerable to delirium.
- Those with Pre-existing Mental Health Conditions: Individuals with baseline cognitive impairments, such as dementia, are at increased risk of delirium.
Interaction of Factors
The development of delirium often involves an interaction between physical health, medication use, and environmental factors. For instance, an elderly person with a urinary tract infection may be more likely to develop delirium if they are also taking multiple medications and experiencing disrupted sleep in a hospital setting. This underscores the importance of a holistic approach in preventing and managing delirium, with careful consideration of all potential contributing factors.
However, understanding the causes of delirium is key to addressing this complex condition. By recognizing the interplay between medical conditions, environmental factors, and individual vulnerabilities, healthcare providers can better prevent and manage delirium, ultimately improving patient outcomes.
Risk Factors and Prevention of Delirium
Understanding the risk factors and implementing effective prevention strategies are crucial steps in managing this condition. This article will explore how to identify individuals at high risk for delirium, strategies for prevention, including medical and environmental approaches, and the importance of careful medication management and treating underlying conditions.
Identifying High-Risk Individuals
The first step in preventing delirium is identifying those who are at high risk. High-risk populations typically include older adults, especially those with previous cognitive impairments such as dementia, patients undergoing major surgery, those with severe or chronic medical conditions, and individuals taking multiple medications. Hospitalized patients, particularly those in intensive care units or those with infections, are also at increased risk. Recognizing these risk factors allows healthcare providers to implement targeted prevention strategies effectively.
Strategies for Preventing Delirium
Prevention of delirium involves a multifaceted approach that addresses both medical and environmental factors.
Medical Approaches
Careful Medication Management: Medications can sometimes contribute to delirium, especially in older adults or those taking multiple drugs. A careful review of a patient’s medications can help identify and minimize the use of drugs with a high risk of causing delirium. This includes adjusting dosages or substituting medications when possible.
Treating Underlying Conditions: Promptly addressing any underlying medical conditions is crucial. This includes treating infections, ensuring proper hydration and nutrition, and managing chronic conditions effectively. Addressing these issues can significantly reduce the risk of delirium.
Environmental Strategies
Ensuring Proper Sleep Hygiene: Poor sleep can exacerbate or contribute to delirium. Implementing strategies to promote good sleep hygiene is essential. This can include minimizing noise and light disruptions, maintaining a regular sleep schedule, and avoiding sleep-disrupting medications when possible.
Orientation Aids: For hospitalized patients, especially, providing orientation aids can help prevent delirium. This includes ensuring that clocks, calendars, and personal items are visible and accessible, helping the patient stay grounded and aware of their surroundings.
By identifying individuals at high risk, managing medications carefully, treating underlying conditions, and ensuring a supportive environment, it is possible to significantly reduce the incidence and severity of delirium. These efforts not only improve the quality of life for at-risk individuals but also support better overall health outcomes.
Diagnosing Delirium: A Comprehensive Guide
Understanding the diagnostic process is crucial for patients, caregivers, and healthcare professionals alike. This article delves into the methods of diagnosing delirium, highlighting the significance of medical assessments, tests, and the pivotal role of medical history and physical examination.
Methods of the Diagnostic Process
The diagnosis of delirium involves a multi-faceted approach, combining clinical assessment with a variety of medical tests to rule out other conditions with similar symptoms. Here’s an overview of the diagnostic steps:
- Clinical Assessment: Healthcare professionals begin with a detailed clinical assessment to identify signs of delirium, such as rapid onset of symptoms, fluctuating cognitive abilities, and changes in alertness and attention.
- Cognitive Tests: Tests like the Confusion Assessment Method (CAM) are utilized to evaluate cognitive function and identify specific indicators of delirium.
- Laboratory Tests: Blood tests are performed to check for infections, electrolyte imbalances, and organ function that might contribute to delirium.
- Imaging Tests: Brain imaging, through CT scans or MRIs, can help identify brain abnormalities or stroke that could be causing the symptoms.
- Medication Review: A thorough review of the patient’s current medications is essential, as certain drugs can trigger delirium.
Medical Assessments and Tests Used
To accurately diagnose delirium, medical professionals rely on a series of assessments and tests:
- Blood Tests: These can reveal vital information about the patient’s general health, including signs of infection, liver and kidney function, and nutritional deficiencies.
- Urine Tests: Urinalysis helps in identifying urinary tract infections or dehydration, common triggers for delirium.
- Brain Imaging: CT scans or MRIs are critical in detecting brain injuries, tumors, or infections that might be responsible for the patient’s symptoms.
- Electroencephalogram (EEG): Although less common, an EEG may be used to measure electrical activity in the brain, particularly if seizures are suspected.
Role of Medical History and Physical Examination
A thorough medical history and physical examination are cornerstone elements in the diagnosis of delirium. These steps allow healthcare providers to gather essential information about:
- Previous Medical Conditions: Knowing the patient’s medical background, including any history of dementia or mental health issues, is vital.
- Symptom Onset: Understanding when symptoms started and how they have progressed is crucial for distinguishing delirium from other cognitive disorders.
- Medication Use: A comprehensive review of all medications, including over-the-counter drugs and supplements, is necessary to identify any potential contributors to delirium.
- Physical Examination: A detailed physical exam can uncover signs of underlying physical health issues, such as infections or heart problems, that could be causing or exacerbating delirium.
This approach ensures a comprehensive evaluation, enabling healthcare professionals to tailor treatment plans effectively and improve outcomes for patients experiencing delirium. Understanding these diagnostic steps can empower patients and caregivers, fostering a collaborative environment conducive to recovery and well-being.
Treatment and Management of Delirium
Managing and treating delirium involves a multi-faceted approach tailored to the individual’s specific symptoms and underlying causes. This guide outlines the general approaches to treatment, the medications and therapies used, the importance of addressing underlying causes, and provides tips for caregivers and family members.
General Approaches to Treatment
The treatment for delirium begins with identifying and addressing the underlying causes. Healthcare providers focus on creating a supportive and safe environment for the patient. This involves:
- Ensuring proper hydration and nutrition: Adequate fluids and a balanced diet can help mitigate symptoms.
- Creating a calm and comfortable environment: Reducing noise, providing adequate lighting, and maintaining a comfortable room temperature can help.
- Minimizing changes: Keeping the patient’s environment and caregivers consistent can reduce confusion and agitation.
- Ensuring adequate rest and sleep: Establishing a routine that encourages regular sleep patterns is crucial.
- Encouraging mobility: If possible, assisting the patient with walking or moving can aid in recovery.
Medications and Therapies Used
Medication may be used to manage symptoms of delirium, but it’s typically reserved for cases of severe agitation or distress that pose a risk to the patient or others. The most commonly used medications include:
- Antipsychotics: These can reduce symptoms of delirium, but they must be used carefully, considering potential side effects.
- Benzodiazepines: Primarily used in delirium due to alcohol withdrawal, these should be used sparingly in other types of delirium due to the risk of worsening confusion.
Non-pharmacological therapies are often effective in managing delirium and include:
- Cognitive stimulation: Engaging the patient in simple, grounding conversations can help.
- Orientation aids: Clocks, calendars, and personal items can help the patient stay connected to reality.
- Physical therapy and occupational therapy: These can help maintain or improve mobility and daily functioning.
Importance of Addressing Underlying Causes
Delirium is often a symptom of another medical condition, medication side effect, or a result of substance withdrawal. Therefore, it’s crucial to identify and treat the underlying cause. This may involve:
- Adjusting or discontinuing medications that may contribute to delirium.
- Treating infections or other medical conditions that could be causing the symptoms.
- Managing pain, dehydration, or nutritional deficiencies effectively.
Tips for Caregivers and Family Members
Caring for someone with delirium can be challenging. Here are some tips to help caregivers and family members:
- Stay calm and patient: Understand that the person with delirium is experiencing confusion and distress.
- Communicate clearly: Use simple words and sentences, and avoid arguing or trying to reason with unreasonable demands.
- Maintain a peaceful environment: Limit visitors and noise to reduce overstimulation.
- Keep a routine: Consistency in daily activities can provide a sense of stability.
- Monitor safety: Implement measures to prevent the patient from falling or injuring themselves.
However, the treatment and management of delirium require a comprehensive approach that addresses both the symptoms and the underlying causes. Medications, when used, should be part of a broader strategy that includes environmental adjustments, supportive care, and, importantly, the involvement of caregivers and family members in the care plan. By understanding these approaches and implementing these tips, caregivers can play a crucial role in the recovery and well-being of individuals experiencing delirium.
Preventing Delirium: Strategies and Interventions
There are effective strategies and lifestyle interventions that can significantly reduce the risk of developing delirium. This guide outlines key measures for preventing delirium, focusing on strategies applicable in hospital settings and lifestyle changes that can make a difference.
Strategies to Reduce the Risk of Delirium
Preventing delirium starts with understanding its triggers, such as infections, dehydration, medication side effects, and sensory impairments. Here are proactive steps to mitigate these risks:
- Regular Medical Check-Ups: Regular health screenings can catch early signs of conditions that might lead to delirium, allowing for prompt treatment.
- Medication Management: Regularly review medications with healthcare providers to avoid those that may contribute to confusion or delirium.
- Stay Hydrated and Nourished: Proper hydration and nutrition are crucial. Dehydration and malnutrition can both trigger delirium.
- Maintain a Healthy Sleep Routine: Disruptions in sleep can exacerbate or lead to delirium. Establishing a regular, restful sleep schedule is essential.
Preventive Measures in Hospital Settings
Hospitals are taking strides to minimize the occurrence of delirium among patients, especially the elderly and those with pre-existing vulnerabilities. Key initiatives include:
- Early Mobilization: Encouraging patients to move and walk around as soon as it’s safe to do so can help maintain physical and cognitive functioning.
- Orientation Aids: Clocks, calendars, and clear signage can help patients maintain a sense of time and place, reducing confusion.
- Minimizing Sleep Disturbances: Hospitals are reducing nighttime disturbances from noise, lights, and medical interventions to promote better sleep.
- Sensory Support: Providing glasses and hearing aids to those who need them helps prevent delirium triggered by sensory impairments.
Lifestyle Changes and Interventions
Lifestyle modifications can play a significant role in preventing delirium, especially for individuals at home or in long-term care facilities. Consider the following interventions:
- Physical Activity: Regular exercise improves overall physical health and can help maintain mental clarity.
- Cognitive Engagement: Activities like puzzles, reading, and social interactions can keep the mind active and reduce the risk of cognitive decline.
- Limit Alcohol and Quit Smoking: Both smoking and excessive alcohol consumption can contribute to delirium and should be avoided.
- Social Connections: Maintaining strong social bonds and engaging in community activities can provide emotional support and mental stimulation, which are vital for mental health.
Implementing these strategies and lifestyle changes can significantly reduce the risk of delirium. It’s important for individuals, caregivers, and healthcare providers to collaborate closely to identify potential risks and take proactive measures to prevent delirium. Awareness and early intervention are key components in safeguarding mental health and ensuring the well-being of those at risk.
FAQs About Delirium Symptoms
What is delirium?
Delirium is a serious disturbance in mental abilities that results in confused thinking and reduced awareness of the environment. It can start suddenly, often within hours or a few days, and can fluctuate during the day.
What are the common symptoms of delirium?
The most recognizable symptoms include sudden confusion, difficulty focusing attention, disorganized thinking, disorientation to time and place, memory problems, hallucinations, and changes in sleep patterns or mood.
How quickly do delirium symptoms appear?
Delirium symptoms can develop over a few hours to a couple of days and often fluctuate throughout the day. It is considered a medical emergency when symptoms appear rapidly.
Can delirium be mistaken for dementia?
Yes, delirium is often mistaken for dementia, especially in elderly patients, but they are different conditions. Delirium develops quickly and is usually temporary, while dementia progresses slowly over months or years and is generally irreversible.
Who is at risk of developing delirium?
People at higher risk include those who are hospitalized, especially in intensive care units or after surgery, the elderly, individuals with previous brain damage or dementia, and those with substance use disorders.
How is delirium treated?
Treatment focuses on addressing the underlying cause. This can involve stopping or changing medications that might be contributing to the confusion, treating infections, correcting metabolic imbalances, and providing supportive care to ensure safety and proper nutrition.
Can delirium be prevented?
Some strategies to reduce the risk of delirium include ensuring proper hydration and nutrition, managing pain, maintaining a regular sleep schedule, and using a minimal amount of sedatives. For hospitalized patients, frequent orientation to the environment and time, and encouraging the presence of familiar objects or people can also help.
Is delirium reversible?
Yes, with prompt and appropriate treatment, many cases of delirium are reversible. The key is to identify and treat the underlying cause(s) of the delirium. Recovery time can vary depending on the health of the individual and the cause of the delirium.
Conclusion
In summary, recognizing the symptoms of delirium and understanding its underlying causes is paramount for the well-being of those affected. Delirium presents with a variety of manifestations, including confusion, altered levels of consciousness, and disorganized thinking, which can be alarming not only to the patient but also to their families and caregivers. Understanding that these symptoms can stem from a wide range of triggers—from infections and medications to dehydration and severe illnesses—is crucial for prompt and accurate diagnosis.
We cannot overemphasize the importance of seeking medical help at the earliest signs of delirium. Early diagnosis and treatment are key to managing the symptoms effectively, mitigating the potential for long-term cognitive effects, and ensuring a quicker recovery. Healthcare professionals can provide a comprehensive assessment to identify the root cause of delirium and tailor a treatment plan that addresses the specific needs of the patient.
If you or someone you know exhibits symptoms of delirium, do not hesitate to seek medical attention. Time is of the essence in these situations, and the sooner a diagnosis can be made, the sooner effective treatment can begin. Let’s prioritize the health and safety of our loved ones by being vigilant about the signs of delirium and advocating for timely medical care.
Remember, delirium is more than just a temporary state of confusion—it is a medical emergency that requires immediate attention. Together, through awareness and prompt action, we can improve outcomes for those affected by this complex condition.