Delirium Treatment: Delirium, a complex condition characterized by sudden changes in brain function, presents a significant challenge in both diagnosis and treatment.
This condition can affect individuals of any age, but it is particularly prevalent among the elderly, especially those in hospital or long-term care settings.
Understanding the nuances of delirium is crucial for healthcare professionals and caregivers alike to ensure effective management and care for those affected.
Understanding Delirium
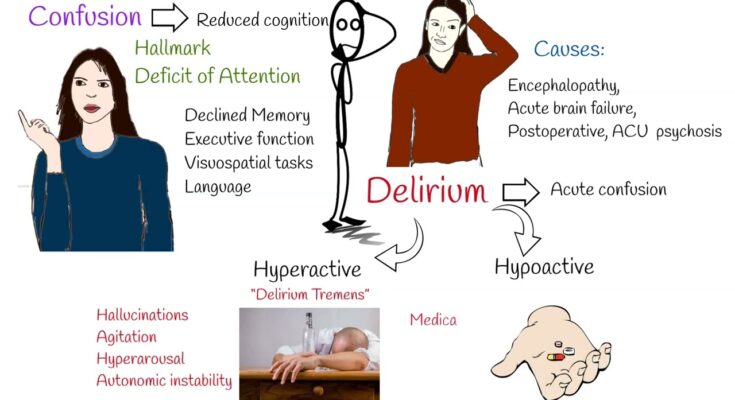
Delirium is a serious disturbance in mental abilities that results in confused thinking and reduced awareness of the environment. The onset of delirium is usually rapid, often occurring within hours or a few days. Delirium can be a frightening experience not only for the person experiencing it but also for those around them. Understanding the symptoms, distinguishing it from similar conditions, and recognizing its causes and risk factors are essential steps in managing and preventing this complex condition.
Symptoms of Delirium
The symptoms of delirium can vary widely from person to person but typically include some or all of the following:
- Confusion and disorientation: Difficulty understanding what is happening around them.
- Memory problems: Especially noticeable with recent events or instructions.
- Difficulty speaking or understanding language: Slurred speech or difficulty in comprehending conversations.
- Changes in alertness: Periods of hyperawareness followed by lethargy.
- Hallucinations and delusions: Seeing, hearing, or believing things that aren’t real.
- Mood swings: Rapid changes in mood, such as from aggression to apathy.
- Sleep disturbances: Difficulty falling asleep or staying asleep, waking up during the night, or sleeping during the day.
Distinction between Delirium and Similar Conditions
Delirium is often confused with dementia, depression, or psychosis due to overlapping symptoms. However, there are key differences:
- Onset: Delirium develops over hours or days, while dementia unfolds over months or years.
- Attention: The ability to stay focused or maintain attention is significantly impaired in delirium, whereas in dementia, this might be less affected in the early stages.
- Reversibility: Delirium is usually reversible with the proper treatment, whereas conditions like dementia are typically irreversible and progressive.
Causes and Risk Factors for Developing Delirium
Delirium can be triggered by a wide array of factors, often related to an underlying medical condition. Some common causes and risk factors include:
- Infections: Particularly urinary tract infections or pneumonia.
- Medication: Adverse reactions to or withdrawal from certain medications.
- Substance abuse: Alcohol or drug intoxication or withdrawal.
- Surgery: Post-operative states, especially in older adults.
- Severe illness or injury: Conditions that significantly affect body function.
- Sensory deprivation: Lack of meaningful sensory input, especially in the elderly.
- Multiple medical problems or medications: Especially in older adults with a history of multiple health issues.
Risk factors that increase the likelihood of developing delirium include advanced age, preexisting brain disorders (such as dementia), and serious medical conditions. Hospitalization, especially in intensive care units, also significantly raises the risk.
However, understanding delirium, its symptoms, how it differs from similar conditions, and the factors that contribute to its development is crucial for early detection and effective management. If you suspect that you or someone you know is experiencing symptoms of delirium, seek medical attention immediately. With prompt and appropriate treatment, it’s possible to manage the symptoms and address the underlying cause, potentially reversing the condition.
Diagnosis of Delirium
Understanding the various diagnostic criteria, assessment tools, and the integral role of healthcare professionals is essential for timely intervention.
Diagnostic Criteria for Delirium
The diagnosis of delirium is primarily clinical, relying on a comprehensive evaluation of the patient’s symptoms and medical history. The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), provides specific criteria for delirium, including:
- A marked change in attention and awareness.
- A rapid onset of symptoms, fluctuating in severity throughout the day.
- Additional disturbance in cognition (e.g., memory deficit, disorientation, language, visuospatial ability, or perception).
- The disturbances are not better explained by another pre-existing, established, or evolving neurocognitive disorder and do not occur in the context of a severely reduced level of arousal, such as coma.
Common Assessment Tools and Tests
Several assessment tools and tests are utilized to support the diagnosis of delirium:
- Confusion Assessment Method (CAM): The most widely used tool for delirium screening, CAM is a structured assessment tool that helps identify the presence of delirium quickly and accurately.
- Delirium Rating Scale (DRS): Used for more detailed assessment, DRS evaluates the severity of delirium symptoms.
- Neuropsychological Tests: These tests assess cognitive functions, including attention, memory, and executive function, to differentiate delirium from other cognitive disorders.
- Laboratory Tests and Imaging: Blood tests, urinalysis, and brain imaging (CT or MRI scans) can help identify underlying causes of delirium, such as infections, metabolic imbalances, or brain injuries.
Role of Healthcare Professionals
The diagnosis of delirium is a collaborative effort involving a multidisciplinary team of healthcare professionals. Physicians, nurses, psychiatrists, and other specialists play a critical role in the assessment process. They conduct thorough clinical evaluations, administer assessment tools, and interpret results to form a comprehensive understanding of the patient’s condition. Their expertise ensures that the diagnosis is accurate, enabling the formulation of an effective treatment plan.
Challenges in Diagnosing Delirium and Overcoming Them
Diagnosing delirium presents several challenges, including its fluctuating symptoms, the presence of coexisting conditions, and variations in its presentation among patients. To overcome these challenges, healthcare professionals should:
- Employ a high index of suspicion, especially in high-risk populations, such as the elderly, critically ill, or postoperative patients.
- Use standardized assessment tools systematically to ensure that no aspect of the condition is overlooked.
- Engage in continuous education and training to stay updated with the latest diagnostic criteria and assessment methods.
- Foster a multidisciplinary approach, ensuring comprehensive care that addresses the multifaceted nature of delirium.
However, the diagnosis of delirium requires a nuanced approach that combines clinical expertise with standardized assessment tools. By understanding the diagnostic criteria, employing effective assessment strategies, and acknowledging the role of healthcare professionals, we can improve the accuracy of delirium diagnoses. Addressing the challenges in diagnosis with a proactive and informed strategy paves the way for better patient outcomes, emphasizing the importance of early detection and intervention in the management of delirium.
Treatment Strategies for Delirium
Treatment strategies encompass both non-pharmacological and pharmacological interventions, with an emphasis on personalized treatment planning to address the unique needs of each patient. This comprehensive approach not only aims to alleviate symptoms but also targets the underlying causes of delirium, ensuring a holistic path to recovery.
Non-pharmacological Interventions for Delirium Treatment
Non-pharmacological strategies play a critical role in the management of delirium, focusing on environmental and supportive measures to reduce confusion and distress. Key interventions include:
- Creating a Supportive Environment: Simplifying patient surroundings to reduce sensory overload can help minimize confusion. This includes ensuring adequate lighting, minimizing noise, and maintaining a calm and comfortable setting.
- Promoting Orientation: Helping patients stay oriented to time, place, and person through verbal reminders, clocks, calendars, and family photos can significantly reduce disorientation.
- Ensuring Proper Hydration and Nutrition: Dehydration and malnutrition can exacerbate delirium symptoms. Providing regular, nutritious meals and encouraging fluid intake are vital.
- Encouraging Mobility: Physical activity, when possible, can enhance recovery by promoting better sleep patterns and reducing the risk of complications associated with prolonged bed rest.
- Enhancing Sleep Hygiene: Establishing regular sleep schedules and minimizing sleep disruptions can help improve sleep quality and contribute to delirium recovery.
Pharmacological Treatments for Delirium
While non-pharmacological measures are the cornerstone of delirium management, pharmacological treatments may be necessary for some patients, especially those experiencing severe symptoms or distress. The choice of medication should be guided by the underlying cause of delirium and patient-specific factors:
- Antipsychotics: Used judiciously for patients with severe agitation or psychosis, antipsychotics can help manage acute symptoms. However, their use should be carefully weighed against potential side effects.
- Cholinesterase Inhibitors: In cases of delirium due to anticholinergic medications or underlying dementia, cholinesterase inhibitors may offer symptomatic relief.
- Benzodiazepines: Primarily used for delirium induced by alcohol withdrawal, benzodiazepines should be used cautiously in other types of delirium due to the risk of worsening confusion.
Personalized Treatment Planning: Tailoring Interventions to Individual Patient Needs
The cornerstone of effective delirium management is a personalized treatment plan that considers the patient’s medical history, current health status, and the specific causes and symptoms of delirium. This tailored approach ensures that both non-pharmacological and pharmacological interventions are optimized to meet the individual needs of the patient, thereby enhancing the effectiveness of the treatment and promoting a quicker recovery. Regular assessment and adjustment of the treatment plan are essential to respond to the evolving needs of the patient throughout their recovery process.
However, a comprehensive and personalized approach to delirium treatment, combining both non-pharmacological and pharmacological strategies, is essential for effective management. By addressing the unique needs of each patient, healthcare providers can improve outcomes, enhance recovery, and significantly impact the overall quality of life for those affected by delirium.
Preventing Delirium: Strategies for At-Risk Populations
Preventing delirium, particularly in at-risk populations, is crucial for maintaining cognitive health and overall well-being. This article explores effective strategies for delirium prevention, emphasizing the importance of early identification and intervention.
Understanding At-Risk Populations
At-risk populations for delirium include elderly patients, especially those undergoing surgical procedures, individuals with pre-existing cognitive impairments, and patients in intensive care units. Recognizing the factors that predispose these groups to delirium is the first step in prevention. These factors often include age, severity of illness, certain medications, and the presence of multiple medical conditions.
Strategies for Prevention
The key to preventing delirium lies in a multi-faceted approach that includes both medical and environmental interventions:
- Early Identification and Assessment: Healthcare providers should assess patients’ risk factors for delirium upon admission and continue monitoring for signs of its onset throughout their care. Tools like the Confusion Assessment Method (CAM) can be invaluable for early detection.
- Optimizing the Environment: Creating a patient-friendly environment can significantly reduce the risk of delirium. This includes ensuring adequate lighting, reducing noise levels, and maintaining a comfortable room temperature. Providing clocks and calendars can also help patients stay oriented to time and place.
- Medication Management: Reviewing and adjusting medications can prevent delirium onset. Avoiding or minimizing the use of delirium-inducing medications, such as certain sedatives and narcotics, is essential.
- Encouraging Mobility and Hydration: Physical activity and proper hydration are vital for preventing delirium. Encouraging patients to move around as much as possible and ensuring they are adequately hydrated can make a significant difference.
- Enhancing Cognitive Engagement: Activities that keep the mind active, such as conversation, reading, or puzzles, can help maintain cognitive function and reduce the risk of delirium.
- Family and Caregiver Involvement: Educating family members and caregivers about the risks and signs of delirium enables them to support preventive measures and seek help promptly if symptoms arise.
The Importance of Early Intervention
Early identification and intervention are paramount in preventing delirium and minimizing its impact. When delirium is recognized promptly, appropriate steps can be taken to address the underlying causes and manage symptoms effectively. This not only improves patient outcomes but can also shorten hospital stays and reduce healthcare costs.
However, preventing delirium in at-risk populations requires a proactive, comprehensive approach. By understanding the factors that contribute to delirium, implementing effective prevention strategies, and emphasizing the importance of early intervention, healthcare providers can significantly improve the quality of care and enhance patient recovery.
Future Directions in Delirium Treatment
The landscape of delirium treatment stands on the brink of significant transformation, driven by groundbreaking research and the advent of innovative technologies. As healthcare professionals and researchers delve deeper into the complexities of delirium, emerging strategies are beginning to reshape our approach to care, promising more effective, personalized, and patient-centered treatments. This section explores the burgeoning frontiers in delirium treatment, highlighting the novel approaches and the potential impact of technology and innovation on the care of patients experiencing delirium.
Emerging Research and Novel Approaches in the Treatment of Delirium
Recent years have witnessed a surge in research dedicated to understanding the multifaceted nature of delirium. This has led to the identification of novel therapeutic targets and the development of innovative treatment modalities. Among these, pharmacological interventions are being refined to minimize adverse effects and maximize efficacy, focusing on the delicate balance of neurotransmitter systems implicated in delirium. Non-pharmacological strategies, too, are gaining traction, emphasizing the importance of environmental modifications, cognitive stimulation, and the implementation of delirium prevention protocols. These approaches underscore a shift towards holistic care, integrating both medical and supportive measures to address the needs of delirium patients comprehensively.
The Potential Impact of Technology and Innovation on Delirium Care
Technology and innovation hold immense promise in revolutionizing delirium care. Digital health applications, such as telemedicine, wearable sensors, and AI-driven diagnostic tools, are at the forefront of this transformation. These technologies offer the potential for early detection and continuous monitoring of delirium signs, enabling timely and targeted interventions. Moreover, AI algorithms can assist in deciphering complex patient data, predicting delirium risk, and personalizing treatment plans. Virtual reality (VR) and augmented reality (AR) technologies are also being explored for their therapeutic potential, offering immersive environments that can aid in cognitive rehabilitation and patient engagement. As these technological solutions evolve, they pave the way for a future where delirium management is more proactive, precise, and patient-friendly.
However, the future of delirium treatment is bright, with emerging research and technological innovations leading the charge towards more effective and humane care. By embracing these novel approaches and harnessing the power of technology, healthcare providers can significantly improve outcomes for patients experiencing delirium, enhancing both the quality of care and the quality of life for this vulnerable population. As we move forward, it is imperative that we continue to support and invest in research and innovation, ensuring that the promise of today becomes the reality of tomorrow in delirium care.
Conclusion
The importance of an integrated approach in the treatment of delirium shines through as a beacon for healthcare professionals. It’s clear that managing delirium extends beyond mere symptom control. It necessitates a holistic strategy that addresses the root causes, involves multidisciplinary care teams, and includes both pharmacological and non-pharmacological interventions. Personalized care plans that consider the patient’s medical history, current health status, and the specific contributors to their delirium are crucial for successful outcomes.
Moreover, the discussion underscored the significance of preventive measures and early intervention. Recognizing at-risk individuals, implementing strategies to mitigate known risk factors, and educating healthcare providers, patients, and families about delirium can profoundly impact the prevention and management of this complex condition.
In conclusion, tackling delirium requires a comprehensive and integrated approach. By combining accurate diagnosis, targeted treatment, and preventive strategies, healthcare professionals can significantly improve the quality of life for patients affected by delirium. This collaborative effort not only aids in the immediate resolution of delirium episodes but also contributes to the long-term health and well-being of patients, underscoring the necessity of an integrated care model in addressing this challenging medical syndrome.