Cushing Syndrome Symptoms: Cushing Syndrome is a complex endocrine condition that poses significant health risks if left untreated.
This article delves deep into the symptoms and causes of Cushing Syndrome, offering comprehensive insights to enhance awareness and understanding of this medical condition.
What is Cushing Syndrome
Cushing Syndrome is a medical condition that occurs when your body is exposed to high levels of the hormone cortisol for an extended period. Often the result of taking glucocorticoid drugs, this condition can also stem from your body making too much cortisol on its own. Cortisol plays a variety of roles in the body, including regulating metabolism, reducing inflammation, and controlling the sleep-wake cycle. However, too much cortisol can lead to a range of health issues, making Cushing Syndrome a condition that requires careful management and treatment.
The Role of Cortisol in the Body
Cortisol, often referred to as the “stress hormone,” is vital for many functions in the body. It helps manage how your body uses carbohydrates, fats, and proteins. It also keeps inflammation down, regulates blood pressure, increases blood sugar (glucose), and can assist in controlling the sleep cycle. Produced by the adrenal glands located at the top of each kidney, cortisol’s production is finely tuned by the needs of the body, making it a crucial component of your body’s response to stress.
How Cushing Syndrome Affects the Body’s Cortisol Levels
Cushing Syndrome significantly impacts the body’s normal levels of cortisol, leading to an overabundance of this hormone. This imbalance can result from the body’s adrenal glands producing too much cortisol or through the prolonged use of corticosteroid medications, which are often prescribed for conditions like asthma, rheumatoid arthritis, and lupus. The excess cortisol in the body can lead to a variety of symptoms and health issues, including weight gain, particularly around the midsection and upper back; pink or purple stretch marks; thinning, fragile skin that bruises easily; a rounded face; and high blood pressure. Additionally, Cushing Syndrome can affect mood and cognitive functions, leading to emotional instability and difficulties with memory and concentration.
By understanding the role of cortisol in the body and how Cushing Syndrome disrupts this balance, individuals and healthcare providers can better recognize the symptoms and seek appropriate treatment. Managing cortisol levels is crucial for maintaining overall health and wellbeing, highlighting the importance of diagnosing and treating Cushing Syndrome effectively.
Symptoms of Cushing Syndrome
These symptoms can vary significantly among individuals, making the condition challenging to diagnose early. This article outlines the major symptoms of Cushing Syndrome, with a special focus on psychological and emotional symptoms, highlighting the variability of symptoms among individuals.
Major Symptoms
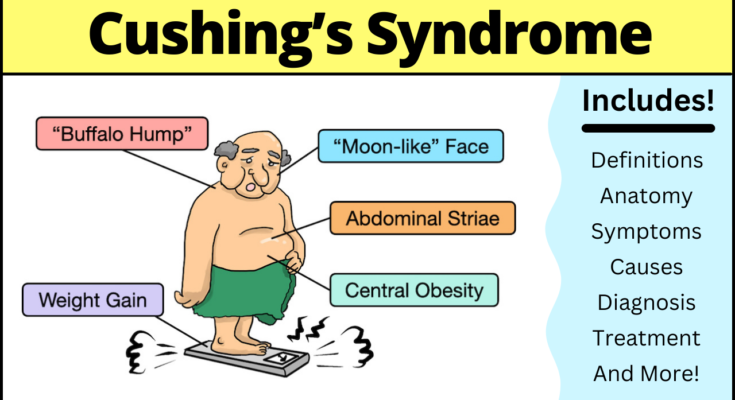
Cushing Syndrome manifests through several distinct physical signs. The most recognizable among these include:
- Weight Gain: Particularly around the midsection and upper back, despite no significant changes in diet or exercise routine.
- Round Face: Often described as a “moon face,” due to significant facial fat.
- Skin Changes: Thinning of the skin, easy bruising, and the appearance of purple or pink stretch marks, primarily on the abdomen, thighs, buttocks, arms, and breasts.
- Muscle Weakness: Progressive and noticeable weakness, especially in the thighs, making it difficult to rise from a sitting position.
- Bone Loss: Leading to an increased risk of fractures, particularly in the spine and ribs.
- High Blood Pressure: Can occur independently or as part of metabolic syndrome.
- Glucose Intolerance: Including prediabetes or diabetes, due to the effect of cortisol on blood sugar regulation.
Psychological and Emotional Symptoms
The psychological and emotional symptoms of Cushing Syndrome are as significant as the physical ones but can often be overlooked. These include:
- Mood Swings: Patients may experience significant fluctuations in mood, from euphoria to deep depression.
- Irritability: A short temper or irritability with little to no provocation.
- Anxiety: General feelings of anxiety, restlessness, or feelings of being overwhelmed.
- Cognitive Difficulties: Including memory impairment, difficulty concentrating, or a general feeling of mental fog.
- Depression: Clinical depression is common and can be severe, necessitating professional intervention.
Highlighting the Variability of Symptoms
The symptoms of Cushing Syndrome can vary widely among individuals. Some people may exhibit only a few mild symptoms, while others may experience a broad spectrum of severe symptoms. The variability can depend on the duration and extent of cortisol overexposure. It’s also worth noting that symptoms like weight gain, mood swings, and high blood pressure are common in the general population, making it even more challenging to pinpoint Cushing Syndrome without a thorough medical evaluation.
Understanding this variability is crucial, both for medical professionals in making a diagnosis and for patients in recognizing the need for a medical assessment. Early diagnosis and treatment can mitigate the long-term effects of the syndrome, emphasizing the importance of awareness and education on this condition.
However, Cushing Syndrome is a complex condition with a broad range of symptoms affecting both the body and the mind. Its variability among individuals necessitates a comprehensive approach to diagnosis and treatment. Awareness of both the physical and psychological symptoms is essential for early detection and effective management of this condition.
Causes of Cushing Syndrome
Understanding these causes is crucial for diagnosis and treatment. In this article, we will explore the different triggers of Cushing Syndrome, including the use of oral corticosteroid medication, the body’s overproduction of cortisol, pituitary adenomas, ectopic ACTH syndrome, adrenal tumors, and the role of familial predispositions and rare cases.
Exogenous Causes: The Role of Corticosteroid Medication
Exogenous causes of Cushing Syndrome primarily involve the external introduction of corticosteroids into the body. This is often the result of medical treatment with oral corticosteroid medication, which is prescribed for a variety of conditions such as asthma, rheumatoid arthritis, and lupus. While these medications are effective for managing inflammation and immune responses, prolonged use or high doses can lead to an excess of cortisol, mimicking the symptoms of Cushing Syndrome.
Endogenous Causes: The Body’s Overproduction of Cortisol
Contrary to exogenous causes, endogenous causes of Cushing Syndrome arise from the body’s own overproduction of cortisol. This overproduction can be attributed to several conditions, including:
- Pituitary Adenomas (Cushing’s Disease): The most common endogenous cause, pituitary adenomas are benign tumors of the pituitary gland that produce an excess of ACTH (Adrenocorticotropic Hormone), which in turn stimulates the adrenal glands to produce more cortisol.
- Ectopic ACTH Syndrome: This condition occurs when a tumor outside the pituitary gland produces ACTH. These tumors are often found in the lungs, thyroid, or pancreas, leading to the overstimulation of the adrenal glands.
- Adrenal Tumors: Tumors located directly on the adrenal glands can lead to an overproduction of cortisol, independent of ACTH stimulation. These tumors can be either benign (adenomas) or malignant (cancerous).
Familial Predispositions and Rare Cases
In some instances, Cushing Syndrome can result from familial predispositions, indicating a genetic component to the condition. Families with a history of endocrine tumors may be at a higher risk of developing Cushing Syndrome. Additionally, rare causes such as ectopic secretion of CRH (Corticotropin-Releasing Hormone) or familial cases of multiple endocrine neoplasia (MEN1) can also trigger the syndrome.
If you suspect you have symptoms of Cushing Syndrome, it’s important to consult with a healthcare professional for appropriate testing and treatment options. Awareness and education about the causes of Cushing Syndrome can lead to early detection and improved outcomes for those affected by this condition.
Diagnosis of Cushing Syndrome
Here, we delve into the primary diagnostic tests for Cushing Syndrome and highlight the crucial role of endocrinologists in both diagnosis and treatment.
Diagnostic Tests for Cushing Syndrome
The journey to diagnosing Cushing Syndrome begins with a detailed evaluation of symptoms, followed by specific diagnostic tests designed to measure cortisol levels in the body. These tests are critical in distinguishing Cushing Syndrome from other conditions that share similar signs and symptoms. The primary diagnostic tests include:
- Blood Tests: These are essential for measuring cortisol levels in the bloodstream. The most common blood test is the dexamethasone suppression test, which evaluates how your cortisol levels respond to an administered steroid.
- Urine Tests: 24-hour urinary free cortisol test involves collecting all urine for 24 hours to measure the amount of cortisol. This test helps in confirming elevated cortisol levels over an extended period.
- Saliva Tests: Late-night salivary cortisol test measures cortisol levels in the saliva at night when they are typically low. Elevated levels may indicate Cushing Syndrome.
- Imaging Tests: Imaging tests such as MRI (Magnetic Resonance Imaging) and CT (Computed Tomography) scans are used to identify any abnormalities in the adrenal glands, pituitary gland, or elsewhere that may be causing increased cortisol production.
The Role of Endocrinologists in Diagnosis and Treatment
Endocrinologists, specialists in hormone-related disorders, play a pivotal role in both the diagnosis and management of Cushing Syndrome. Their expertise is crucial in:
- Interpreting Test Results: Endocrinologists possess the specialized knowledge required to accurately interpret the results of the aforementioned tests, differentiating Cushing Syndrome from conditions with similar symptoms.
- Developing a Treatment Plan: Once a diagnosis is confirmed, endocrinologists are instrumental in crafting a tailored treatment plan. This may involve medication to control cortisol production, surgery to remove tumors, or radiation therapy in certain cases.
- Long-term Management: Cushing Syndrome can have lasting effects on the body. Endocrinologists provide ongoing care to manage these effects, adjust treatments as necessary, and monitor for potential recurrences.
However, diagnosing Cushing Syndrome is a meticulous process that necessitates a range of diagnostic tests to accurately measure cortisol levels in the body. The expertise of endocrinologists is invaluable, not only in confirming the diagnosis but also in providing comprehensive treatment and management plans tailored to the needs of each individual. With their guidance, patients can navigate the complexities of Cushing Syndrome and embark on a path toward recovery and better health.
Treatment Options for Cushing Syndrome
There are several effective treatment options available, each tailored to the underlying cause of the condition. These treatments range from surgery and radiation therapy to medication, as well as lifestyle and home remedies designed to manage symptoms and improve quality of life. Understanding these options can empower patients and caregivers to make informed decisions about their health care.
Surgery (For Tumors)
Surgery is often the first line of treatment for Cushing Syndrome when the condition is caused by tumors. For those with adrenal gland tumors, surgical removal of the affected gland can effectively cure the condition. In cases where a pituitary adenoma is the culprit, removing the tumor through an operation can significantly reduce cortisol levels. Surgical interventions require a skilled medical team and a thorough pre-surgical evaluation to ensure the best outcomes.
Radiation Therapy (For Pituitary Adenomas)
When surgery is not viable or fails to remove all of a pituitary tumor, radiation therapy may be employed as a secondary treatment option. This approach involves directing precise radiation beams at the tumor, gradually shrinking it over time. Although effective, radiation therapy for pituitary adenomas is a slower process and may take several months to show results. It’s typically considered when surgery isn’t possible or as an adjunct to surgical treatment.
Medication (To Control Cortisol Production or Effects)
Medications play a crucial role in managing Cushing Syndrome, especially for individuals who cannot undergo surgery. These drugs can either reduce the production of cortisol or mitigate its effects on the body. Examples include ketoconazole, metyrapone, and etomidate, which inhibit cortisol production, and mifepristone, which blocks cortisol’s action on tissues. Medication regimes require close monitoring by healthcare professionals to avoid side effects and ensure effectiveness.
Lifestyle and Home Remedies
In addition to medical treatments, incorporating lifestyle changes and home remedies can significantly improve symptoms and overall well-being. Managing stress through techniques such as meditation, yoga, or counseling can help control cortisol levels naturally. A healthy diet, rich in fruits, vegetables, and whole grains, supports overall health, while regular physical activity can combat weight gain, muscle weakness, and bone density loss associated with Cushing Syndrome. These lifestyle modifications not only complement medical treatments but also enhance recovery and quality of life.
Living with Cushing Syndrome: A Comprehensive Guide
Living with Cushing Syndrome presents unique challenges that necessitate a well-rounded approach to health and well-being. This condition, characterized by an excess of the hormone cortisol, affects various aspects of physical and mental health. Managing symptoms, navigating treatment side effects, and ensuring long-term health are crucial aspects of living with this syndrome. Equally important is finding the right support and coping strategies to maintain a high quality of life. This guide aims to provide practical advice and resources for individuals living with Cushing Syndrome.
Managing Symptoms and Side Effects of Treatment
Cushing Syndrome symptoms can range from weight gain and muscle weakness to high blood pressure and skin changes. Treatment often involves medication, surgery, or radiation therapy, each with potential side effects. It’s essential to work closely with your healthcare provider to:
- Adjust medications to minimize side effects while effectively managing the condition.
- Incorporate a balanced diet and exercise regimen to combat weight gain and strengthen muscles without overexertion.
- Monitor blood sugar and blood pressure levels regularly, as Cushing Syndrome can increase the risk of diabetes and hypertension.
Staying informed about your treatment options and potential side effects can empower you to make decisions that best suit your health needs.
Long-term Monitoring and Health Maintenance
Long-term health maintenance for individuals with Cushing Syndrome involves regular check-ups and monitoring to prevent complications. Key aspects include:
- Routine tests to monitor cortisol levels and assess the effectiveness of treatment.
- Regular screenings for osteoporosis, diabetes, and cardiovascular disease, which are common complications associated with Cushing Syndrome.
- Lifestyle adjustments to mitigate risk factors, such as adopting a heart-healthy diet, engaging in regular physical activity, and quitting smoking.
Establishing a proactive approach to health maintenance can significantly improve your long-term prognosis and quality of life.
Support Resources and Coping Strategies
Living with Cushing Syndrome can be emotionally and physically demanding. Finding support and employing coping strategies are vital for mental health and well-being:
- Join support groups either in-person or online to connect with others who understand the challenges of living with Cushing Syndrome.
- Seek professional mental health support if you’re struggling with anxiety, depression, or stress related to your condition.
- Develop stress management techniques, such as mindfulness, meditation, or yoga, which can help in managing cortisol levels and improving overall well-being.
Accessing resources and developing strategies to cope with the emotional and physical demands of Cushing Syndrome is essential for living a balanced and fulfilling life.
FAQ Section on Cushing Syndrome
What is Cushing Syndrome?
Cushing Syndrome is a hormonal disorder caused by prolonged exposure of the body’s tissues to high levels of the hormone cortisol. This can result from taking glucocorticoid drugs or by tumors that produce cortisol or adrenocorticotropic hormone (ACTH).
What causes Cushing Syndrome?
The most common cause of Cushing Syndrome is the use of oral corticosteroid medication. The condition can also be caused by tumors on the pituitary or adrenal glands, or elsewhere in the body, which produce cortisol or ACTH.
What are the symptoms of Cushing Syndrome?
Symptoms of Cushing Syndrome can vary but often include weight gain, especially in the upper body; a rounded face; increased fat around the neck; thinning skin; easy bruising; and purple stretch marks. Fatigue, weakness, high blood pressure, and high blood sugar levels are also common.
How is Cushing Syndrome diagnosed?
Diagnosing Cushing Syndrome usually involves a review of medical history, physical examination, and laboratory tests to measure cortisol levels in the urine, saliva, or blood. Imaging tests may also be used to find abnormalities in the adrenal or pituitary glands.
Can Cushing Syndrome be cured?
Yes, Cushing Syndrome can often be cured with proper treatment, which depends on the underlying cause. Treatment options may include surgery, radiation, medication, or reducing the use of corticosteroid medications.
Is Cushing Syndrome common?
Cushing Syndrome is considered rare. It most commonly affects adults aged 20 to 50 and is more prevalent in females than in males.
What are the complications of Cushing Syndrome?
If left untreated, Cushing Syndrome can lead to serious complications such as osteoporosis, hypertension, type 2 diabetes, infections, and increased risk of blood clots.
How can I manage Cushing Syndrome?
Management of Cushing Syndrome includes treatment of the underlying cause, lifestyle adjustments to manage symptoms and complications, and regular follow-ups with your healthcare provider to monitor the condition and response to treatment.
Is there a way to prevent Cushing Syndrome?
Preventing Cushing Syndrome involves using corticosteroid medications responsibly and only as prescribed by a healthcare provider. Regular check-ups are important for detecting any health changes that could indicate Cushing Syndrome, especially for individuals at higher risk.
Can lifestyle changes help with Cushing Syndrome?
While lifestyle changes cannot cure Cushing Syndrome, they can help manage symptoms and improve quality of life. This includes adopting a healthy diet, engaging in regular physical activity, managing stress, and avoiding tobacco and excessive alcohol use.
Conclusion:
The importance of early detection and treatment of Cushing Syndrome cannot be overstated. Identifying the condition in its nascent stages can significantly mitigate the risk of long-term health complications, enhancing the quality of life for those affected. Early intervention enables more effective management strategies, including surgery, medication, and lifestyle adjustments, which can lead to a better prognosis and reduce the risk of irreversible damage to the body.
We strongly encourage anyone who recognizes the symptoms of Cushing Syndrome in themselves or loved ones to seek medical advice without delay. Consulting with a healthcare professional can lead to early diagnosis and treatment, which are pivotal in managing the condition effectively. Healthcare providers can offer comprehensive care plans tailored to individual needs, ensuring the best possible outcomes.
In conclusion, awareness and understanding of Cushing Syndrome are vital. Recognizing the signs early and seeking professional medical advice can make a significant difference in treatment success. Let this article serve as a reminder of the power of informed action and the importance of prioritizing your health. Remember, the sooner Cushing Syndrome is detected, the more effective the treatment can be, offering a hopeful outlook for those affected.