Croup Treatment: Croup is a common respiratory condition that primarily affects young children, characterized by a distinctive barking cough, stridor, and often, difficulty breathing.
Prompt recognition and effective treatment are crucial to managing this condition and preventing complications.
This article provides a comprehensive overview of the diagnosis and treatment options for croup, aiming to offer valuable insights for caregivers and healthcare professionals alike.
What is Croup?
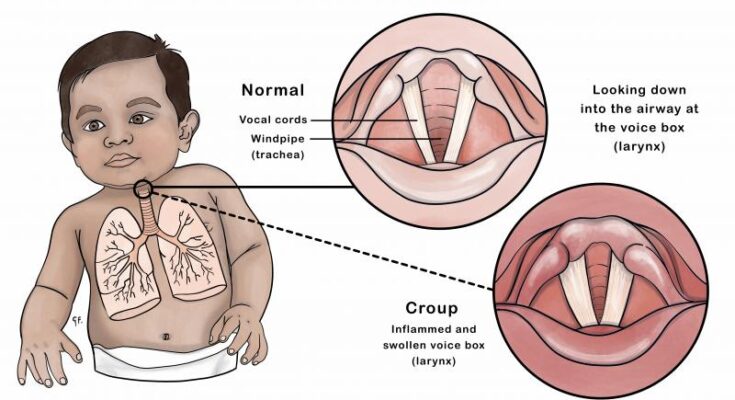
Croup is a common respiratory condition primarily affecting young children. It is characterized by a distinctive barking cough, often compared to the sound of a seal. This condition results from inflammation and swelling around the vocal cords, windpipe, and bronchial tubes. Croup can cause difficulties in breathing and is typically caused by viral infections.
Causes of Croup and Its Effects on the Respiratory System
Croup is most commonly triggered by viral infections, particularly the parainfluenza virus. However, other viruses and, in rare cases, bacteria can also cause croup. These pathogens lead to inflammation of the larynx, trachea, and bronchi, resulting in the symptoms associated with croup.
The swelling in these areas makes the airway narrower, which can make breathing difficult. This is particularly problematic in young children, whose airways are smaller and more easily obstructed. In severe cases, croup can lead to significant breathing difficulties, requiring immediate medical intervention.
Key Statistics: Incidence Rates and Age Groups Most Commonly Affected
Croup is most prevalent in children between the ages of 6 months and 3 years, with a peak incidence at 2 years of age. While it can occur in older children and, very rarely, adults, the condition is most commonly a pediatric issue. Each year, a significant number of young children are seen in emergency departments for croup, which tends to be more common during the fall and winter months.
The incidence of croup varies globally, but it is a leading cause of respiratory tract infections in children. Despite its frequency, severe complications are relatively rare, thanks to effective treatment options. Most children with croup can be cared for at home, with only the most severe cases requiring hospitalization.
Recognizing the Symptoms of Croup
Understanding the symptoms of croup, how they differ from other respiratory illnesses, and knowing when to seek medical attention is crucial for parents and caregivers. This guide provides a comprehensive overview of croup symptoms, differentiating factors, and guidelines for seeking medical help.
Detailed Description of Croup Symptoms
Croup symptoms are often noticeable and can include the following:
- Distinctive Barking Cough: The most recognizable sign of croup is a cough that resembles the barking of a seal. This unique sound is due to swelling around the voice box, windpipe, and bronchial tubes.
- Hoarse Voice: Swelling in the voice box can cause the child’s voice to sound hoarse or muffled.
- Stridor: This is a high-pitched wheezing sound heard when the child breathes in. It indicates that the airway is narrowed, making it harder to breathe.
- Breathing Difficulties: The child may show signs of labored breathing, such as fast breathing, flaring nostrils, or the skin between the ribs pulling in with each breath.
Differentiating Croup from Other Respiratory Illnesses
Croup can be confused with other respiratory conditions, but certain features help differentiate it:
- Timing: Croup symptoms, particularly the cough, often worsen at night.
- Age Group: Croup primarily affects young children between the ages of 6 months and 3 years. While other respiratory illnesses can affect all age groups, the distinctive barking cough of croup is more common in toddlers.
- Onset: Croup symptoms can develop suddenly, often after a few days of mild cold symptoms, which is less common in conditions like bronchitis or pneumonia.
When to Seek Medical Attention for Croup Symptoms
While croup can often be managed at home, certain symptoms warrant immediate medical attention:
- Difficulty Breathing: If the child is struggling to breathe, has rapid breathing, or shows signs of oxygen deprivation (like bluish lips), seek emergency care.
- Persistent Stridor at Rest: If the high-pitched wheezing is present even when the child is calm and not crying, it’s a sign of severe airway narrowing.
- Dehydration: Signs include fewer wet diapers, dry mouth, or lethargy due to difficulty in swallowing.
- High Fever: Though croup itself can cause a mild fever, a high fever could indicate a secondary infection.
Early intervention can prevent complications and ensure a quicker recovery for the child. If in doubt, it’s always best to consult with a healthcare provider for personalized advice and treatment options.
Diagnosis of Croup: Methods and Importance
Diagnosing croup accurately is critical for implementing effective treatment and ensuring a swift recovery. Here, we delve into how healthcare providers diagnose croup, the role of imaging and lab tests, and why precise diagnosis is crucial.
How Healthcare Providers Diagnose Croup
The diagnosis of croup is predominantly clinical, based on a combination of medical history and physical examination. Healthcare providers look for the hallmark symptoms of croup:
- A barking cough that often sounds like a seal’s bark.
- Stridor, a high-pitched wheezing noise that occurs when breathing in.
- Hoarseness and difficulty breathing in more severe cases.
Medical professionals pay close attention to the child’s medical history, including the onset and duration of symptoms. Information on recent exposures to colds or other respiratory infections is also valuable, as these can precede croup.
The Role of Imaging and Lab Tests
While the diagnosis of croup is mainly clinical, imaging and lab tests may be employed in ambiguous cases or when complications are suspected. Radiographic imaging, such as a neck X-ray, can be helpful. A characteristic finding in croup is the “steeple sign” on a lateral neck X-ray, which shows a narrowing of the upper airway that resembles a church steeple. This feature, however, is not present in all cases of croup.
Lab tests are not routinely used for diagnosing croup but may be necessary if bacterial infection or other conditions (like epiglottitis) need to be ruled out. In these instances, a complete blood count (CBC) or cultures from throat swabs might be considered to identify the specific causative agent.
Discussing the Importance of Accurate Diagnosis
An accurate diagnosis of croup is essential for several reasons. Primarily, it enables healthcare providers to implement the most effective treatment strategies, such as corticosteroids for reducing airway swelling and nebulized epinephrine for severe cases. Additionally, distinguishing croup from more serious conditions like epiglottitis is critical for preventing potential complications.
Early and precise diagnosis also allows for appropriate home care advice and, when necessary, hospital admission for children who may need closer monitoring or additional treatments. Furthermore, understanding the viral nature of most croup cases can help manage expectations regarding the course of the illness and the use of antibiotics, which are not effective against viral infections.
However, diagnosing croup accurately is a cornerstone of pediatric healthcare, ensuring that children receive prompt, appropriate care. Through clinical examination and, when needed, the judicious use of imaging and lab tests, healthcare providers can distinguish croup from other conditions, guiding families towards effective treatments and supportive care.
Treatment Options for Croup
The primary objectives in treating croup are to alleviate symptoms, ensure the child can breathe easily, and prevent complications. Treatment approaches vary from simple home remedies to medical interventions, depending on symptom severity. Mild cases often resolve with home care, while severe instances may require medical attention. The overarching goal is to provide comfort and support to the affected child, ensuring a smooth recovery.
Home Care Strategies and Remedies for Managing Mild Croup Symptoms
For mild croup, home care strategies play a crucial role in managing symptoms. Key remedies include:
- Humidified Air: Using a cool-mist humidifier in the child’s room can help soothe inflamed airways.
- Hydration: Encouraging the child to drink plenty of fluids aids in keeping the airways moist and reduces the viscosity of mucus.
- Comforting Presence: Keeping the child calm and comfortable is vital, as crying can exacerbate breathing difficulties.
- Positioning: Keeping the child in an upright position can help ease breathing.
These strategies can significantly alleviate mild symptoms of croup, promoting a quicker recovery without the need for medical intervention.
Medical Treatments for Severe Croup Cases: Medications, Steroids, and Hospitalization Criteria
Severe cases of croup may necessitate medical treatment to prevent complications. Options include:
- Steroids: Medications like dexamethasone can reduce airway inflammation, improving breathing.
- Nebulized Epinephrine: In emergency situations, this can relieve airway swelling rapidly.
- Hospitalization: Indicated if the child exhibits severe breathing difficulties, dehydration, or requires more intensive treatment.
The decision to escalate treatment is based on the child’s response to initial management and the severity of symptoms. Healthcare providers may use specific criteria, including the child’s breathing rate, oxygen levels, and overall distress level, to determine the need for hospitalization.
The Importance of Hydration and Rest in Croup Recovery
Hydration and rest are fundamental to the recovery process from croup. Adequate fluid intake ensures the mucus remains thin and easier to cough up, while rest helps the body heal. Parents and caregivers should monitor the child’s fluid intake and encourage restful activities, avoiding overexertion during the recovery period.
However, managing croup effectively requires a comprehensive approach tailored to the severity of the symptoms. Home care remedies are often sufficient for mild cases, but severe symptoms may necessitate medical intervention. Regardless of the severity, hydration and rest are critical components of the recovery process. Understanding these treatment options empowers parents and caregivers to provide the best care for their child, ensuring a swift and smooth recovery from croup.
Medications Used in Croup Treatment: An In-depth Guide
This guide delves into the medications frequently prescribed for croup, covering their dosages, purposes, benefits, and potential side effects. Additionally, we offer advice on the use of over-the-counter (OTC) medications and highlight when it’s crucial to consult a healthcare provider.
Commonly Prescribed Medications for Croup
- Corticosteroids: Corticosteroids, such as dexamethasone or prednisolone, are the cornerstone of croup treatment. They reduce inflammation in the airways, making breathing easier. Dosage varies depending on the severity of symptoms but is typically a single dose administered orally.
- Nebulized Epinephrine: In more severe cases, nebulized epinephrine may be used. This medication works by shrinking the swollen tissues in the throat, providing quick relief. It’s usually administered in a hospital setting due to the potential for side effects.
Benefits and Potential Side Effects
- Corticosteroids offer significant benefits in reducing croup symptoms. They can decrease the need for additional medical treatment and hospitalization. However, side effects are minimal due to the low dosage and short course of treatment, but may include mood changes, increased appetite, and stomach upset.
- Nebulized Epinephrine provides rapid relief in severe cases, but its effects are temporary. Side effects can include rapid heartbeat, increased blood pressure, and restlessness. Therefore, its use is closely monitored in a clinical setting.
Guidance on Over-the-Counter Medications
OTC medications can play a role in managing mild croup symptoms. However, it’s important to use them judiciously:
- Pain Relievers: Acetaminophen or ibuprofen can help reduce fever and discomfort associated with croup. Always adhere to the recommended dosages based on the child’s age and weight.
- Cough Syrups and Cold Medicines: Generally, these are not recommended for children under 6 years of age due to a lack of evidence on their effectiveness and potential for harm.
- Humidifiers: Running a cool mist humidifier in the child’s room can help soothe irritated airways and make breathing easier.
When to Consult a Healthcare Provider
While mild cases of croup can often be managed at home, it’s vital to know when to seek professional advice. Consult a healthcare provider if your child:
- Exhibits difficulty breathing or shows signs of respiratory distress.
- Has a high fever or symptoms that persist for more than a few days.
- Is under 3 months old and has symptoms of croup.
- Exhibits signs of dehydration, such as reduced urination, dry mouth, or lethargy.
While OTC medications can support treatment, recognizing when professional medical advice is needed can ensure the best outcomes for your child. Always consult with a healthcare provider before starting or changing any medication regimen for croup.
Preventing Croup and Complications
Understanding prevention and early recognition of complications is key to managing the condition effectively. Here’s how you can prevent the spread of viruses that cause croup, recognize complications, and know when it’s time to follow up with a healthcare provider.
Tips for Preventing the Spread of Viruses That Cause Croup
- Practice Good Hygiene: Regular handwashing with soap and water for at least 20 seconds can significantly reduce the spread of viruses. It’s particularly important after coughing, sneezing, or blowing your nose.
- Cover Coughs and Sneezes: Teach children to cough or sneeze into a tissue or their elbow, not their hands. This practice helps contain the spread of virus particles.
- Clean and Disinfect: Frequently touched surfaces like toys, doorknobs, and mobile devices should be regularly cleaned and disinfected.
- Avoid Close Contact: Try to avoid close contact with sick individuals, especially during croup season, typically fall and winter.
- Stay Home When Sick: Keeping children home from school or daycare when they are sick can prevent the spread of the virus to others.
Recognizing Complications Associated with Croup and How to Prevent Them
While croup is usually mild, it can lead to complications such as bacterial infections, pneumonia, or severe breathing difficulties. Here’s how to recognize and prevent these complications:
- Watch for Worsening Symptoms: Difficulty breathing, a high fever, or a persistent cough that gets worse instead of better should prompt immediate medical attention.
- Ensure Proper Hydration: Keeping your child well-hydrated is crucial. Fluids can help thin mucus and ease breathing.
- Use a Cool-Mist Humidifier: This can help keep your child’s airways moist and reduce the severity of coughing spells.
- Avoid Smoke Exposure: Smoke can aggravate symptoms. Keep your child away from cigarette smoke and other irritants.
When to Follow Up with a Healthcare Provider After a Croup Diagnosis
It’s essential to monitor your child’s symptoms and know when to seek further medical advice. Follow up with a healthcare provider if:
- Symptoms Persist or Worsen: If symptoms do not improve with home treatment or if they worsen after initial improvement, it’s time to see a doctor.
- Breathing Difficulties: Any sign of labored breathing, wheezing, or stridor (a high-pitched breathing sound) warrants immediate medical attention.
- Dehydration Signs: If your child is not urinating as frequently as usual, has a dry mouth, or is less tearful when crying, these could be signs of dehydration and require a doctor’s evaluation.
- Fever: A high fever or a fever that persists for more than a few days should be evaluated by a healthcare provider.
Prevention and early detection are key to managing croup effectively. By following these guidelines, you can help minimize the spread of the virus and identify any complications early, ensuring your child remains healthy and comfortable.
FAQs About Croup Treatment
What is the best way to treat croup at home?
For mild cases of croup, several home remedies can help alleviate symptoms:
- Keep your child comfortable: Ensure they are resting and staying well-hydrated. Offer them their favorite soothing drinks like warm broth or cold fluids.
- Humidified air: Use a cool-mist humidifier in your child’s room to keep the air moist, which can help ease breathing. Alternatively, taking your child into a steamy bathroom for a few minutes can have a similar effect.
- Stay calm: Children can become anxious when they have difficulty breathing, so it’s important to remain calm and reassuring.
When should I seek medical attention for croup?
You should seek medical attention if your child:
- Has difficulty breathing or shows signs of increased effort to breathe (e.g., fast breathing, straining muscles around the ribs).
- Exhibits a high fever (above 38.5°C or 101.3°F).
- Has symptoms that worsen or do not improve with home treatment.
- Shows signs of dehydration, such as reduced urination, dry mouth, or lethargy.
Can over-the-counter medications help with croup?
Over-the-counter (OTC) fever reducers like acetaminophen or ibuprofen can be used to manage fever and discomfort associated with croup. However, cough suppressants are generally not recommended for treating the cough from croup, as the coughing helps to keep the airway clear. Always consult with a healthcare provider before giving any medication to your child.
Is there a specific diet recommended for a child with croup?
While there’s no specific diet for treating croup, encouraging fluid intake is crucial to prevent dehydration. Warm fluids might help soothe the throat, while cold fluids can provide relief from the throat irritation. Avoid giving very spicy or acidic foods that could further irritate the throat.
How can I prevent my child from getting croup?
Croup is often caused by viral infections, so the best prevention methods include general illness prevention strategies:
- Encourage regular handwashing with soap and water.
- Teach your child to cover their mouth and nose when coughing or sneezing.
- Avoid close contact with sick individuals when possible.
- Keep your child’s vaccinations up to date, as some vaccines can help prevent infections that might lead to croup.
Can adults get croup?
While croup is most common in children aged 6 months to 3 years, adults can occasionally get an infection that causes similar symptoms. However, it’s rare and usually less severe because the airways are larger and less susceptible to obstruction.
Conclusion:
For parents and guardians, the journey through your child’s episode of croup can be daunting. However, armed with the right knowledge and resources, you can navigate this challenge with greater confidence. Remember, early recognition of croup’s hallmark signs—such as the distinctive barking cough and stridor—plays a pivotal role in ensuring your child receives the care they need without delay.
Encouragement is extended to all parents to actively engage with healthcare providers when it comes to your child’s health. Consulting with professionals offers you personalized advice and treatment plans tailored to your child’s specific situation. Healthcare providers can guide you through the intricacies of croup, from distinguishing its symptoms to understanding the best course of action for treatment and recovery.
Moreover, fostering a partnership with your child’s medical team empowers you to make informed decisions, ensuring your child’s swift return to health and well-being. It’s through this collaborative approach that you can provide the best support for your child, ensuring they overcome croup with minimal discomfort and risk.
In summary, while croup is a condition that necessitates prompt attention, it is manageable with the right approach and resources. By staying informed, recognizing the early signs, and seeking professional guidance, parents can effectively steer their children through the recovery process. Let this be a call to action: embrace the importance of proactive healthcare engagement, ensuring your child’s health and happiness are always at the forefront.