Creutzfeldt-Jakob Disease Treatment: Creutzfeldt-Jakob Disease (CJD) stands as a rare, degenerative, invariably fatal brain disorder, affecting one in every million people per annum worldwide.
This article delves deeply into the facets of CJD, providing essential insights into its diagnosis, treatment options, and the critical importance of early detection.
What is Creutzfeldt-Jakob Disease?
Creutzfeldt-Jakob Disease (CJD) is a rare, degenerative, invariably fatal brain disorder that affects about one person in every one million people per year worldwide. The disease belongs to a family of human and animal diseases known as the prion diseases. Prions are misfolded proteins that replicate by converting their properly folded counterparts in the brain, leading to brain damage and a rapid decline in mental function and movement. Symptoms can include dementia, muscle stiffness, confusion, difficulty moving, and visual disturbances, progressing swiftly to severe impairment and ultimately death. CJD can occur sporadically, be inherited, or arise from exposure to brain or nervous system tissue, usually through certain medical procedures.
Types of Creutzfeldt-Jakob Disease
CJD exists in several forms, which are characterized by their cause and genetic factors:
- Sporadic CJD: The most common form, occurring without known reason.
- Variant CJD (vCJD): Linked to consumption of meat from cattle affected by bovine spongiform encephalopathy (BSE), also known as “mad cow disease.”
- Familial CJD: Caused by a genetic mutation and accounts for a small percentage of cases.
- Iatrogenic CJD: Resulting from accidental transmission through medical procedures, such as transplantation of infected human growth hormone or dura mater grafts.
Statistics on Incidence Rates Globally
CJD is considered extremely rare. Globally, the incidence rate is estimated to be one case per million people per year. Sporadic CJD is the most common form, accounting for approximately 85% of cases. Variant CJD, linked to BSE, has been primarily identified in the United Kingdom and other European countries but remains exceedingly rare. Familial CJD accounts for about 10-15% of cases, and iatrogenic CJD is even less common. Due to its rarity, precise global statistics are challenging to obtain, but ongoing surveillance in many countries helps track the occurrence and spread of this devastating disease.
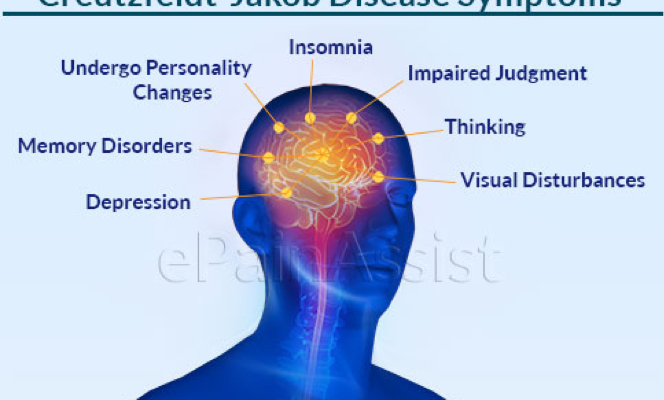
Understanding the Symptoms of Creutzfeldt-Jakob Disease (CJD)
Understanding these symptoms and how the disease progresses is crucial for timely diagnosis and management. Let’s delve into the early symptoms, progression of the disease, its neurological impact, physical manifestations, and how symptoms can vary among the different types of CJD.
Early Symptoms and Progression of the Disease
The initial symptoms of CJD are often subtle and may include:
- Memory problems, forgetfulness, and confusion, which are often mistaken for signs of aging or stress.
- Changes in personality and behavior, including anxiety, depression, or irritability.
- Difficulty walking, clumsiness, and a lack of coordination.
As the disease progresses, these symptoms rapidly worsen. Patients may experience:
- Severe mental impairment, including the inability to think, reason, or remember.
- Muscle stiffness, twitching, and involuntary movements.
- Difficulty speaking and swallowing, leading to nutritional challenges.
The speed at which symptoms worsen varies from person to person, but the disease typically progresses rapidly, leading to severe disability and eventually death, often within a year of diagnosis.
Neurological Impact and Physical Manifestations
CJD primarily affects the brain and nervous system. On a neurological level, it causes the brain tissue to degenerate rapidly, leading to the formation of tiny holes in the brain, giving it a sponge-like appearance when viewed under a microscope. This degeneration results in the loss of brain function, manifesting physically as:
- Muscle weakness and loss of motor control.
- Visual disturbances or blindness.
- Insomnia and other sleep disturbances.
- Seizures in some cases.
These symptoms reflect the widespread damage CJD causes in the brain, impacting various brain functions and leading to a range of neurological and physical symptoms.
Variation in Symptoms Among Types of CJD
The symptoms of CJD can vary somewhat among its different types:
- Sporadic CJD: The most common type, where symptoms usually appear in later life, typically around the age of 60, and progress rapidly.
- Variant CJD (vCJD): Linked to consuming meat from cattle affected by Bovine Spongiform Encephalopathy (BSE), variant CJD affects younger individuals and has a longer duration of symptoms before rapid progression.
- Familial CJD: Caused by a genetic mutation, this form of CJD presents similarly to sporadic CJD but may occur in younger patients and has a slightly different pattern of symptom progression.
- Iatrogenic CJD: Results from medical procedures that inadvertently transmit the disease, with symptom patterns that can vary based on the method of transmission.
Understanding the nuances in symptoms among the different types of CJD is crucial for medical professionals in diagnosing and managing the disease. Although there is currently no cure for CJD, early recognition of symptoms can lead to supportive treatments that improve the quality of life for patients and their families.
However, CJD is a complex disease with a wide range of symptoms that can vary significantly among individuals and the type of CJD. Awareness and understanding of these symptoms are vital for early diagnosis, which is crucial in managing the disease and providing supportive care to patients and their families.
Diagnosis of Creutzfeldt-Jakob Disease (CJD)
Understanding the diagnostic process for CJD can help in managing the disease more effectively. This article outlines the initial diagnostic tests, advanced techniques, the role of genetic testing, and the challenges faced in diagnosing CJD.
Initial Diagnostic Tests and Assessments
The diagnosis of Creutzfeldt-Jakob Disease begins with a comprehensive neurological examination. Healthcare providers assess the patient’s medical history, symptoms, and conduct various neurological tests to check for physical and cognitive impairments typical of CJD. Following the initial assessment, several imaging and electrical tests are performed:
- Magnetic Resonance Imaging (MRI): MRI scans are crucial in detecting changes in brain structure and patterns indicative of CJD, such as spongiform changes and hyperintense signals in specific brain areas.
- Electroencephalogram (EEG): An EEG may reveal characteristic patterns in brain wave activity associated with CJD, including periodic sharp wave complexes, although these are not present in all cases.
Advanced Diagnostic Techniques
For a more definitive diagnosis, advanced diagnostic techniques are employed, including:
- Spinal Fluid Tests for 14-3-3 Protein: The presence of 14-3-3 protein in cerebrospinal fluid is a marker for neuronal damage and is often elevated in CJD patients. This test, while not specific to CJD, can support the diagnosis when combined with clinical findings and other test results.
- Real-Time Quaking-Induced Conversion (RT-QuIC): This novel diagnostic test detects prion protein aggregates, the causative agent of CJD, in cerebrospinal fluid. RT-QuIC is highly sensitive and specific for CJD, making it a powerful tool for early and accurate diagnosis.
The Role of Genetic Testing in Hereditary CJD
Approximately 10-15% of CJD cases are hereditary, caused by mutations in the PRNP gene. Genetic testing can identify mutations associated with hereditary CJD, providing crucial information for diagnosing familial cases and for genetic counseling of family members. It’s important to note that genetic testing is recommended only when there’s a known family history of the disease or when the clinical presentation suggests a genetic form.
Challenges in Diagnosing CJD Accurately and Early
Diagnosing CJD poses significant challenges:
- Symptom Similarity: Early symptoms of CJD are nonspecific and can resemble other neurodegenerative disorders, leading to misdiagnosis.
- Lack of a Definitive Early Test: While advanced tests like RT-QuIC have improved diagnosis, there’s still no single test that can definitively diagnose CJD in its earliest stages.
- Rapid Disease Progression: CJD progresses quickly, often before a definitive diagnosis can be made, impacting treatment and management options.
However, diagnosing Creutzfeldt-Jakob Disease accurately and early requires a combination of clinical assessments, advanced diagnostic tests, and in some cases, genetic testing. Despite advances in diagnostic techniques, challenges remain due to the disease’s rapid progression and the non-specific nature of early symptoms. Ongoing research and development of new diagnostic tools are essential for improving the detection and management of CJD.
Treatment Options for Creutzfeldt-Jakob Disease (CJD)
As of now, there is no cure for CJD, which makes the diagnosis daunting for patients and their loved ones. However, understanding the available treatment options can provide some relief by managing symptoms and improving the quality of life.
Supportive Treatments
The core approach to CJD management revolves around supportive treatments. Since the disease directly affects neurological functions, symptom management is crucial. These treatments aim to provide comfort and maintain the dignity of the patient throughout the disease’s progression. Supportive care includes:
- Medications for Myoclonus and Seizures: Drugs are often prescribed to control myoclonus (sudden, involuntary muscle jerks) and seizures, which are common symptoms of CJD. These medications can help reduce the frequency and severity of these episodes, contributing to a more comfortable state for the patient.
- Pain Management: Pain control is another critical aspect of supportive care. Physicians may recommend a variety of pain relief options, ranging from traditional painkillers to more specific neuropathic pain medications, tailored to the individual’s needs and symptomatology.
- Neurological Support: As the disease progresses, patients may require assistance with mobility, speech, and other neurological functions. Occupational and physical therapy can play a role in maintaining as much independence as possible for the patient.
Experimental Treatments and Clinical Trials
In the quest for a cure, researchers are exploring a range of experimental treatments and engaging in clinical trials to discover effective therapies for CJD. These include:
- Antiviral Drugs: Some studies have investigated the potential of antiviral drugs in slowing the progression of CJD, with the rationale that these medications might interfere with the pathogenic prion proteins that cause the disease.
- Immunotherapy: This treatment approach involves stimulating the body’s immune system to attack the harmful prion proteins. Although still in the experimental phase, immunotherapy offers a glimpse of hope in managing or potentially halting the progression of CJD.
It’s important for patients and families to consult with healthcare professionals about the possibility of participating in clinical trials. These studies not only contribute to the scientific understanding of CJD but also offer access to cutting-edge treatments that are not yet widely available.
The Role of Palliative Care
Palliative care is integral to the management of Creutzfeldt-Jakob Disease, focusing on enhancing the quality of life for patients and their families. This multidisciplinary approach addresses the physical, emotional, spiritual, and social needs of the patient. Palliative care teams work to:
- Alleviate Symptoms: Through comprehensive symptom management, palliative care aims to reduce suffering and improve comfort.
- Provide Emotional and Spiritual Support: Counseling and support services are available to help patients and their families cope with the emotional and psychological aspects of the disease.
- Assist with Decision Making: Guidance is provided to help families make informed decisions about care options and end-of-life planning, ensuring that the patient’s wishes are respected.
However, while there is currently no cure for Creutzfeldt-Jakob Disease, a combination of supportive treatments, experimental therapies, and palliative care can significantly impact the management of the disease. These approaches are designed to improve the quality of life for CJD patients and provide support for their families during challenging times. Engaging with a healthcare team that specializes in neurodegenerative diseases can offer the most comprehensive and compassionate care for those affected by CJD.
Research and Future Directions in Creutzfeldt-Jakob Disease (CJD) Treatment
The quest for effective Creutzfeldt-Jakob Disease (CJD) treatments remains a critical focus within the medical and scientific communities. This rare but fatal brain disorder, characterized by rapid neurodegeneration, presents significant challenges in both diagnosis and treatment. However, ongoing research and global collaboration offer hope for breakthroughs in managing this disease. This article explores the current landscape of CJD treatment research, emphasizing the importance of early detection, and highlights how international cooperation is pivotal in advancing patient support and therapy development.
Ongoing Research into CJD Treatments
The landscape of CJD research is diverse, with scientists exploring various avenues to understand and combat the disease. Key areas of investigation include the development of therapeutic agents capable of crossing the blood-brain barrier to directly target the abnormal prion proteins responsible for CJD. Researchers are also examining the role of immunotherapy in neutralizing prions, alongside advancements in antiviral therapies which have shown promise in preliminary studies.
Another exciting development is the use of gene editing technologies, such as CRISPR-Cas9, to manipulate the genetic factors that may predispose individuals to CJD. This approach not only opens the door to potential treatments but also enhances our understanding of the disease’s molecular underpinnings.
The Importance of Early Detection Research
Early detection of CJD is paramount in improving treatment outcomes. The disease’s rapid progression means that any delay can significantly hinder the effectiveness of therapeutic interventions. Current research is therefore focused on identifying biomarkers that can signal the presence of CJD before symptoms become pronounced. Techniques such as advanced imaging and the analysis of cerebrospinal fluid are at the forefront of this effort, offering the promise of earlier diagnosis and the possibility of intervention before significant brain damage occurs.
Global Collaboration in CJD Research and Patient Support
The fight against CJD is a global endeavor, with researchers, clinicians, and patient advocacy groups worldwide working in concert to advance our understanding and treatment of the disease. International consortia and networks facilitate the sharing of data and resources, accelerating the pace of discovery and ensuring that insights into CJD are disseminated broadly and rapidly.
Patient support also benefits greatly from this collaborative approach. Global partnerships enable the development of comprehensive care strategies, integrating the latest research findings into treatment plans and ensuring that patients and their families have access to the support they need. This collective effort not only furthers research but also enhances the quality of life for those affected by CJD.
While the path to effective treatments for Creutzfeldt-Jakob Disease is fraught with challenges, ongoing research and international collaboration offer hope. By focusing on the development of innovative therapies and the importance of early detection, the scientific community moves closer to understanding and ultimately defeating CJD. The global effort in research and patient support underscores the commitment to tackling this devastating disease, promising a future where CJD can be effectively managed or even cured.
Living with Creutzfeldt-Jakob Disease
Living with Creutzfeldt-Jakob Disease (CJD) presents unique challenges and requires comprehensive care strategies for both patients and their families. This section aims to offer guidance on caregiving, mental health support, and navigating the complex legal and ethical considerations associated with CJD.
Caregiving for Someone with CJD
Caring for a loved one with Creutzfeldt-Jakob Disease demands a well-informed approach that prioritizes the patient’s comfort and quality of life. Here are some key points to consider:
- Personalized Care Plans: Each CJD case is unique, so it’s crucial to work closely with healthcare professionals to create a care plan tailored to the patient’s specific needs and symptoms.
- Safety Measures: Implement safety modifications in the home to prevent falls and injuries, considering CJD’s impact on coordination and mobility.
- Nutritional Support: Difficulty swallowing is a common symptom, which may necessitate adjustments in diet and possibly the use of feeding tubes, under medical advice.
- Symptom Management: Be proactive in managing symptoms and side effects of treatment with the help of the medical team to ensure the patient’s comfort.
Mental Health Support for Patients and Families
The emotional impact of CJD on both patients and their families can be profound. It’s essential to seek support:
- Professional Counseling: Consider therapy for patients and family members to cope with the emotional stress and grief that CJD can bring.
- Support Groups: Connecting with others going through similar experiences can provide comfort and practical advice for managing the disease.
- Self-Care: Caregivers should also prioritize their own mental health and well-being, taking time for rest and activities that they enjoy.
Legal and Ethical Considerations
Navigating the legal and ethical aspects of CJD involves several key considerations:
- Advanced Directives: Early in the disease progression, discuss and document the patient’s wishes regarding treatment and end-of-life care to guide future decisions.
- End-of-Life Care: Consider palliative care options that focus on relieving symptoms and improving quality of life as the disease progresses.
- Legal Advice: Consult with legal professionals experienced in health care law to ensure that all decisions and documents are in order, including wills and guardianship arrangements if necessary.
By focusing on tailored care strategies, emotional support, and addressing legal and ethical considerations head-on, caregivers can provide compassionate care that honors the dignity and wishes of their loved ones with CJD. Remember, you’re not alone; seek out professional guidance and community support to help you through this journey.
FAQs on Creutzfeldt-Jakob Disease
What is Creutzfeldt-Jakob Disease (CJD)?
Creutzfeldt-Jakob Disease (CJD) is a rare, degenerative, invariably fatal brain disorder. It affects about one person in every one million people per year worldwide. CJD usually appears in later life and runs a rapid course. Typically, onset of symptoms occurs at about age 60, and death follows within a year.
How is CJD diagnosed?
Diagnosing CJD can be challenging, especially in the early stages, as its signs and symptoms can mimic those of other dementia-like brain disorders. Tests used in the diagnosis include EEG (electroencephalogram), MRI (magnetic resonance imaging), spinal fluid tests for 14-3-3 protein, and, in some cases, a brain biopsy. The only way to confirm a diagnosis of CJD is by brain biopsy or autopsy.
What treatment options are available for CJD?
Currently, there is no cure for CJD, and treatment focuses on alleviating symptoms and making the patient as comfortable as possible. Medical management might include medications to help control symptoms such as pain, seizures, and mood swings. Supportive care with assistance in feeding, bathing, and dressing may be necessary as the disease progresses.
Can CJD be inherited?
Yes, while the majority of CJD cases are sporadic, meaning they occur with no known cause, a small percentage of cases are hereditary. These cases are caused by a mutation in the PRNP gene and can be passed down from an affected parent to their child.
How can caregivers support a patient with CJD?
Caring for someone with CJD requires a comprehensive approach. This includes managing physical symptoms, providing emotional support, and ensuring the patient’s environment is safe and comfortable. Caregivers should also seek support for themselves, both for practical caregiving advice and emotional coping strategies.
Is there a risk of transmitting CJD?
CJD cannot be transmitted through casual contact with a person who has the disease. However, it can be transmitted through exposure to brain or nervous system tissue, usually in a medical or research setting. Strict protocols are in place to minimize this risk.
Where can I find more information and support for CJD?
For more information and support, contact national and international organizations dedicated to CJD research and patient care. These organizations offer resources for patients, families, and healthcare professionals, including the latest research, support groups, and care management advice.
Conclusion
For those seeking more information or support related to CJD, there are numerous resources available. Organizations such as the Creutzfeldt-Jakob Disease Foundation offer comprehensive guides, support networks, and up-to-date information on CJD. These resources provide invaluable support for individuals affected by CJD, whether patients, families, or caregivers, helping them navigate the challenges associated with the disease.
In closing, the fight against Creutzfeldt-Jakob Disease is a collective effort that requires our attention and support. By fostering research, raising awareness, and offering support to those affected, we can make significant strides in understanding and managing this devastating condition. Together, we can make a difference in the lives of those touched by CJD and move closer to a future where effective treatments, and ultimately a cure, are available.