Costochondritis Symptoms: Costochondritis, a condition often misunderstood and overlooked, emerges as a significant concern for many individuals, marked by pain and discomfort in the chest region.
This comprehensive guide delves into the symptoms and causes of costochondritis, aiming to enlighten readers on its intricacies and the steps one can take towards management and recovery.
What is Costochondritis?
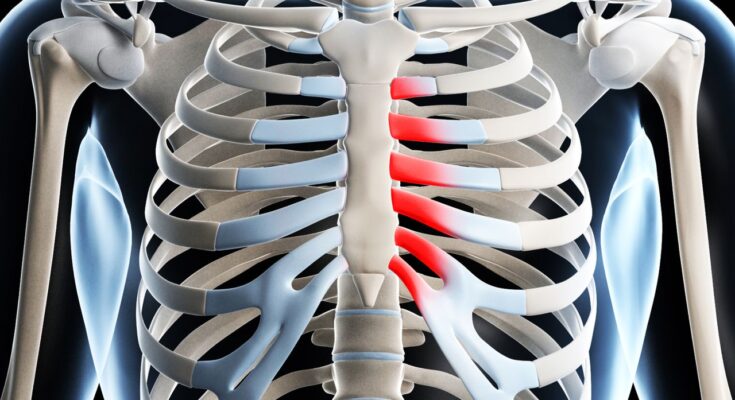
Costochondritis is an inflammatory condition that affects the cartilage connecting the ribs to the sternum, an area known as the costosternal junction. This condition is characterized by chest pain that can mimic that of a heart attack or other heart conditions, leading to concern or confusion for those experiencing it. However, unlike heart-related issues, costochondritis pain is more likely to be reproducible with palpation or movement, indicating its musculoskeletal origin.
Distinction Between Costochondritis and Other Chest-Related Conditions
Understanding the difference between costochondritis and other chest-related conditions is crucial for accurate diagnosis and treatment. Unlike conditions affecting the heart or lungs, costochondritis does not come with systemic symptoms like fever, cough, or shortness of breath. Its primary symptom is localized chest pain, often exacerbated by certain movements, deep breathing, or physical activity. This contrasts with the more severe and widespread symptoms associated with cardiac events, which may include radiating pain to the arm or jaw, nausea, and sweating.
Brief Mention of the Anatomy Involved in Costochondritis
The anatomy involved in costochondritis includes the rib cage, cartilage, and sternum. The rib cage is a critical structure made of ribs connected to the spine at the back and the sternum at the front. The ribs are connected to the sternum by costal cartilages, which provide flexibility and movement. In costochondritis, it is this cartilage at the costosternal junction that becomes inflamed, leading to pain and discomfort. Understanding this anatomy is essential in distinguishing costochondritis from other potential causes of chest pain and in guiding effective treatment strategies.
However, costochondritis is a common source of chest pain stemming from inflammation of the cartilage connecting the ribs to the sternum. Distinguishing this condition from other chest-related issues is vital for appropriate management, and a basic understanding of the involved anatomy helps clarify the origins and characteristics of the pain experienced.
Symptoms of Costochondritis: A Comprehensive Guide
Understanding the symptoms of costochondritis is crucial for identifying this condition and differentiating it from other, potentially more serious, conditions. Below, we detail the common symptoms associated with costochondritis, provide insight on how to recognize these symptoms, and discuss potential triggers that can exacerbate the condition.
Common Symptoms of Costochondritis
The primary symptom of costochondritis is chest pain. This pain can vary in intensity from mild to severe and is often described as sharp, aching, or pressure-like. The characteristics of costochondritis pain include:
- Location: The pain is typically concentrated on the left side of the chest but can affect any part of the chest.
- Pain on Palpation: Tenderness is felt when pressing on the costosternal junction, the area where the ribs meet the breastbone.
- Worsening with Movement: Activities that involve moving the upper body or deep breathing can intensify the pain.
- Radiation: Although primarily in the chest, the pain can radiate to the back or abdomen.
Differentiating Costochondritis Symptoms
Distinguishing costochondritis from other conditions like heart disease, gastroesophageal reflux disease (GERD), or lung issues is essential due to the overlapping symptom of chest pain. Several key factors can help identify costochondritis:
- Pain Location and Quality: Costochondritis pain is localized and can be reproduced by pressing on the affected area, which is not typical of heart-related chest pain.
- No Associated Symptoms: Unlike heart conditions, costochondritis usually does not come with symptoms like shortness of breath, nausea, or sweating.
- Physical Activity Impact: The pain associated with costochondritis is more likely to increase with certain movements or physical activity, unlike the pain from cardiac conditions, which can be triggered by stress or exertion but not by specific movements.
Potential Triggers for Costochondritis
Understanding what can exacerbate costochondritis is key to managing the condition. Potential triggers include:
- Physical Strain: Heavy lifting, strenuous exercise, or sudden movements can aggravate the pain.
- Poor Posture: Sitting or standing in a poor posture for extended periods can increase stress on the chest area.
- Injury: Direct injury to the chest can trigger or worsen symptoms.
- Respiratory Infections: Severe coughing from respiratory infections can strain the chest and exacerbate pain.
By recognizing the symptoms of costochondritis and the activities that can trigger or worsen these symptoms, individuals can take steps to manage their condition effectively. If you suspect you have costochondritis, consult a healthcare professional for a proper diagnosis and treatment plan. Remember, while costochondritis is not life-threatening, distinguishing it from other causes of chest pain is crucial for ensuring your overall health and well-being.
Causes and Risk Factors of Costochondritis
Understanding the causes and risk factors associated with costochondritis is essential for both patients and healthcare providers. This article explores the known causes of costochondritis, discusses risk factors that may increase the likelihood of developing the condition, and suggests ways to mitigate these risks.
Known Causes of Costochondritis
- Physical Strain or Injury: Activities that involve heavy lifting, strenuous exercise, or sudden movements can strain the chest area, leading to inflammation of the costal cartilage. Injuries to the chest, whether from falls, sports, or accidents, are also common culprits.
- Respiratory Infections and Related Coughing: Viral infections, particularly those affecting the respiratory system, can lead to persistent coughing. This repeated coughing puts stress on the rib cage and the costosternal joints, potentially causing costochondritis.
- Allergic Reactions and Rheumatic Diseases: In some cases, allergic reactions that trigger widespread inflammation in the body can also affect the costochondral junctions. Similarly, rheumatic diseases like rheumatoid arthritis and lupus, which cause chronic inflammation, can contribute to the development of costochondritis.
Risk Factors for Costochondritis
- Age Demographics: While costochondritis can occur at any age, it is more frequently diagnosed in people over 40. This may be due to the cumulative wear and tear on the costochondral cartilage over time.
- Specific Physical Activities or Lifestyles: Individuals engaged in activities that involve repetitive arm movements or upper body strain, such as rowing, weightlifting, or certain types of manual labor, are at a higher risk. Sedentary lifestyles can also contribute, as lack of exercise may weaken chest muscles and place additional strain on the chest wall.
- Pre-existing Health Conditions: People with chronic respiratory conditions, arthritis, or those who have had chest injuries in the past are more susceptible to developing costochondritis. Additionally, individuals with poor posture or those who carry heavy bags regularly may experience increased stress on their chest wall, leading to inflammation.
Mitigating the Risk
Understanding the causes and risk factors of costochondritis is the first step in preventing or managing the condition. For those engaged in high-risk activities or with pre-existing health conditions, taking precautions such as practicing good posture, avoiding repetitive strain, and engaging in exercises that strengthen the chest muscles can help reduce the likelihood of developing costochondritis. Additionally, managing chronic conditions effectively and seeking medical advice when experiencing chest pain can ensure timely diagnosis and treatment, preventing complications associated with costochondritis.
However, costochondritis is a condition with various causes and risk factors, ranging from physical strain and respiratory infections to rheumatic diseases and specific lifestyle choices. By being aware of these factors, individuals can take proactive steps to minimize their risk and ensure a prompt, effective response should symptoms arise.
Diagnosing Costochondritis
Here, we delve into the diagnostic process for costochondritis, highlighting the importance of a comprehensive medical review and physical examination, alongside tests to rule out other conditions.
Medical History Review
The first step in diagnosing costochondritis involves a thorough review of the patient’s medical history. This review helps healthcare professionals understand the onset, duration, and characteristics of the chest pain, including any activities or incidents that may have triggered the condition. By gathering detailed information on past health issues and current symptoms, doctors can begin to differentiate costochondritis from other potential causes of chest pain.
Physical Examination
Following the medical history review, a physical examination is conducted with a focus on the chest area. Doctors look for specific signs of costochondritis, such as tenderness or pain when pressure is applied to the areas where the ribs join the breastbone. Since costochondritis is primarily diagnosed based on the presence of localized chest pain without any visible signs of inflammation, the physical exam plays a critical role in the diagnosis process.
Tests to Rule Out Other Conditions
To ensure an accurate diagnosis and rule out more serious conditions, doctors may order additional tests. An Electrocardiogram (EKG) can be performed to check for heart problems, while a chest X-ray can help rule out lung and heart diseases. These tests are crucial because symptoms of costochondritis can closely resemble those of heart attacks or other cardiac conditions. In some cases, blood tests may also be conducted to exclude infections or rheumatic diseases.
Importance of Professional Evaluation
Seeking professional evaluation for chest pain is vital due to the potential for confusion with more serious conditions. A healthcare professional’s expertise ensures that the diagnostic process is thorough, considering all possible causes of chest pain. By ruling out life-threatening conditions, doctors can confidently diagnose costochondritis and recommend an appropriate treatment plan.
However, diagnosing costochondritis requires a careful evaluation that includes a review of the patient’s medical history, a detailed physical examination, and tests to exclude other conditions. The complexity of chest pain diagnosis underscores the importance of professional evaluation, ensuring that patients receive the correct diagnosis and treatment for their symptoms.
Treatment Options for Costochondritis
This guide offers a comprehensive overview of typical treatment options for managing costochondritis, including home remedies, medications, physical therapy, exercises, and insights into their effectiveness and the potential need for ongoing management.
Home Remedies
Home remedies are a cornerstone of costochondritis treatment, focusing on reducing inflammation and relieving pain without the need for medical intervention. These include:
- Heat and Cold Therapy: Applying heat packs or cold packs to the chest area can help reduce inflammation and pain. It’s advisable to use a cloth barrier to protect the skin and limit application to 15-20 minutes at a time.
- Rest: Limiting physical activity that aggravates the chest area can prevent further irritation of the costal cartilage.
- Positioning: Sleeping in a more upright position or using pillows for support can reduce pressure on the chest and alleviate discomfort during the night.
Medications
Over-the-counter (OTC) and prescription medications can play a pivotal role in managing costochondritis symptoms:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): OTC NSAIDs such as ibuprofen (Advil, Motrin IB) or naproxen (Aleve) can help reduce inflammation and pain. It’s important to use these medications as directed to avoid potential side effects.
- Analgesics: For those who cannot take NSAIDs, acetaminophen (Tylenol) may be an alternative to help relieve pain, although it does not reduce inflammation.
Physical Therapy and Exercises
Physical therapy and specific exercises can strengthen the chest muscles, improve posture, and reduce the recurrence of costochondritis symptoms:
- Stretching Exercises: Gentle stretching of the chest and upper body muscles can improve flexibility and reduce tension in the chest area.
- Strengthening Exercises: A physical therapist may recommend exercises to strengthen the chest, back, and shoulder muscles, supporting better posture and reducing stress on the ribcage.
Effectiveness of Treatments and Ongoing Management
The effectiveness of costochondritis treatments varies from person to person, and a combination of therapies may be necessary to find relief. While many individuals experience significant improvement with conservative treatments, some may require ongoing management to keep symptoms at bay. It’s important to work closely with a healthcare provider to tailor a treatment plan that addresses the specific needs and symptoms of the individual.
Understanding the potential triggers and learning to manage activities that exacerbate symptoms can also play a crucial role in long-term management. Regular follow-ups with a healthcare provider can help adjust treatment plans as needed and ensure that symptoms are effectively managed.
However, costochondritis can be a manageable condition with the right combination of home remedies, medications, and physical therapy. By adopting a proactive approach to treatment and working closely with healthcare professionals, individuals can significantly reduce their symptoms and improve their overall quality of life.
Preventing Costochondritis
Now, we’ll explore practical tips and exercise techniques aimed at reducing the risk of developing costochondritis, focusing on proper exercise methods, avoiding activities that strain the chest area, and incorporating strengthening exercises for the chest and upper body.
Embrace Proper Exercise Techniques
Adopting correct exercise techniques is fundamental in preventing costochondritis. Engaging in physical activities with improper form can exert unnecessary pressure on the chest area, leading to inflammation and pain. Here are some guidelines to ensure your exercise routine supports chest health:
- Warm-Up Adequately: Always begin with a thorough warm-up to prepare your muscles and joints for the upcoming activity. This can include light cardiovascular exercises or dynamic stretches that target the upper body.
- Maintain Proper Form: Whether lifting weights, running, or performing bodyweight exercises, maintaining proper form is critical. Ensure your chest is not overly compressed or strained during exercise. If unsure, consider seeking advice from a fitness professional.
- Gradually Increase Intensity: Avoid sudden increases in exercise intensity or volume. Gradually build up your fitness levels to give your body time to adapt, reducing the risk of chest strain.
Avoid Activities That Strain the Chest Area
Certain activities, especially those involving repetitive movements or heavy lifting, can strain the chest area and trigger costochondritis. To prevent this:
- Limit Repetitive Upper Body Movements: Activities such as rowing or certain types of manual labor can increase the risk. If these activities are unavoidable, take frequent breaks and use supportive equipment if available.
- Be Cautious with Heavy Lifting: When lifting heavy objects, use proper techniques to distribute the load evenly and avoid putting excessive strain on the chest. Engage your legs and core to support the effort.
Strengthening Exercises for Chest and Upper Body
Strengthening the muscles around the chest and upper body can help support the ribcage and reduce the risk of costochondritis. Focus on exercises that enhance strength without overstraining the chest area:
- Incorporate Low-Impact Strength Training: Exercises such as push-ups, light bench presses, or resistance band workouts can strengthen the chest muscles without excessive strain. Ensure you perform these exercises with correct form and moderate intensity.
- Strengthen the Upper Back and Shoulders: Exercises that target the upper back and shoulders, such as rows or reverse flys, can help balance the muscle strength around the chest and upper body, offering additional support to the ribcage.
- Practice Core Strengthening: A strong core supports the upper body and can reduce the strain on the chest area during physical activities. Incorporate exercises like planks, bird-dogs, and gentle yoga poses to build core strength.
However, by adopting proper exercise techniques, avoiding activities that overly strain the chest area, and engaging in targeted strengthening exercises, you can significantly reduce the risk of developing costochondritis. Remember to listen to your body and consult with healthcare professionals if you have concerns about chest pain or discomfort. With these preventative measures, you can maintain a healthy, active lifestyle while protecting your chest health.
FAQ Section: Understanding Costochondritis
What is Costochondritis?
Costochondritis is a medical condition characterized by inflammation of the cartilage that connects a rib to the breastbone (sternum). This inflammation can cause sharp chest pain which is often mistaken for a heart attack. Costochondritis is a relatively common condition and is generally benign, meaning it’s not life-threatening.
What Causes Costochondritis?
The exact cause of costochondritis is often difficult to determine. However, it may be associated with injury, physical strain, heavy lifting, or repetitive motion. Infections and certain forms of arthritis can also contribute to the development of this condition.
How Is Costochondritis Diagnosed?
Diagnosis typically involves a physical examination, where a doctor will look for tenderness in the costosternal, costochondral, or costovertebral areas. Imaging tests like chest X-rays, CT scans, or MRIs are sometimes used to rule out other conditions.
What Are the Symptoms of Costochondritis?
The primary symptom is chest pain on the left side of the body that may feel sharp, aching, or pressure-like. The pain can increase with movement or deep breathing and decrease with rest. It’s localized around the affected cartilage, usually on the upper ribs.
How Is Costochondritis Treated?
Treatment focuses on relieving pain and inflammation. Over-the-counter pain relievers such as ibuprofen or naproxen can be effective. Applying heat or ice to the affected area and avoiding activities that worsen the pain are also recommended. In some cases, physical therapy can help.
Can Costochondritis Go Away on Its Own?
Yes, costochondritis often resolves on its own without specific treatment. The duration varies among individuals, ranging from a few days to several weeks. However, chronic cases may persist for months or longer.
Is Costochondritis Contagious?
No, costochondritis is not contagious. It is an inflammation of the cartilage and does not spread from person to person.
When Should I See a Doctor for Costochondritis?
If you experience persistent chest pain that doesn’t improve with rest or over-the-counter medications, it’s important to see a doctor. Also, seek immediate medical attention if you have difficulty breathing, high fever, signs of infection around the ribs, or severe chest pain, as these could indicate more serious conditions.
Conclusion
As we conclude, the emphasis on recognizing symptoms and understanding the causes of costochondritis cannot be overstated. If you or someone you know is experiencing symptoms that align with those of costochondritis, it is highly encouraged to seek medical advice. Consulting a healthcare professional not only aids in confirming a diagnosis but also ensures that any underlying issues are addressed, facilitating a path towards relief and recovery.
In the realm of health and well-being, being informed and proactive about conditions like costochondritis is a crucial step in maintaining one’s health. Remember, your health is invaluable, and seeking professional guidance is a wise and necessary action when faced with health uncertainties.