Corticobasal Degeneration Symptoms: Corticobasal degeneration (CBD) is a rare, progressive neurodegenerative disorder that affects the brain’s cortex and basal ganglia.
It leads to a wide range of physical and cognitive symptoms, deeply impacting the lives of those affected.
Understanding its symptoms and causes is crucial for early diagnosis and management, albeit there is currently no cure for CBD.
Understanding Corticobasal Degeneration
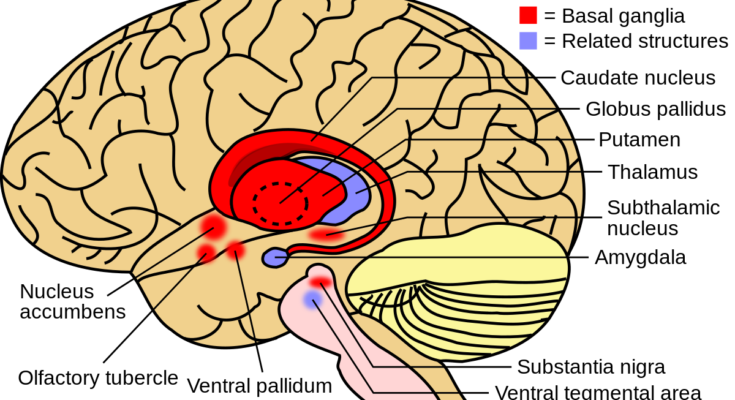
Corticobasal Degeneration (CBD) is a rare, progressive neurodegenerative disorder that significantly impacts motor functions and cognitive abilities. Characterized by the gradual deterioration of various brain regions, particularly the cortex and basal ganglia, CBD presents a complex array of symptoms that often overlap with other neurological conditions. This makes its diagnosis particularly challenging for healthcare professionals.
Prevalence and Demographics Affected
CBD is considered a rare condition, with its prevalence challenging to quantify accurately due to its similarity to other neurodegenerative disorders. However, it is most commonly diagnosed in individuals aged 60 and above, with no clear preference for any gender. The rarity and specific age demographic targeted by CBD emphasize the need for increased awareness and understanding within the medical community and the general public.
Complexity of Diagnosing CBD
One of the most significant challenges in managing CBD is the complexity of its diagnosis. Its symptoms closely mimic those of other neurological conditions, such as Parkinson’s disease, progressive supranuclear palsy, and Alzheimer’s disease, among others. This overlap can lead to misdiagnosis or delayed diagnosis, impacting treatment efficacy and patient quality of life. Healthcare professionals must rely on a combination of clinical evaluations, imaging studies, and the exclusion of other conditions to accurately diagnose CBD, underscoring the need for advanced diagnostic tools and increased research into this debilitating disorder.
However, Corticobasal Degeneration is a condition that demands greater awareness and understanding due to its complex nature and the diagnostic challenges it presents. With advancements in medical research and diagnostic methodologies, there is hope for more accurate diagnoses and, ultimately, more effective treatments for those affected by CBD.
Symptoms of Corticobasal Degeneration
Understanding the symptoms can help in early diagnosis and management of the condition. This article breaks down the symptoms into early signs, progressive symptoms, and other associated symptoms to provide a comprehensive overview.
Early Signs
The onset of CBD can be subtle and may be mistaken for other conditions. Early signs include:
- Motor Symptoms: One of the first noticeable signs of CBD is difficulty with motor skills. This may manifest as clumsiness in one hand, difficulty with fine motor tasks like buttoning a shirt, or changes in handwriting.
- Asymmetrical Symptoms: Symptoms typically start on one side of the body and may include stiffness, shakiness, or a lack of coordination. This asymmetry is a hallmark of early CBD.
- Cognitive Decline: Mild cognitive impairment, especially in planning, organizing, and problem-solving, can occur early in the disease process.
Progressive Symptoms
As CBD progresses, symptoms become more pronounced and debilitating:
- Movement Disorders: Individuals may experience rigidity, dystonia (abnormal muscle postures), and myoclonus (sudden, involuntary muscle jerks). These symptoms can significantly impair mobility and daily activities.
- Speech and Language Difficulties: Progressive difficulties with speech and language, such as apraxia (difficulty performing movements on command) and aphasia (trouble understanding or producing speech), are common.
- Difficulty Swallowing: Dysphagia, or difficulty swallowing, can develop, increasing the risk of choking or aspiration pneumonia.
Other Associated Symptoms
CBD can also lead to a variety of other symptoms, reflecting the widespread brain involvement:
- Cognitive and Behavioral Changes: Executive function decline is prominent, alongside possible changes in personality and behavior, such as apathy, irritability, and impulsivity.
- Sensory Symptoms: Some individuals may experience numbness, tingling, or pain in the affected limbs.
- Eye Movement Abnormalities: Difficulty with voluntary eye movements, including double vision or difficulty focusing, can occur as the disease progresses.
Early recognition and diagnosis are crucial for managing symptoms and improving quality of life. If you or someone you know is experiencing these symptoms, it’s important to consult a healthcare professional for a thorough evaluation and tailored management plan.
Causes of Corticobasal Degeneration
Understanding its causes is critical for developing targeted therapies and improving patient outcomes. The etiology of CBD is thought to be influenced by a combination of genetic factors, environmental triggers, and pathological protein accumulations, with the tau protein playing a central role.
Genetic Factors
Recent advancements in genetic research have begun to shed light on the potential genetic predisposition to CBD. While the vast majority of cases appear sporadic, meaning they occur at random without a clear hereditary pattern, there are rare familial cases that suggest a genetic component may be involved. These familial instances provide valuable insights, offering researchers clues that could lead to the identification of specific genetic markers associated with the disease. However, it’s important to note that these cases are exceedingly rare, and the direct genetic contributions to CBD are still not fully understood.
Environmental Factors
The search for environmental factors that might trigger CBD has been extensive, yet conclusive evidence remains elusive. Researchers have explored various potential environmental triggers, including exposure to toxins, lifestyle factors, and even viral infections, as possible contributors to the development of the disease. Despite these efforts, there has been no definitive proof linking any specific environmental factor to CBD. This uncertainty highlights the complexity of the disease and the need for further research to identify any external factors that may play a role in its onset.
The Role of Tau Protein
At the heart of CBD pathology is the abnormal accumulation of tau protein in the brain. Tau proteins are essential for the stabilization of microtubules in nerve cells, but in CBD and other tauopathies, these proteins become defective and accumulate in an abnormal form. This accumulation leads to the formation of neurofibrillary tangles, which disrupt cell function and contribute to the neurodegenerative process. The connection between tauopathies and neurodegenerative diseases is well-established, with tau abnormalities being a hallmark of several conditions, including Alzheimer’s disease.
Understanding how tau protein abnormalities contribute to CBD is crucial for developing effective treatments. By unraveling the mechanisms by which tau dysfunction leads to neurodegeneration, researchers can target these pathways with therapies aimed at preventing or slowing the progression of the disease.
However, the causes of Corticobasal Degeneration are multifaceted, involving a complex interplay between genetic predispositions, potential environmental triggers, and the pathological role of tau protein accumulations. Despite the challenges in pinpointing the exact causes, ongoing research continues to make strides in unraveling the mysteries of CBD, offering hope for future therapeutic advancements.
Risk Factors of Corticobasal Degeneration
Corticobasal Degeneration (CBD) is a rare, progressive neurodegenerative disorder that primarily affects the brain’s cortex and basal ganglia, leading to a range of neurological symptoms. While the exact causes of CBD are still under investigation, understanding its risk factors can offer insights into who is more likely to develop this condition. This article delves into the two primary risk factors associated with CBD: age and possible links to other neurological conditions.
Age as a Primary Risk Factor
Age stands out as the most significant risk factor for Corticobasal Degeneration. The condition predominantly affects adults in their mid-60s and older, with a very low incidence rate in younger populations. The aging process itself is thought to contribute to the likelihood of developing CBD, as it may involve the accumulation of abnormal proteins in the brain or the decline in the brain’s natural repair mechanisms. Recognizing age as a key risk factor is crucial for early detection and management of the disease, although CBD remains rare even among older adults.
Possible Links to Other Neurological Conditions
Research into Corticobasal Degeneration has also explored its possible connections with other neurological disorders, suggesting that individuals with a history of certain conditions may be at an increased risk. These conditions include:
- Parkinson’s Disease and Parkinsonian Syndromes: Given CBD’s similarity to Parkinson’s in terms of motor symptoms, some studies suggest a potential overlap in their underlying pathological mechanisms.
- Alzheimer’s Disease: There is some evidence to suggest that individuals with Alzheimer’s may have an increased susceptibility to developing symptoms similar to those of CBD, due to shared pathological features like tau protein accumulation.
- Frontotemporal Dementia: CBD and frontotemporal dementia share clinical features, particularly in terms of cognitive and behavioral changes, indicating a possible link.
It’s important to note, however, that these connections are based on observational studies and do not imply a direct causation. The relationship between CBD and other neurological disorders remains a complex area of research, with ongoing studies aimed at uncovering more definitive links.
In sum, while Corticobasal Degeneration remains a challenging condition with much still to learn, recognizing and addressing its risk factors can play a key role in enhancing the quality of life for those affected.
Diagnosing Corticobasal Degeneration
This section aims to shed light on the intricacies of diagnosing CBD, highlighting the challenges faced, the diagnostic criteria and methods employed, and the importance of differential diagnosis in distinguishing CBD from other similar neurodegenerative conditions.
Challenges in Diagnosing CBD
One of the primary hurdles in diagnosing CBD is its symptomatic overlap with other neurodegenerative diseases such as Parkinson’s disease, progressive supranuclear palsy, and Alzheimer’s disease. Symptoms can vary widely among patients and may include motor impairments, cognitive dysfunction, and speech difficulties. This variability not only complicates the diagnosis process but also leads to a high risk of misdiagnosis.
Another challenge is the absence of a singular test that can definitively diagnose CBD. Currently, diagnosis is primarily based on clinical assessment and the exclusion of other conditions, which requires a comprehensive understanding of the disorder and its manifestations.
Diagnostic Criteria and Methods
To navigate the complexities of diagnosing CBD, healthcare professionals rely on a combination of diagnostic criteria and advanced imaging techniques. The diagnostic process typically involves:
- MRI (Magnetic Resonance Imaging): MRI scans are crucial for identifying structural changes in the brain that are indicative of CBD. These may include atrophy in specific regions such as the cerebral cortex and basal ganglia.
- PET (Positron Emission Tomography) Scans: PET scans can provide valuable insights into the brain’s metabolic activity, helping to differentiate CBD from other disorders by highlighting areas of reduced glucose metabolism.
- Clinical Assessments: A thorough clinical evaluation is essential for diagnosing CBD. This includes a detailed patient history, neurological examinations, and assessments of motor and cognitive functions. The aim is to document the presence of hallmark symptoms such as limb rigidity, apraxia (difficulty with motor planning), and cognitive impairment.
Differential Diagnosis
Differential diagnosis plays a pivotal role in the accurate identification of CBD. It involves distinguishing CBD from other neurodegenerative disorders with similar symptoms. This process is critical, as it ensures that patients receive the correct diagnosis and, consequently, the most appropriate care and management for their condition.
Healthcare professionals must consider a range of factors, including the pattern of symptom progression, the presence of specific clinical features, and imaging findings. A nuanced understanding of CBD and related disorders is essential for making an accurate differential diagnosis.
The diagnosis of Corticobasal Degeneration is fraught with challenges, from the variability of symptoms to the overlap with other neurodegenerative diseases. The use of advanced imaging techniques, alongside careful clinical assessment and a thorough differential diagnosis process, is essential for accurately identifying CBD. As research progresses, it is hoped that more definitive diagnostic criteria and methods will be developed, improving outcomes for those affected by this complex condition.
Treatment and Management of Corticobasal Degeneration
Currently, there is no cure for CBD, and treatments primarily focus on managing symptoms and improving the quality of life for those affected. This article outlines the current treatment options, the importance of physical and occupational therapy, and the role of medication and ongoing research in the search for potential treatments.
Current Treatment Options: Managing Symptoms
The cornerstone of managing corticobasal degeneration involves a personalized approach to alleviate specific symptoms. Given the complexity and variability of CBD, treatment plans often require adjustments and close monitoring by healthcare professionals. Symptom management may include:
- Physical Therapy: Aimed at improving mobility, balance, and coordination, physical therapy is crucial for maintaining movement and reducing the risk of falls. Therapists may also introduce exercises to enhance muscle strength and flexibility, which can help manage spasticity and rigidity, common symptoms of CBD.
- Occupational Therapy: This focuses on promoting independence in daily activities. Occupational therapists work with patients to adapt their living environments, recommend assistive devices, and develop strategies to overcome difficulties with tasks such as dressing, eating, and personal care.
- Speech and Language Therapy: For those experiencing speech difficulties or dysphagia (trouble swallowing), speech and language therapy can be beneficial. Therapists provide techniques to improve speech clarity and recommend dietary adjustments or feeding methods to ensure safe swallowing.
Role of Medication
While there is no medication that directly targets the underlying causes of corticobasal degeneration, certain drugs can help manage symptoms. For example:
- Parkinsonian Symptoms: Medications commonly used for Parkinson’s disease, like levodopa, may offer temporary relief for some CBD symptoms, such as rigidity and tremors, although their effectiveness varies widely among patients.
- Cognitive and Behavioral Symptoms: Antidepressants or medications designed to treat Alzheimer’s disease may be prescribed to address cognitive decline, mood swings, or behavioral changes.
Research on Potential Treatments
Research into corticobasal degeneration is ongoing, with scientists exploring various avenues to find effective treatments. This includes:
- Clinical Trials: Investigating new medications or therapeutic approaches that might slow the progression of CBD or improve symptoms. Participation in clinical trials also provides patients access to cutting-edge treatments and contributes to the broader understanding of the disease.
- Genetic and Molecular Studies: Aiming to uncover the genetic and molecular mechanisms underlying CBD, which could lead to the development of targeted therapies.
- Stem Cell Research: Exploring the potential of stem cells to regenerate or repair damaged brain cells, offering hope for future treatments.
However, while the current treatment landscape for corticobasal degeneration primarily focuses on symptom management, the combination of physical, occupational, and speech therapies, alongside symptom-specific medications, plays a critical role in enhancing the quality of life for those affected. Ongoing research into the causes and potential treatments of CBD is vital, offering hope for future breakthroughs in the management of this challenging condition.
Living with Corticobasal Degeneration
Living with Corticobasal Degeneration (CBD) presents unique challenges and impacts on the quality of life for both patients and their families. This progressive neurological disorder, characterized by movement difficulties, cognitive decline, and a range of other symptoms, necessitates a comprehensive support system and access to dedicated resources and communities. The journey with CBD requires resilience, understanding, and a proactive approach to manage its complexities.
Impact on Quality of Life
Corticobasal Degeneration significantly alters the daily lives of those affected. As the disease progresses, simple tasks become increasingly challenging, affecting independence and leading to frustration and emotional distress. Symptoms such as limb rigidity, difficulty in speaking, and cognitive impairment contribute to a decreased quality of life. Patients may experience social isolation due to physical limitations and changes in their ability to communicate effectively.
Understanding the emotional and physical toll of CBD is crucial for both patients and caregivers. Acknowledging the changes and challenges is the first step toward adapting and finding joy in new ways, despite the constraints of the condition.
Support Systems: Family Support and Caregiving
The role of family support and caregiving cannot be overstated in the context of living with CBD. Caregivers, often family members, play a pivotal role in providing daily care, emotional support, and advocating for the needs of the patient. This journey, while rewarding, can also be physically and emotionally taxing for caregivers. It’s important for caregivers to seek support, take breaks, and care for their own well-being to sustain the level of care their loved one needs.
Families can enhance the quality of life for a person with CBD by creating a supportive home environment, facilitating access to medical care, and encouraging social interaction within the limits of the patient’s abilities. Open communication within the family and with healthcare professionals is essential to navigate the challenges and make informed decisions about care and treatment options.
Resources and Communities for Patients and Families
Fortunately, there are numerous resources and communities dedicated to supporting patients with Corticobasal Degeneration and their families. National and international organizations offer information on the latest research, treatment options, and strategies for managing symptoms. Many of these organizations also provide platforms for connecting with others through support groups, forums, and social media channels, offering a sense of community and shared understanding.
Accessing these resources can empower patients and caregivers with knowledge, practical advice, and emotional support. It’s beneficial to explore:
- Educational Materials: Understand CBD’s symptoms, progression, and management strategies.
- Support Groups: Connect with others who are navigating similar challenges, share experiences, and offer mutual support.
- Therapy and Rehabilitation Services: Engage with professionals who can tailor therapies to improve quality of life and maintain independence for as long as possible.
- Legal and Financial Planning Assistance: Prepare for the future with guidance on decision-making, healthcare directives, and financial planning to ensure long-term care needs are met.
Living with Corticobasal Degeneration is undeniably challenging, but with the right support systems, resources, and a community of understanding individuals, patients and their families can navigate this journey with dignity and resilience. By focusing on quality of life, maintaining connections, and accessing available resources, it’s possible to face the challenges of CBD with strength and hope.
Conclusion
For individuals and families navigating the complexities of CBD, seeking professional medical advice is paramount. Healthcare professionals specializing in neurodegenerative diseases can provide comprehensive care, support, and guidance tailored to each individual’s unique situation. They can also connect patients and caregivers with resources and support networks that can make a significant difference in managing the challenges of the disease.
In conclusion, while CBD presents significant hurdles, the ongoing research and support from the medical community offer hope and resources for those affected. Encouragement and advocacy for professional consultation and care are essential in navigating this condition. The road ahead may be challenging, but with continued advancements in research and a supportive care network, there is reason to remain hopeful for the future.