Congenital Myasthenic Syndromes Treatment: Congenital Myasthenic Syndromes (CMS) are a group of rare genetic disorders that impair the transmission of signals between nerves and muscles, leading to muscle weakness and fatigue.
Unlike myasthenia gravis, which is acquired and autoimmune, CMS is inherited and presents symptoms from birth or early childhood. Understanding CMS is crucial for timely diagnosis and effective treatment.
What is Congenital Myasthenic Syndromes
Congenital Myasthenic Syndromes (CMS) are a group of inherited neuromuscular disorders characterized by muscle weakness that worsens with physical exertion. Unlike Myasthenia Gravis, which is an autoimmune condition, CMS results from genetic mutations affecting the communication between nerve cells and muscles. This disruption in neuromuscular transmission leads to symptoms such as muscle fatigue, weakness, and in some cases, respiratory issues. Early diagnosis and treatment are crucial for managing symptoms and improving quality of life.
Types of CMS and Their Characteristics
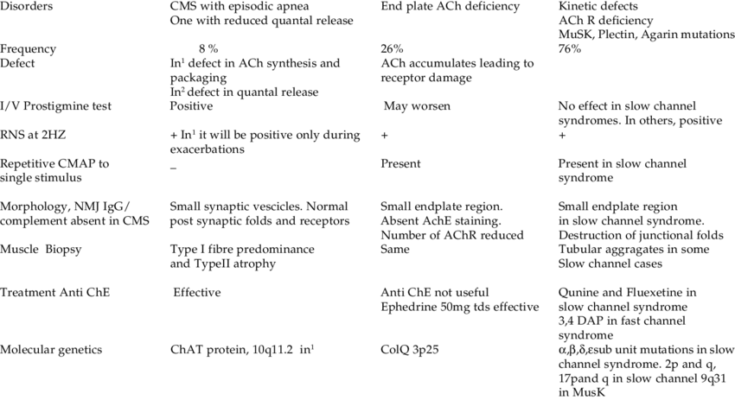
CMS is categorized into several types, each with distinct genetic causes and clinical manifestations:
- Presynaptic CMS involves defects in the nerve ending, affecting the release of acetylcholine, a neurotransmitter essential for muscle contraction. Symptoms often include weakness and fatigability.
- Synaptic CMS is characterized by abnormalities in the space between nerve and muscle cells, impacting the efficiency of neurotransmitter transmission.
- Postsynaptic CMS results from mutations affecting the muscle cell receptors that bind to acetylcholine. This type is more common and presents with muscle weakness that can improve with rest.
Each type of CMS manifests differently, affecting various muscle groups and leading to a range of symptoms from mild to severe.
The Genetic Basis of CMS and Inheritance Patterns
CMS is caused by mutations in genes critical for neuromuscular junction function. These mutations can be inherited in various patterns, including autosomal dominant, autosomal recessive, or sometimes X-linked, depending on the specific gene involved. For example, mutations in the CHRNE gene, responsible for encoding acetylcholine receptor subunits, typically follow an autosomal recessive pattern, meaning a child must inherit one mutated gene from each parent to develop the condition.
Prevalence and Impact on Quality of Life
CMS is a rare condition, with its prevalence varying widely among different populations. The impact on quality of life can be significant, affecting physical abilities, respiratory function, and daily activities. However, with appropriate treatment, which may include medications like cholinesterase inhibitors or immunosuppressants, and supportive therapies, individuals with CMS can lead active and fulfilling lives. Early intervention and personalized care plans are essential for managing symptoms and improving outcomes.
However, understanding CMS’s complexities, from its genetic underpinnings to its diverse clinical presentations, is crucial for healthcare providers, patients, and families. Advancements in genetic testing and therapies continue to improve diagnosis and treatment options, offering hope to those affected by this challenging condition.
Symptoms and Early Signs of Congenital Myasthenic Syndromes (CMS)
Here, we’ll discuss the common symptoms associated with CMS, early signs that may indicate the presence of the condition, and the variability of symptoms among different types of CMS.
Common Symptoms Associated with CMS
The symptoms of Congenital Myasthenic Syndromes primarily involve muscle weakness that worsens with physical activity and improves with rest. Key symptoms include:
- Muscle Weakness and Fatigue: Most individuals experience weakness in the muscles used for movement (skeletal muscles), particularly in the eyes, face, and limbs. This can lead to droopy eyelids, difficulty swallowing, and generalized fatigue.
- Respiratory Issues: Some forms of CMS affect the respiratory muscles, leading to breathing difficulties, especially during sleep or respiratory infections.
- Delayed Motor Milestones: Children with CMS may show delays in reaching developmental milestones such as sitting, standing, or walking.
- Episodes of Weakness: Sudden episodes of muscle weakness can be triggered by infections, fever, or stress.
Early Signs That May Indicate CMS
Early detection of CMS is vital for effective treatment and management. Signs that may suggest a diagnosis of CMS include:
- Persistent Muscle Weakness: Unlike typical fatigue, muscle weakness in CMS does not resolve with rest and is often more pronounced towards the end of the day.
- Frequent Falls or Difficulty Climbing Stairs: Young children may frequently fall or exhibit an inability to keep up with peers during physical activities.
- Difficulty with Eye Movements and Facial Expressions: Struggles with keeping eyes open, smiling, or swallowing can be early indicators of CMS.
Variability of Symptoms Among Different Types of CMS
CMS encompasses a variety of syndromes, each with its genetic cause and symptom profile. The variability of symptoms among these types can influence the onset, severity, and progression of the condition:
- Age of Onset: Symptoms can appear at any age, from infancy to adulthood, depending on the type of CMS.
- Severity and Progression: Some forms of CMS present with mild symptoms that remain stable over time, while others may experience a progressive worsening of muscle weakness.
- Response to Treatment: The effectiveness of treatments, such as cholinesterase inhibitors, varies significantly among different CMS types, with some individuals showing marked improvement and others experiencing minimal benefit.
However, understanding the diverse symptoms and early signs of Congenital Myasthenic Syndromes is essential for prompt and accurate diagnosis. Early intervention and tailored treatment plans can significantly improve the quality of life for individuals with CMS. Awareness of the variability among different types of CMS is also crucial for managing expectations and optimizing care strategies.
Treatment Options for Congenital Myasthenic Syndromes
Treatment plans are tailored to each individual, taking into account the specific type of CMS and the severity of symptoms. Below, we outline the general approach to CMS treatment, including pharmacological and non-pharmacological options, as well as lifestyle adjustments and supportive care.
General Approach to CMS Treatment
The cornerstone of managing CMS involves a comprehensive evaluation to accurately diagnose the specific subtype, as treatments can vary significantly. A multidisciplinary team, including neurologists, geneticists, and physical therapists, often collaborates to develop a personalized treatment plan. Regular follow-ups are crucial to monitor the condition and adjust treatments as needed.
Pharmacological Treatments
- Cholinesterase Inhibitors: These drugs, such as pyridostigmine, are often the first line of treatment. They work by increasing communication between nerves and muscles, improving muscle strength.
- Immunosuppressants: For some types of CMS, particularly those with an autoimmune component, medications like prednisone, azathioprine, or mycophenolate mofetil may be used to suppress the immune system.
- Quinidine and Fluoxetine: In cases involving the slow-channel syndrome subtype of CMS, these medications can help by blocking excessive ion channel activity in the neuromuscular junction.
- Ephedrine and Albuterol: These stimulants can be effective in certain CMS subtypes by enhancing the release of acetylcholine, a neurotransmitter that stimulates muscle contraction.
Non-Pharmacological Treatments
- Physical Therapy: Tailored exercise programs can help maintain muscle strength and mobility, and prevent contractures.
- Occupational Therapy: This focuses on improving daily living skills and adapting the environment to enhance independence and safety.
- Speech Therapy: For those with bulbar muscle weakness affecting speech and swallowing, speech therapists can offer strategies to manage these issues.
Lifestyle Adjustments and Supportive Care
- Diet and Nutrition: A balanced diet, sometimes with adjustments to manage swallowing difficulties, is essential. Nutritional supplements may be recommended in some cases.
- Assistive Devices: Tools like braces, walkers, or wheelchairs can help maintain mobility and independence.
- Energy Conservation: Learning to balance activity with rest periods can prevent fatigue and manage energy levels more effectively.
- Emotional and Social Support: Living with CMS can be challenging, making support from family, friends, and support groups vital. Psychological counseling may also be beneficial for dealing with the emotional aspects of chronic illness.
However, while CMS presents a variety of challenges, a comprehensive and personalized treatment plan can significantly improve the lives of those affected. Ongoing research and advances in genetic understanding may offer new treatment avenues in the future. Regular consultations with healthcare providers ensure that treatment strategies evolve with the latest findings and the individual’s changing needs.
Advances in Congenital Myasthenic Syndromes Treatment
The field of medical research continually evolves, bringing forth new insights and innovations. Particularly, the treatment of Congenital Myasthenic Syndromes (CMS) has seen significant advancements, thanks to recent research and the development of emerging therapies. This article delves into the latest progress in CMS treatment, highlighting gene therapy and the pivotal role of clinical trials.
Recent Research and Emerging Therapies
The journey toward understanding and treating CMS has been accelerated by recent research efforts. Scientists have made groundbreaking discoveries regarding the genetic mutations responsible for CMS, leading to the development of targeted therapies. These emerging therapies are designed to correct the underlying genetic defects, offering hope for more effective treatment options. One notable advancement is the use of cholinesterase inhibitors, which have shown promise in improving neuromuscular transmission in some patients.
Gene Therapy and Future Prospects
Gene therapy stands at the forefront of future prospects for CMS treatment. This innovative approach involves correcting or replacing the faulty genes responsible for the syndrome. The potential of gene therapy is immense, offering a long-term solution that could address the root cause of CMS. Although still in the early stages of research, preliminary trials have demonstrated the feasibility of gene delivery systems targeting muscle cells, paving the way for future clinical applications.
The Importance of Clinical Trials for CMS Treatment
Clinical trials play a crucial role in the advancement of CMS treatment. These studies are essential for testing the safety and efficacy of new therapies before they are made available to the public. Clinical trials also offer insights into the disease mechanisms and the potential side effects of treatments. Participation in clinical trials not only contributes to scientific knowledge but also provides patients with access to the latest treatment options. It is through these rigorous studies that the medical community can validate the effectiveness of emerging therapies, ensuring that they meet the highest standards of care.
As the landscape of CMS treatment continues to evolve, the emphasis on research, gene therapy, and clinical trials underscores a commitment to improving the lives of those affected by this challenging condition. The progress made thus far inspires optimism for the future, with the promise of more effective and personalized treatment strategies on the horizon.
Living with Congenital Myasthenic Syndromes
Living with Congenital Myasthenic Syndromes (CMS) presents unique challenges that require effective management strategies and strong support systems. Individuals diagnosed with CMS, a rare neuromuscular disorder, often face difficulties in daily life and activities due to muscle weakness. This article aims to guide those living with CMS and their loved ones on managing daily life, leveraging support systems, and navigating educational and occupational considerations.
Managing Daily Life and Activities
Living with CMS means adapting your lifestyle to accommodate varying degrees of muscle weakness. Here are some strategies to help manage daily life:
- Personalized Routine: Tailor your daily activities according to your energy levels. It’s important to recognize when you’re most energetic and plan tasks that require more physical effort during these times.
- Energy Conservation: Learn to conserve energy by breaking down tasks into smaller, manageable steps and taking regular breaks. Using assistive devices can also help reduce fatigue.
- Physical Therapy: Engage in physical therapy designed for CMS patients. These exercises can help improve muscle strength and mobility without overexertion.
- Nutrition and Hydration: A balanced diet and adequate hydration are crucial. Some individuals may benefit from dietary adjustments that can help manage symptoms.
Support Systems: Family, Community, and Online Resources
Having a robust support system is vital for individuals with CMS. It provides emotional, physical, and informational support.
- Family Support: Open communication with family members is essential. Educating them about CMS can help them understand your daily challenges and how they can assist.
- Community Resources: Connect with local support groups and health services. These resources can provide practical advice, emotional support, and opportunities to engage with others facing similar challenges.
- Online Resources: The internet is a rich source of information and support. Online forums, social media groups, and websites dedicated to CMS can offer advice, share experiences, and foster a sense of belonging.
Educational and Occupational Considerations
Navigating education and work with CMS requires planning and communication.
- Educational Support: Schools and universities often have services for students with disabilities. These might include modified exam arrangements, note-taking services, and customized learning plans. It’s important to communicate your needs early and work closely with educational staff.
- Occupational Considerations: Workplace accommodations can make a significant difference. Discuss with your employer the possibility of flexible working hours, telecommuting options, or ergonomic workplace adjustments to suit your physical needs.
Living with Congenital Myasthenic Syndromes certainly has its challenges, but with the right strategies and support, individuals can lead fulfilling lives. Embracing a proactive approach towards managing daily activities, tapping into the strength of support systems, and making informed educational and occupational choices are key steps in navigating life with CMS.
Frequently Asked Questions (FAQ) about Congenital Myasthenic Syndromes
What are Congenital Myasthenic Syndromes (CMS)?
Congenital Myasthenic Syndromes (CMS) are a group of genetic disorders that lead to muscle weakness and fatigue. These conditions are caused by mutations in genes that are essential for the communication between nerves and muscles. Unlike Myasthenia Gravis, which is an autoimmune disorder, CMS is inherited and present from birth.
How are CMS diagnosed?
Diagnosis of CMS involves a combination of clinical evaluation, family history, and specialized tests. These may include genetic testing to identify specific mutations, electromyography (EMG) to assess muscle response to nerve stimulation, and blood tests. A thorough evaluation by a neurologist specializing in neuromuscular disorders is essential for accurate diagnosis.
What are the symptoms of CMS?
Symptoms of CMS can vary widely but generally include muscle weakness that worsens with activity and improves with rest, droopy eyelids, difficulty swallowing or speaking, and respiratory issues. The severity and range of symptoms can differ greatly among individuals, even those with the same genetic mutation.
Is there a cure for CMS?
While there is no cure for CMS, treatments are available to manage symptoms and improve quality of life. These may include medications to enhance neuromuscular transmission, immunosuppressants (in some cases), physical therapy to maintain muscle strength and mobility, and respiratory support for those with breathing difficulties.
Can CMS be inherited?
Yes, CMS is an inherited disorder, meaning it is passed down from parents to their children. The pattern of inheritance can be autosomal dominant, autosomal recessive, or, less commonly, X-linked, depending on the specific genetic mutation involved.
Are there different types of CMS?
Yes, there are several types of CMS, classified based on the genetic mutation and the part of the neuromuscular junction affected. These include presynaptic, synaptic, and postsynaptic CMS, each with its own set of characteristics and response to treatment.
How common is CMS?
CMS is considered a rare disorder, though its exact prevalence is difficult to determine due to its varied presentation and the possibility of undiagnosed cases. It is less common than autoimmune myasthenia gravis.
What research is being done on CMS?
Research on CMS is ongoing, with scientists studying the genetics of the disorder, exploring new treatment options, and conducting clinical trials for potential therapies. Advances in genetic testing and therapies offer hope for better management and understanding of CMS in the future.
Can lifestyle changes help manage CMS symptoms?
While lifestyle changes cannot cure CMS, they can help manage symptoms. Regular, moderate exercise tailored to individual capabilities can maintain muscle strength and function. Adequate rest, stress management, and a balanced diet can also play supportive roles in managing the condition.
Where can I find support and more information about CMS?
Support for individuals and families affected by CMS can be found through neuromuscular disease organizations, online support groups, and healthcare providers specializing in neuromuscular disorders. These resources can provide valuable information, support networks, and access to specialized care and research opportunities.
Conclusion:
The journey towards a better understanding and management of CMS is far from over. Continued research is essential for uncovering the mysteries of CMS and developing new treatments. It is through the dedication of the medical community and the support of patient advocacy groups that progress is made. Families affected by CMS, along with healthcare providers, are encouraged to participate in research studies and support networks, contributing to the collective effort to combat these complex disorders.
The path forward for CMS treatment is promising, marked by groundbreaking discoveries and an unwavering commitment to improving patient outcomes. As we embrace the evolving landscape of CMS treatment, let us remain steadfast in our support for ongoing research and the development of innovative therapies. Together, we can forge a future where Congenital Myasthenic Syndromes are no longer an insurmountable challenge, but a condition with a range of effective treatments and a hopeful outlook.
In conclusion, our understanding and ability to treat Congenital Myasthenic Syndromes have grown significantly, yet the journey ahead remains filled with opportunities for discovery and improvement. By continuing to push the boundaries of science and medicine, we can look forward to a future where CMS patients can lead fuller, healthier lives.