Congenital Heart Defects in Children Symptoms: Congenital heart defects (CHDs) are the most common type of birth defect, affecting millions of newborns worldwide.
These conditions involve abnormalities in the heart’s structure that are present from birth, significantly impacting the heart’s ability to function normally.
Understanding the symptoms and causes of congenital heart defects in children is crucial for early detection, treatment, and management, ensuring affected children can lead healthier lives.
What Are Congenital Heart Defects?
Congenital Heart Defects (CHDs) represent a group of abnormalities in the heart’s structure that are present from birth. These defects can affect the walls of the heart, the heart valves, and the arteries and veins near the heart. They range in severity from simple problems, such as a small hole in the heart that may heal on its own, to complex issues that require surgical intervention shortly after birth.
Prevalence and Significance of CHDs in Children
CHDs are the most common type of birth defect, affecting approximately 1% of newborns in the United States each year. This translates to about 40,000 infants born with a heart defect annually. The significance of CHDs cannot be overstated, as they are a leading cause of birth defect-associated infant illness and death. However, advancements in medical and surgical treatments have significantly improved the survival rate and quality of life for children with these heart defects. Early detection and treatment are crucial for managing CHDs effectively, making prenatal screening and postnatal monitoring essential components of care.
Different Types of Congenital Heart Defects
There are many different types of CHDs, ranging from simple to complex conditions. Here are some of the most common types:
- Atrial Septal Defect (ASD): A hole in the wall between the two upper chambers of the heart (atria), allowing oxygen-rich blood to mix with oxygen-poor blood.
- Ventricular Septal Defect (VSD): A hole in the wall separating the two lower chambers of the heart (ventricles), which can cause the heart to work harder and lead to heart failure if not treated.
- Tetralogy of Fallot (ToF): A complex heart defect that involves four heart problems, including a VSD, pulmonary stenosis, right ventricular hypertrophy, and an overriding aorta.
- Patent Ductus Arteriosus (PDA): A condition where the ductus arteriosus, a blood vessel in a baby’s heart, fails to close and results in blood flowing directly from the aorta into the pulmonary artery.
- Coarctation of the Aorta (CoA): A narrowing of the major artery (the aorta) that carries blood to the body, which can cause high blood pressure and damage to the heart.
- Pulmonary Atresia: A malformation where the pulmonary valve does not form properly, affecting the flow of blood from the heart to the lungs to pick up oxygen.
Each type of CHD has its specific symptoms, treatment options, and outlook. The management of these conditions often requires a multidisciplinary approach, including cardiology, pediatric surgery, and often lifelong follow-up with specialized care. With the advancements in medical science, most children with CHDs go on to live healthy, productive lives. It’s essential for parents and caregivers to work closely with a healthcare team to ensure the best possible outcomes for their child.
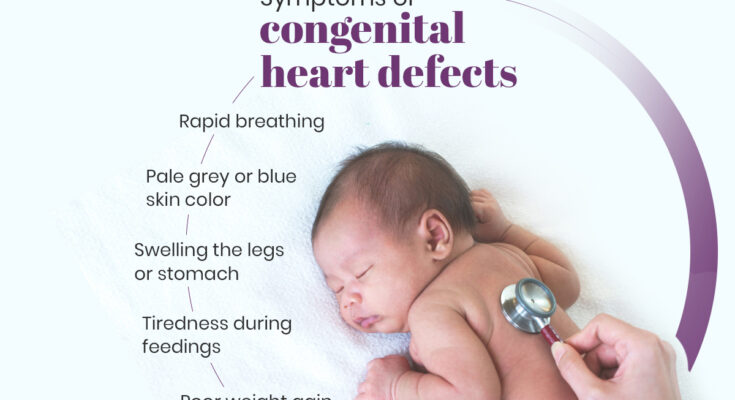
Symptoms of Congenital Heart Defects in Children
Understanding these signs is crucial for early diagnosis and timely intervention. This article delves into the general symptoms of CHDs, highlights age-specific symptoms distinguishing newborns from older children, and explains how these symptoms relate to different types of CHDs.
General Symptoms
Children with congenital heart defects may exhibit a range of general symptoms that indicate the heart isn’t functioning effectively. These include:
- Rapid breathing or breathlessness, especially during feeding or physical activity.
- Cyanosis, a bluish tint to the skin, lips, and fingernails, signaling a lack of oxygen in the blood.
- Fatigue, which is often more noticeable during times of increased activity.
- Poor weight gain, as feeding difficulties or increased energy expenditure can affect growth.
- Sweating, particularly around the head, even when the child is not engaging in physical activity.
Age-Specific Symptoms
Newborns with congenital heart defects may show signs shortly after birth, including:
- Difficulty breathing, which may be observed as grunting or nostril flaring.
- Poor feeding, as they may become quickly tired during feeds or have difficulty breathing while feeding.
- Excessive sleepiness, indicating that they may not have the energy for feeding or staying awake due to reduced oxygen levels.
Older children might display symptoms that include:
- Shortness of breath during play or physical activities.
- Difficulty in keeping up with their peers during play due to fatigue or breathlessness.
- Frequent respiratory infections or conditions like pneumonia, which can be exacerbated by underlying CHDs.
Symptoms and Their Relation to Different Types of CHDs
The symptoms a child experiences can often give clues about the type of congenital heart defect they have. For instance:
- Cyanotic CHDs, such as Tetralogy of Fallot or transposition of the great arteries, often cause a bluish skin color due to poorly oxygenated blood circulating through the body.
- Acyanotic CHDs, like ventricular or atrial septal defects, might not lead to cyanosis but can cause symptoms like rapid breathing, fatigue, and poor weight gain due to the heart working harder to pump blood.
Understanding these symptoms and their connection to specific types of CHDs is essential for healthcare providers to diagnose and manage these conditions effectively. Early detection and treatment can significantly improve the quality of life for children with congenital heart defects.
However, recognizing the signs of congenital heart defects in children, whether general, age-specific, or related to specific CHD types, is crucial for early intervention. Parents and caregivers should seek medical advice if they notice any concerning symptoms, as early diagnosis and management can lead to better outcomes for affected children.
Causes of Congenital Heart Defects in Children
Understanding the causes of congenital heart defects is crucial for expecting parents, healthcare providers, and researchers. These causes can be broadly categorized into genetic factors, environmental influences, and a combination of both.
Genetic Factors and Heredity
Genetics play a significant role in the development of congenital heart defects. Some heart defects are passed down through families, indicating a hereditary component. These genetic links can be due to changes in a single gene or multiple genes. Sometimes, a congenital heart defect is a part of genetic syndromes, such as Down syndrome, Turner syndrome, and Marfan syndrome, where the heart defect is one of several other health issues affected by genetic abnormalities.
Environmental Influences
The environment in which an expecting mother lives and the lifestyle choices she makes can also impact the heart development of the fetus. Several environmental factors have been identified:
- Maternal Illnesses: Certain conditions during pregnancy, such as diabetes (not well controlled), lupus, and rubella (German measles), have been linked to an increased risk of CHDs in newborns.
- Medications: Taking certain medications during pregnancy, including some for acne (like isotretinoin), mood disorders, and epilepsy, can increase the risk of congenital heart defects.
- Lifestyle Choices: Lifestyle factors such as smoking, drinking alcohol, and using illegal drugs during pregnancy can significantly elevate the risk of having a child with a CHD.
Combination of Genetic and Environmental Factors
In many cases, congenital heart defects result from a combination of genetic predispositions and environmental exposures. This means that even if a genetic tendency towards heart defects exists, exposure to certain environmental factors during pregnancy can increase the likelihood of these defects developing. Conversely, a baby with no genetic predisposition to heart defects could still develop them due to significant environmental exposures.
Understanding the multifaceted causes of congenital heart defects can help in prevention efforts and guiding research into new treatments. Expecting parents concerned about CHDs should consult with healthcare providers for genetic counseling and advice on minimizing environmental risks during pregnancy.
However, congenital heart defects in children can stem from genetic factors, environmental influences, or a mix of both. Awareness and understanding of these causes are essential for reducing risks and ensuring the health and well-being of future generations.
Diagnosing Congenital Heart Defects in Children
Early diagnosis is crucial for the effective management and treatment of these conditions. This article explores the common diagnostic tests and procedures for CHDs, the role of prenatal screening, and the importance of early detection.
Common Diagnostic Tests and Procedures
Detecting congenital heart defects in children involves a series of tests and procedures designed to assess heart structure, function, and rhythm. These may include:
- Echocardiogram: This ultrasound test uses sound waves to create detailed images of the heart, allowing doctors to identify structural heart defects and assess heart function.
- Electrocardiogram (ECG or EKG): This test records the electrical activity of the heart, helping to diagnose heart rhythm issues and other heart problems.
- Chest X-ray: A chest X-ray can show the size and shape of a child’s heart and lungs, providing clues about the presence of a heart defect.
- Pulse Oximetry: A simple test that measures the oxygen level in the blood, indicating how well the heart is pumping oxygenated blood to the body.
- Cardiac MRI: A magnetic resonance imaging (MRI) test of the heart provides detailed images of the heart’s structure and can assess its function.
The Role of Prenatal Screening and Diagnosis
Prenatal screening plays a vital role in the early detection of congenital heart defects. Through various screening methods, such as fetal ultrasound and specialized echocardiograms, doctors can identify heart defects before a baby is born. Early diagnosis allows for better planning and management of the condition, including arranging for delivery in a facility equipped to care for babies with heart defects and early intervention strategies.
Importance of Early Detection in Management and Treatment
Early detection of congenital heart defects is critical for several reasons:
- Improved Outcomes: Early diagnosis and treatment can improve the overall health and well-being of children with CHDs, reducing the risk of complications later in life.
- Treatment Planning: Identifying a heart defect early allows healthcare providers to develop a comprehensive treatment plan, which may include medications, interventions like catheter procedures or surgery, and ongoing monitoring of heart health.
- Family Preparedness: Early detection gives families time to understand the condition, seek out specialists, and prepare for any necessary treatments or lifestyle adjustments.
However, diagnosing congenital heart defects in children involves a combination of prenatal screening and various diagnostic tests after birth. The early identification of these conditions is paramount in ensuring effective treatment and management, leading to better health outcomes for affected children. By understanding the importance of these diagnostic processes, parents and caregivers can take proactive steps towards the care and support of children with CHDs.
Treatment Options for Congenital Heart Defects (CHDs)
Here, we explore the treatment options available for CHDs, including non-surgical treatments, surgical interventions, and the importance of long-term management and care for children with these heart conditions.
Non-Surgical Treatments
For some children with CHDs, non-surgical treatments may be the first line of defense. These treatments are often used for minor defects that do not severely affect the heart’s function or for patients who are not candidates for surgery. Non-surgical options include:
- Medications: To help the heart work more efficiently or to treat symptoms associated with CHDs, such as medications to control heart rhythm, improve heart function, or prevent blood clots.
- Oxygen Therapy: For babies who have trouble getting enough oxygen due to their heart defect.
- Cardiac Catheterization: A minimally invasive procedure that can be used to diagnose or treat certain heart defects. During this procedure, a thin tube is inserted into a vein or artery and guided to the heart, allowing doctors to perform repairs or observe heart function without open surgery.
Surgical Interventions
When non-surgical treatments are not enough, surgery may be necessary to repair the heart defect. The type of surgery depends on the nature of the defect and the child’s overall health. Surgical options include:
- Open-heart Surgery: To repair structural defects, such as holes in the heart, valve problems, or narrow arteries.
- Heart Transplant: In rare cases, when a heart defect cannot be repaired, a heart transplant may be the only option. This involves replacing the child’s heart with a healthy one from a donor.
Long-term Management and Care
Managing a child’s CHD is a lifelong process. Even after successful treatment, regular medical follow-ups are crucial to monitor the child’s heart health and ensure the best possible outcome. Long-term care may include:
- Routine Check-ups: Regular visits to a cardiologist to monitor heart health and detect any changes or complications early.
- Lifestyle Adjustments: Encouraging a heart-healthy lifestyle, including a balanced diet, regular exercise, and avoiding smoking.
- Education: Educating the child and family about the CHD, its implications, and how to manage it effectively.
Advances in medical treatments and surgical techniques continue to improve the outcomes for these children, highlighting the importance of early diagnosis and treatment. By understanding the options available for treating CHDs, parents can collaborate with healthcare providers to ensure their child receives the best possible care.
Preventing Congenital Heart Defects
Congenital heart defects (CHDs) are the most common type of birth defect, affecting the structure of a baby’s heart and its function. While not all CHDs can be prevented, understanding potential preventive measures and staying informed about current research on prevention and early detection can help reduce the risk. This section explores actionable strategies and the latest scientific advancements aimed at preventing congenital heart defects.
Potential Preventive Measures
- Maternal Health Before and During Pregnancy: Maintaining a healthy lifestyle before and during pregnancy plays a crucial role in minimizing the risk of CHDs. This includes a balanced diet, regular exercise, and avoiding harmful substances such as alcohol, tobacco, and certain medications not recommended during pregnancy.
- Prenatal Vitamins and Folic Acid: Studies have shown that taking prenatal vitamins containing folic acid before conception and during early pregnancy can help prevent major birth defects, including some CHDs. A daily intake of 400 micrograms of folic acid is recommended for women of childbearing age.
- Managing Chronic Conditions: Women with chronic health issues such as diabetes or obesity should work closely with their healthcare providers to manage these conditions. Proper management of diabetes and maintaining a healthy weight before and during pregnancy can significantly reduce the risk of CHDs.
- Vaccinations: Staying up to date with vaccinations, including the flu shot and the COVID-19 vaccine, is important for pregnant women. Certain infections during pregnancy can increase the risk of birth defects.
- Environmental Factors: Avoiding exposure to harmful environmental factors such as certain pesticides, solvents, and air pollutants can also play a role in preventing CHDs. Pregnant women should consult their healthcare providers about safe work and home environments.
Current Research on Prevention and Early Detection
Research into the prevention and early detection of congenital heart defects is ongoing and focuses on several key areas:
- Genetic Studies: Scientists are exploring the genetic factors that contribute to CHDs. Understanding the genetic causes can lead to better prevention strategies and early detection methods.
- Early Ultrasound and Fetal Echocardiography: Advances in prenatal imaging allow for the early detection of CHDs. Early diagnosis through ultrasound and fetal echocardiography enables timely planning for interventions that can improve outcomes.
- Nutritional and Environmental Research: Ongoing studies aim to identify the role of nutrition, lifestyle, and environmental factors in the prevention of CHDs. This research includes the impact of specific nutrients, the effects of maternal obesity, and the influence of environmental toxins.
- Vaccine Development: Research is also focused on developing vaccines to prevent maternal infections that can lead to CHDs. Preventing these infections through vaccination could significantly reduce the risk of congenital heart defects.
Ongoing research into genetic, environmental, and lifestyle factors continues to offer new insights into the prevention and early detection of CHDs, holding promise for future generations. Parents-to-be and healthcare providers must work together to leverage these strategies and advancements to mitigate the impact of congenital heart defects.
Living with a Congenital Heart Defect
Living with a congenital heart defect (CHD) presents a unique set of challenges and impacts on a child’s life and development. However, with advancements in medical treatment and a strong support network, families and children can navigate these challenges successfully. This article explores the impact of CHD on children, the support available for families, and highlights success stories and advancements in treatment, offering hope and guidance for those affected.
Impact on the Child’s Life and Development
Children with congenital heart defects may face various challenges that can affect their physical, emotional, and social development. Depending on the severity of the condition, children might experience limitations in their ability to participate in certain activities, leading to feelings of isolation or difference from their peers. Additionally, frequent hospital visits and medical treatments can disrupt normal childhood experiences and education.
However, with proper medical care and support, many children with CHD can lead active and fulfilling lives. It’s crucial for parents and caregivers to foster an environment that encourages the child to explore their capabilities while being mindful of their limitations. Early intervention programs and individualized education plans (IEPs) can also support a child’s development and academic achievements, ensuring they receive the accommodations needed to thrive.
Support for Families and Children
Navigating the journey of a congenital heart defect is not something families have to do alone. A wealth of resources and support groups exist to provide emotional support, practical advice, and a sense of community. Hospitals and heart health organizations often offer connections to local and online support groups where families can share experiences and coping strategies.
Moreover, many charities and non-profit organizations provide financial assistance, educational resources, and advocacy for children with CHD and their families. These resources can be invaluable in helping families understand the condition, make informed decisions about care, and connect with other families who understand their experiences.
Success Stories and Advancements in Treatment
The field of pediatric cardiology has seen remarkable advancements in the treatment of congenital heart defects, leading to improved outcomes and quality of life for affected children. Minimally invasive procedures, innovative surgeries, and better post-operative care have significantly increased survival rates and reduced the impact of CHD on long-term health.
Success stories of individuals living with CHD serve as powerful testimonials to the resilience of the human spirit and the potential for a fulfilling life despite the condition. These stories also highlight the importance of research and development in medical science, offering hope for even greater improvements in treatment and care.
FAQs on Congenital Heart Defects in Children
What is a congenital heart defect?
A congenital heart defect (CHD) is a structural problem with the heart that is present at birth. These defects can affect the heart’s walls, valves, and blood vessels, and can range from simple issues that cause no symptoms to complex problems that require immediate medical attention.
How common are congenital heart defects?
Congenital heart defects are the most common type of birth defect. According to the Centers for Disease Control and Prevention (CDC), CHDs affect nearly 1% of—about 40,000—births per year in the United States. They are a leading cause of birth defect-associated infant illness and death.
What causes congenital heart defects?
The exact cause of most congenital heart defects is unknown. However, some factors that may increase the risk include genetic conditions (like Down syndrome), taking certain medications during pregnancy, maternal diabetes, smoking, and viral infections during the first trimester of pregnancy.
How are congenital heart defects diagnosed?
CHDs can often be detected through fetal ultrasound before birth. After birth, they might be identified through physical examinations, echocardiograms, chest X-rays, or pulse oximetry screening. Early diagnosis is crucial for managing and treating these conditions effectively.
Can congenital heart defects be treated?
Yes, many congenital heart defects can be treated with surgery, catheter procedures, or medications. The treatment depends on the type and severity of the defect. Some children with minor defects may not need any treatment, but they should be regularly monitored by a healthcare professional.
Will my child lead a normal life?
Many children with congenital heart defects grow up to lead active, healthy lives. The outlook depends on the specific defect and its severity. Ongoing care from a team of heart specialists will help manage health issues and support a good quality of life.
Are congenital heart defects preventable?
While not all congenital heart defects can be prevented, you can take steps to lower the risks. These include getting proper prenatal care, avoiding harmful substances during pregnancy, and managing chronic illnesses effectively. Genetic counseling may be recommended for families with a history of CHDs or other genetic conditions.
Should children with congenital heart defects be physically active?
Physical activity is important for children with CHDs, but the level and type of activity should be discussed with a healthcare provider. Some children may need to limit certain activities, while others may be encouraged to be as active as possible.
Conclusion:
As we conclude, let’s echo a call to action for increased awareness and early diagnosis of congenital heart defects. It’s through our collective efforts in education, research, and support that we can make a substantial impact. Let us advocate for routine screenings, share knowledge on the signs and symptoms of CHD, and champion the cause in our communities. Together, we can pave the way for brighter futures for children affected by congenital heart defects, ensuring they receive the care and attention necessary for a thriving life.
Recognizing the symptoms and causes of congenital heart defects is more than a medical necessity; it’s a societal imperative that calls for our unwavering attention and action. Let’s stand in solidarity with affected families, bolster ongoing research, and strive for a world where every child has the opportunity to lead a heart-healthy life.