Congenital Diaphragmatic Hernia Symptoms: Congenital Diaphragmatic Hernia (CDH) is a serious medical condition present at birth that affects the diaphragm, the muscle that separates the chest cavity from the abdominal cavity.
Understanding the symptoms and causes of CDH is crucial for early diagnosis and treatment, which can significantly improve outcomes for affected infants.
What is Congenital Diaphragmatic Hernia (CDH)?
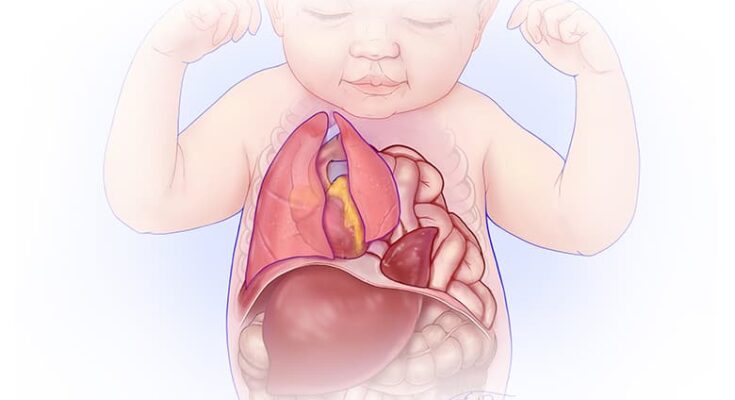
Congenital Diaphragmatic Hernia (CDH) is a serious condition that affects infants, characterized by the abnormal development of the diaphragm, the muscle that separates the chest cavity from the abdominal cavity. This rare condition occurs when a baby is born with an opening (hernia) in the diaphragm, allowing abdominal organs such as the stomach, liver, spleen, and intestines to move into the chest cavity. This displacement of organs can severely impact the infant’s lung development and function, making CDH a life-threatening condition that requires immediate medical attention after birth.
The Role of the Diaphragm in the Body
The diaphragm plays a crucial role in the respiratory system. As a large, dome-shaped muscle located at the base of the lungs and the top of the abdomen, it acts as the main muscle of respiration. During inhalation, the diaphragm contracts and flattens, creating a vacuum that draws air into the lungs. During exhalation, it relaxes and returns to its dome shape, expelling air from the lungs. Beyond its respiratory functions, the diaphragm also aids in maintaining intra-abdominal pressure, which is vital for proper digestion, and it separates the thoracic and abdominal cavities, ensuring the correct placement of organs.
How CDH Affects Infants
CDH significantly impacts infants’ health due to the herniation of abdominal organs into the chest cavity, which can lead to a host of complications. The most pressing issue is the restriction of lung development, known as pulmonary hypoplasia, where the lungs are underdeveloped and cannot provide adequate oxygenation for the body’s needs. This can lead to respiratory distress and failure immediately after birth. Furthermore, the presence of abdominal organs in the chest cavity can cause the heart and lungs to be displaced or compressed, leading to further cardiovascular and respiratory issues.
Infants with CDH often require intensive medical interventions, including surgical repair of the hernia, respiratory support, and sometimes long-term care for associated health issues. The prognosis for infants with CDH varies widely and depends on the severity of the hernia, the degree of lung underdevelopment, and the presence of other anomalies.
Understanding CDH, its implications on the health of infants, and the critical role of the diaphragm in bodily functions underscores the importance of early diagnosis and treatment. Advances in prenatal imaging and neonatal care have improved the outcomes for infants with CDH, making it a condition that, while serious, has a hopeful outlook with proper medical care.
Symptoms of Congenital Diaphragmatic Hernia (CDH)
Recognizing the symptoms of CDH is crucial for early diagnosis and treatment. Symptoms can range widely among individuals, but they are generally categorized into primary and secondary symptoms.
Primary Symptoms Associated with CDH
The primary symptoms of CDH often relate directly to respiratory distress due to the displacement of abdominal organs into the chest cavity. These symptoms can be noticeable immediately after birth and may include:
- Rapid Breathing (Tachypnea): Newborns with CDH may breathe rapidly as they struggle to take in enough air.
- Blue Skin Coloration (Cyanosis): Insufficient oxygenation can lead to a bluish tint to the skin, lips, and nail beds.
- Difficulty Breathing: There may be evident struggling to breathe, with the use of accessory muscles, flaring of the nostrils, or grunting sounds.
- Diminished Breath Sounds: Upon examination, a healthcare provider might notice decreased or absent breath sounds on the affected side due to the presence of abdominal organs in the chest.
Secondary Symptoms and Signs
Secondary symptoms of CDH may develop as a consequence of the primary symptoms or the underlying disruption of normal organ placement. These include:
- Poor Feeding: Difficulty breathing can lead to challenges with feeding, which may result in poor weight gain.
- Developmental Delays: Severe cases of CDH can impact overall development, including physical and possibly cognitive development, due to the initial critical illness and its treatments.
- Heart Murmurs: The displacement of organs can sometimes affect heart function, leading to detectable heart murmurs during physical examinations.
How Symptoms May Vary Between Individuals
The severity and combination of symptoms associated with CDH can vary significantly from one individual to another. This variation largely depends on the size of the diaphragmatic hernia and the extent to which the lungs have developed and are compressed by the displaced organs. Some newborns may exhibit mild symptoms and require less immediate intervention, while others may face life-threatening respiratory distress requiring emergency surgery.
In some cases, CDH may be diagnosed prenatally through routine ultrasound, which can reveal the herniation of abdominal organs into the chest cavity. Prenatal diagnosis allows for careful planning of delivery and immediate postnatal care. However, the exact symptoms and their severity can only be fully assessed after birth.
Understanding the symptoms of Congenital Diaphragmatic Hernia is essential for early detection and effective management of this complex condition. If you suspect your child is showing signs of CDH, immediate medical evaluation is critical to confirm the diagnosis and begin appropriate treatment.
This comprehensive overview aims to provide clarity on the symptoms associated with CDH, emphasizing the importance of early recognition and intervention. By staying informed, parents and caregivers can better advocate for their child’s health and wellbeing.
Causes and Risk Factors of Congenital Diaphragmatic Hernia (CDH)
Understanding the causes and risk factors of CDH is crucial for early diagnosis and treatment. This article explores the genetic and environmental contributions to CDH, the significance of family history, potential pregnancy complications, and recent research insights.
Genetic and Environmental Factors Contributing to CDH
Research indicates that CDH is influenced by both genetic and environmental factors, though the exact cause is often not identifiable. Genetic mutations or changes in the DNA may play a significant role, and these can be spontaneous or inherited. Environmental factors, including maternal smoking, drug use, or exposure to certain medications or chemicals during pregnancy, have also been associated with an increased risk of CDH. These findings suggest a multifactorial origin, where a combination of genetic predispositions and environmental exposures contributes to the development of CDH.
The Role of Family History in CDH
Family history is another critical aspect in the risk assessment of CDH. While most cases of CDH appear to be sporadic, meaning they occur by chance, a small percentage of cases have been observed to recur in families. This suggests a possible genetic component. Families with a history of CDH or related congenital anomalies may have a higher risk of the condition, underscoring the importance of genetic counseling and testing for at-risk individuals.
Possible Complications During Pregnancy
CDH can lead to significant complications during pregnancy, affecting both the mother and the fetus. The presence of abdominal organs in the chest cavity can severely impair fetal lung development, leading to pulmonary hypoplasia (underdeveloped lungs) and consequently, difficulties in breathing at birth. Additionally, CDH can be associated with other anomalies, including heart defects, which may complicate pregnancy management and outcomes.
Research Insights into CDH Causes
Ongoing research continues to shed light on the complex causes of CDH. Recent studies have focused on identifying specific genes and molecular pathways involved in diaphragm development, as well as how environmental factors interact with genetic predispositions to cause CDH. These insights are crucial for developing targeted therapies and improving prenatal diagnosis through advanced genetic testing and imaging techniques.
However, Congenital Diaphragmatic Hernia is a complex condition with multiple contributing factors, including genetic mutations, environmental exposures, and possibly a family history of the condition. Understanding these factors is essential for early detection, management, and treatment of CDH. Ongoing research into the causes and mechanisms of CDH holds promise for better outcomes for affected individuals and their families.
Diagnosing Congenital Diaphragmatic Hernia
Early and accurate diagnosis is paramount to managing this condition effectively. This comprehensive guide delves into the methods of diagnosing CDH, emphasizing the significance of prenatal screening, postnatal diagnosis techniques, and the importance of early detection.
Prenatal Screening and Diagnostics
Prenatal screening for CDH plays a crucial role in early detection, allowing healthcare providers to prepare for immediate intervention after birth. Several methods are employed in prenatal diagnostics:
- Ultrasound: A routine ultrasound, typically performed during the second trimester of pregnancy, can reveal the presence of CDH by showing the herniation of abdominal organs into the chest cavity.
- MRI (Magnetic Resonance Imaging): For a more detailed view, an MRI can be utilized to assess the extent of organ displacement and the size of the diaphragmatic defect.
- Fetal Echocardiogram: This specialized ultrasound examines the baby’s heart to check for any abnormalities that often accompany CDH, helping to evaluate the condition’s severity.
Postnatal Diagnosis Methods
If CDH is not detected prenatally, or to confirm prenatal findings, postnatal diagnostic methods are crucial:
- Physical Examination: Upon birth, symptoms such as respiratory distress, a barrel-shaped chest, or a concave abdomen may indicate CDH.
- Chest X-ray: This is the most common postnatal diagnostic tool, revealing displaced abdominal organs into the chest cavity.
- Computed Tomography (CT) Scan: A CT scan provides a detailed image of the diaphragm and organs, offering precise information on the hernia’s location and size.
- Blood Gas Analysis: This test measures the baby’s ability to oxygenate blood and remove carbon dioxide, indicating the lungs’ functionality affected by CDH.
The Importance of Early Detection
Early detection of CDH is critical for several reasons:
- Improved Survival Rates: Early diagnosis allows for timely surgical intervention, significantly improving survival rates.
- Better Preparation: Knowing about CDH before birth enables healthcare providers to assemble a specialized care team and prepare for potential complications.
- Informed Decision Making: Parents can make informed decisions regarding the care and treatment options for their child.
- Enhanced Management of Complications: Early detection facilitates the management of potential complications, such as respiratory distress and pulmonary hypertension, which are common in babies with CDH.
However, diagnosing Congenital Diaphragmatic Hernia as early as possible is vital for optimizing the outcome for affected infants. Prenatal screenings, coupled with postnatal diagnostic methods, play an instrumental role in identifying CDH. The importance of early detection cannot be overstated, as it directly impacts the survival rates and quality of life for the newborns facing this challenging condition.
Treatment Options for Congenital Diaphragmatic Hernia (CDH)
The treatment for CDH primarily focuses on stabilizing the infant post-birth, followed by surgical intervention to repair the diaphragmatic defect. This comprehensive guide outlines the treatment methodologies, surgical interventions, and the essential aspects of long-term care for CDH patients.
List of Treatment Methodologies
1. Initial Stabilization: Immediate treatment post-diagnosis involves stabilizing the infant to ensure adequate oxygen levels and blood circulation. This may include providing oxygen support and, in some cases, using a mechanical ventilator.
2. Nutritional Support: Proper nutrition is crucial for infants with CDH. Parenteral or enteral feeding techniques are employed depending on the infant’s condition and ability to tolerate oral feeding.
3. Pharmacological Management: Medications may be used to manage symptoms and support organ function, including treatments to help improve lung function and manage pulmonary hypertension, a common complication of CDH.
Surgical Interventions and Their Timing
Surgical Repair of CDH: The definitive treatment for CDH is surgical repair of the hernia, which involves repositioning the abdominal organs into the abdominal cavity and repairing the diaphragm.
- Timing of Surgery: The timing for the surgery is critical and is typically determined based on the infant’s stability, especially respiratory and hemodynamic stability. Surgery may be delayed until the infant is stable enough to withstand the procedure, often within the first few days to weeks of life.
Long-term Care and Considerations
1. Follow-Up Care: Infants with CDH require long-term follow-up with a multidisciplinary team including pediatric surgeons, pulmonologists, gastroenterologists, and developmental specialists to monitor growth, lung development, and any potential complications or developmental delays.
2. Respiratory Support: Some children may require ongoing respiratory support, including supplemental oxygen or mechanical ventilation, especially in cases of severe lung hypoplasia.
3. Nutritional Management: Ongoing nutritional support may be necessary to ensure proper growth and development, addressing any feeding difficulties or gastrointestinal complications.
4. Monitoring for Complications: Regular monitoring for potential long-term complications such as recurrent hernias, gastrointestinal issues, or respiratory problems is crucial for the overall well-being of the child.
The treatment of Congenital Diaphragmatic Hernia is multifaceted, involving immediate postnatal care, surgical intervention, and comprehensive long-term follow-up. Advances in medical and surgical techniques have significantly improved the outcomes for infants with CDH, emphasizing the importance of specialized care and monitoring to optimize health and development. Parents and caregivers should work closely with a dedicated healthcare team to ensure the best possible outcome for their child.
Living with Congenital Diaphragmatic Hernia (CDH): Navigating the Journey
Congenital Diaphragmatic Hernia (CDH) is a rare condition that occurs when a baby is born with an opening in the diaphragm, the muscle that helps with breathing. This opening allows abdominal organs to move into the chest, which can affect lung development and function. For families affected by CDH, understanding the challenges, considerations, support systems, and the long-term outlook is crucial for navigating this difficult journey.
Challenges and Considerations for Affected Families
Families facing a CDH diagnosis often experience a rollercoaster of emotions, from fear and confusion to hope and determination. The initial challenge is understanding the complexity of CDH and its potential impact on their child’s health. Immediate medical care is crucial, often starting with intensive neonatal support. Parents and caregivers must quickly become familiar with a range of medical terms and treatment options, including surgery to repair the diaphragm and ongoing care to support lung development and overall health.
Another significant consideration is the emotional and psychological impact on the family. Coping with the uncertainty of their child’s condition can be overwhelming. Families must navigate their own emotional well-being while providing constant care and support to their child. This journey can strain personal relationships, finances, and daily life, highlighting the importance of a strong support system.
Support Systems and Resources
Building a robust support network is essential for families affected by CDH. This network can include healthcare professionals, such as pediatric surgeons, neonatologists, respiratory therapists, and nurses, who specialize in CDH care. Equally important are the emotional and psychological support resources, including counselors, support groups, and organizations dedicated to CDH. These resources offer families a platform to share experiences, seek advice, and find comfort in a community that understands their challenges.
Online resources also play a crucial role in providing information and connecting families with support services. Websites, forums, and social media groups dedicated to CDH can offer valuable insights, advice, and encouragement from other families navigating similar paths.
Long-term Outlook for Infants with CDH
The long-term outlook for infants with CDH has improved significantly with advances in medical care and surgical techniques. Early diagnosis and treatment are key factors that influence outcomes. While the severity of CDH varies, many children go on to lead healthy, active lives. However, some may face ongoing health challenges, such as respiratory issues, growth delays, or the need for additional surgeries.
Regular follow-up with healthcare providers is essential to monitor the child’s health and development, address any complications, and provide support for any developmental delays or challenges. A proactive and informed approach to care can help maximize the child’s quality of life and potential.
Living with Congenital Diaphragmatic Hernia is a challenging journey that requires strength, resilience, and a comprehensive support system. By understanding the challenges and considerations, leveraging support resources, and focusing on the long-term outlook, families can navigate the path of CDH with hope and determination. As medical care continues to advance, the future for children with CDH is brighter than ever, offering them the possibility of a fulfilling life.
Prevention and Research: Towards a Better Understanding of Congenital Diaphragmatic Hernia (CDH)
Let’s delves into the current state of CDH prevention and the groundbreaking advances in genetic screening and prenatal care that promise to mitigate its incidence and impact.
Current Research on CDH Prevention
Research into the prevention of Congenital Diaphragmatic Hernia has increasingly focused on identifying the risk factors and genetic mutations associated with its development. Scientists and medical professionals are dedicated to discovering biomarkers and genetic indicators that can predict CDH, enabling early intervention strategies. Through extensive cohort studies and the analysis of familial health histories, researchers are piecing together the puzzle of CDH’s etiology, aiming to develop targeted prevention measures that can be implemented even before birth.
The multifaceted nature of CDH, influenced by genetic, environmental, and possibly maternal health factors, necessitates a broad research approach. Current studies explore the interplay between these elements, seeking to understand how they contribute to the malformation of the diaphragm. By identifying the conditions that predispose infants to CDH, researchers are laying the groundwork for preventive guidelines that could significantly reduce the prevalence of this challenging condition.
Advances in Genetic Screening and Prenatal Care
One of the most promising areas of CDH research is in the advancements of genetic screening and prenatal care. Genetic testing has become an invaluable tool in the early detection of CDH, offering expectant parents critical insights into their baby’s health. Through cutting-edge techniques such as whole-exome sequencing and non-invasive prenatal testing (NIPT), healthcare providers can identify genetic abnormalities associated with CDH more accurately and earlier in the pregnancy than ever before.
These genetic screenings are complemented by innovations in prenatal care, including advanced ultrasound imaging and fetal MRI. These technologies not only improve the detection rates of CDH but also allow for the detailed monitoring of the fetus’s condition throughout the pregnancy. Such advancements enable multidisciplinary teams of specialists to formulate comprehensive care plans, preparing for immediate intervention after birth if necessary.
Moreover, the integration of telemedicine into prenatal care has made these advanced screening and monitoring services more accessible to expectant mothers, especially those in remote or underserved areas. This ensures that a broader demographic has access to the specialized care required for managing pregnancies complicated by CDH.
The ongoing research into the prevention of Congenital Diaphragmatic Hernia and the rapid advancements in genetic screening and prenatal care are vital in the fight against this condition. With each discovery and technological breakthrough, the medical community moves closer to reducing the incidence and severity of CDH, offering hope to countless families. As we continue to push the boundaries of what’s possible in prenatal medicine, the goal remains clear: a future where CDH can be effectively prevented or managed, ensuring healthier outcomes for the next generation.
FAQs on Congenital Diaphragmatic Hernia (CDH)
What is Congenital Diaphragmatic Hernia (CDH)?
Congenital Diaphragmatic Hernia (CDH) is a birth defect where there is an abnormal opening in the diaphragm, the muscle that helps in breathing and separates the chest cavity from the abdominal cavity. This opening allows organs from the abdomen to move into the chest cavity, affecting lung development and function.
What causes CDH?
The exact cause of CDH is not known. It is believed to occur during fetal development when the diaphragm fails to form completely. This condition can be associated with genetic factors, environmental exposure, or a combination of both, but in many cases, the cause remains unidentified.
What are the symptoms of CDH?
Symptoms of CDH can vary depending on the severity of the hernia and the organs involved. Common symptoms include difficulty breathing, a rapid heartbeat, a blue tinge to the skin (cyanosis), a concave abdomen, and a chest that appears swollen on one side. Severe cases may lead to life-threatening respiratory distress immediately after birth.
How is CDH diagnosed?
CDH is often diagnosed before birth through prenatal ultrasound, which can show the herniation of abdominal organs into the chest cavity. After birth, diagnosis may be confirmed with additional imaging tests such as X-rays, MRI, or CT scans to assess the extent of the hernia and the displacement of organs.
What treatment options are available for CDH?
Treatment for CDH typically involves surgical repair of the hernia, which may be performed after stabilizing the infant’s condition post-birth. This surgery involves repositioning the herniated organs into the abdominal cavity and repairing the opening in the diaphragm. In severe cases, additional treatments may be required to support lung development and function, including ventilation support and, in some cases, a treatment called ECMO (Extracorporeal Membrane Oxygenation) if the baby’s lungs are severely underdeveloped.
Can CDH be prevented?
Currently, there is no known way to prevent CDH. However, expecting mothers can reduce the risk of congenital defects by maintaining a healthy pregnancy. This includes regular prenatal care, avoiding harmful substances like tobacco and alcohol, and managing chronic health conditions under a healthcare provider’s guidance.
What is the prognosis for a baby with CDH?
The prognosis for a baby with CDH varies widely and depends on the size of the hernia, the degree of lung underdevelopment, and the presence of other congenital conditions. Advances in medical and surgical treatments have significantly improved outcomes, with many children leading healthy lives after treatment. However, some children may experience long-term health issues related to their condition.
Is there any support available for families affected by CDH?
Yes, there are several support groups and organizations dedicated to helping families affected by CDH. These groups offer resources for emotional support, information on treatment options, and opportunities to connect with other families facing similar challenges. It’s important for affected families to reach out for support and information to navigate the challenges of CDH together.
Conclusion
In summing up our discussion on Congenital Diaphragmatic Hernia (CDH), recognizing the symptoms and understanding the causes of this condition are pivotal steps toward ensuring the health and well-being of newborns. CDH, a condition characterized by the abnormal development of the diaphragm, allows abdominal organs to move into the chest cavity, thereby affecting lung development. This highlights the critical nature of early detection and intervention.
Expecting parents are strongly encouraged to prioritize and seek comprehensive prenatal care. Regular prenatal visits not only provide a platform for the early detection of CDH through ultrasound screenings but also offer an opportunity for healthcare providers to educate parents about potential risk factors and preventive measures. Prenatal care plays a crucial role in preparing for conditions like CDH, enabling timely and effective treatment plans that can significantly improve outcomes for affected infants.
As we navigate the complexities of congenital conditions such as CDH, let us remember the power of knowledge, early intervention, and the unwavering support of healthcare professionals. Expecting parents, armed with the right information and guided by specialized care, can face these challenges with confidence, ensuring a healthier start for their children.