Colon Polyps Symptoms: Colon polyps are growths on the inner lining of the colon or large intestine, part of your digestive system. While most polyps are benign, some can develop into cancer over time.
Understanding the symptoms and causes of colon polyps is crucial for early detection and prevention of colon cancer.
This comprehensive guide will delve into the key aspects of colon polyps, including their types, potential symptoms, causes, and the importance of screening and prevention.
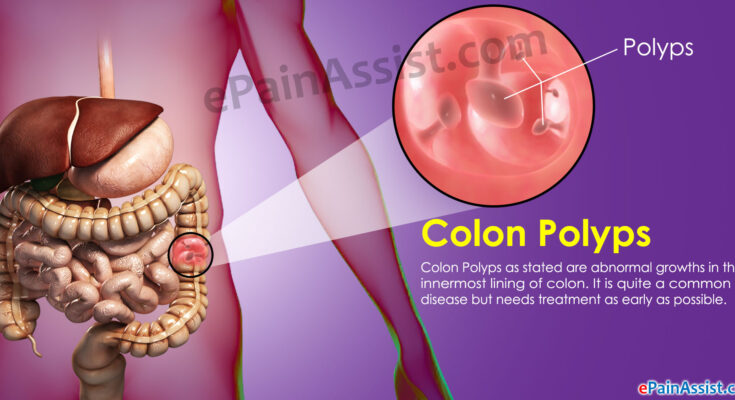
What Are Colon Polyps?
Colon polyps are growths that appear on the inner lining of the large intestine (colon) or rectum. While many colon polyps are benign (noncancerous), some can develop into colon cancer over time, making early detection and removal crucial for preventing cancer. Understanding what colon polyps are, the types you might encounter, and their prevalence across different demographics can help you stay informed about your colon health.
Types of Colon Polyps
There are several types of colon polyps, each with unique characteristics and implications for your health:
- Adenomatous Polyps (Adenomas): These are the most common type of colon polyps and are considered precancerous. Although not all adenomas become cancerous, the majority of colon cancers originate from adenomatous polyps.
- Hyperplastic Polyps and Inflammatory Polyps: Generally smaller and not considered precancerous, these polyps are less likely to develop into colon cancer. They are often found in the rectum and lower colon.
- Serrated Polyps: This category includes several types of polyps, such as hyperplastic polyps and sessile serrated adenomas. While hyperplastic polyps are usually benign, sessile serrated adenomas can be precancerous, especially when they are larger in size.
Understanding the types of colon polyps is crucial for assessing cancer risk and determining the appropriate treatment and surveillance strategies.
Prevalence and Demographic Considerations
Colon polyps are a common health concern, with their prevalence increasing with age. Most individuals who develop colon polyps are over the age of 50, which is why screening recommendations often start at this age. However, colon polyps can occur in younger individuals, especially those with a family history of colon polyps or colon cancer.
Demographic factors, including race and ethnicity, can also influence the risk of developing colon polyps. Studies have shown that African Americans may have a higher risk of developing polyps and colon cancer at a younger age compared to other racial groups. Lifestyle factors, such as diet, smoking, and physical inactivity, are also linked to an increased risk of polyps, highlighting the importance of a healthy lifestyle in prevention.
However, colon polyps are a significant health issue that can lead to colon cancer if not detected and treated early. Understanding the types of colon polyps and being aware of the prevalence and risk factors associated with different demographics can empower individuals to take proactive steps in managing their colon health. Regular screening, especially for those over 50 or with risk factors, is key to early detection and prevention of colon cancer.
Symptoms of Colon Polyps
Colon polyps are growths that appear on the inner lining of the colon or large intestine. While often benign, some polyps can develop into cancer, making it crucial to be aware of their symptoms and when to seek medical advice. However, it’s important to note that many colon polyps do not cause symptoms, which is why regular screening is recommended, especially for those over the age of 50 or with risk factors for colorectal cancer.
Common Symptoms Associated with Colon Polyps
In cases where symptoms are present, they may include the following:
- Rectal Bleeding: This is one of the most noticeable signs. Blood can appear as red streaks in the stool or make the stool appear darker. It’s crucial not to ignore rectal bleeding, as it can also be a sign of other conditions such as hemorrhoids or colorectal cancer.
- Change in Stool Color: Polyps can cause the stool to become black, indicating the presence of blood. It’s important to monitor any significant changes in stool color.
- Change in Bowel Habits: This includes new constipation or diarrhea that lasts for more than a week. Changes in bowel habits can signal alterations in the colon caused by polyps.
- Abdominal Pain: While less common, some individuals may experience discomfort or pain in the lower abdomen, especially if a polyp is large or if there are multiple polyps.
- Iron-deficiency Anemia: Unexplained anemia might be a sign of hidden bleeding in the colon, possibly due to polyps.
Why Many Colon Polyps Don’t Cause Symptoms
The reason many colon polyps go unnoticed without causing symptoms is largely due to their size and location. Smaller polyps are less likely to disturb the normal function of the colon and thus remain asymptomatic. It’s only when they grow larger that they may lead to noticeable symptoms, such as bleeding or changes in bowel habits.
When to See a Doctor: Symptoms That Require Medical Attention
It’s imperative to consult a healthcare provider if you experience any of the symptoms mentioned, even if they seem minor or inconsistent. Early detection and removal of polyps can prevent colorectal cancer. Specifically, seek medical advice if you have:
- Persistent rectal bleeding
- Unexplained changes in your bowel habits lasting more than a week
- Continuous discomfort or abdominal pain
- A family history of colon polyps or colorectal cancer
Regular screenings, such as colonoscopies, are recommended starting at age 45 or earlier for individuals with a family history of colorectal cancer or polyps. These screenings are crucial for detecting polyps early, often before symptoms develop.
Understanding the potential signs of colon polyps and the importance of regular screenings can significantly impact early detection and prevention of colorectal cancer. If you’re experiencing any of the symptoms listed or fall into a high-risk category, don’t hesitate to discuss screening options with your healthcare provider.
Causes and Risk Factors of Colon Polyps
While many polyps are benign (noncancerous), some can evolve into colon cancer over time, making it crucial to understand the causes and risk factors associated with their development.
Genetic Factors Contributing to Colon Polyps
Genetics play a significant role in the development of colon polyps. Certain inherited genetic conditions can increase the risk significantly:
- Familial Adenomatous Polyposis (FAP): A rare disorder that causes hundreds to thousands of polyps in the lining of the colon and rectum during the teenage years. If untreated, it significantly increases the risk of developing colon cancer by age 40.
- Lynch Syndrome (Hereditary Non-Polyposis Colorectal Cancer or HNPCC): Another genetic condition that predisposes individuals to colon cancer and other cancers, often leading to the development of fewer polyps at a younger age.
- MUTYH-associated polyposis (MAP): A condition similar to FAP but caused by mutations in the MUTYH gene, leading to multiple adenomatous polyps and a high risk of colon cancer.
Understanding these genetic factors is crucial for early detection and prevention, especially in individuals with a family history of these conditions.
Lifestyle and Dietary Factors
Lifestyle and dietary choices significantly influence the development of colon polyps:
- High-fat, low-fiber diet: Diets high in red meat and fat but low in fiber, fruits, and vegetables are linked to an increased risk of colon polyps.
- Obesity: Being significantly overweight increases the risk of developing and dying from colon cancer.
- Smoking: Long-term smoking has been associated with an increased risk of developing colon polyps and colon cancer.
- Alcohol consumption: Excessive alcohol intake is linked to a higher risk of polyps and colon cancer.
Adopting a healthy lifestyle that includes regular exercise, a diet rich in fruits, vegetables, and whole grains, and limiting alcohol and tobacco use can help reduce the risk of colon polyps.
Age, Family History, and Other Risk Factors
Apart from genetic predispositions and lifestyle choices, several other factors contribute to the risk of developing colon polyps:
- Age: The risk of developing colon polyps increases with age, particularly after the age of 50.
- Family history: Having a family history of colon polyps or colon cancer increases one’s risk. This risk is higher if a first-degree relative (parent, sibling, or child) was diagnosed with colon cancer or polyps at a young age.
- Personal history of polyps or colon cancer: Individuals who have previously had colon polyps or cancer are at higher risk of developing new polyps.
- Inflammatory intestinal conditions: Conditions like ulcerative colitis and Crohn’s disease can increase the risk of developing colon cancer and polyps.
However, regular screenings, such as colonoscopies, are recommended for individuals at higher risk, starting at an age determined by their healthcare provider. Lifestyle modifications can also play a significant role in reducing the risk of polyps and the subsequent risk of colon cancer.
Complications Associated with Colon Polyps
Here, we delve into the primary complications associated with colon polyps, including their potential to develop into cancer and other related health issues such as bleeding and intestinal blockage.
Risk of Colon Polyps Turning into Cancer
One of the most significant concerns with colon polyps is their potential to transform into colorectal cancer over time. Although not all polyps become cancerous, certain types, particularly adenomatous polyps (adenomas), have a higher risk of evolving into cancer. The likelihood of a polyp turning into cancer depends on several factors, including its size, number, and histological type. Polyps larger than 1 cm in diameter, those that are numerous, and those with villous features or high-grade dysplasia are considered at greater risk. Regular screenings and polyp removal during colonoscopies can significantly reduce the risk of colon cancer, highlighting the importance of early detection and intervention.
Other Potential Complications
In addition to the risk of cancer, colon polyps can lead to other complications, albeit less commonly. These include:
- Bleeding: Polyps can cause rectal bleeding, which might be noticeable in the stool. While bleeding can also result from other conditions, it’s essential to consult a healthcare provider for proper diagnosis and treatment if noticed.
- Intestinal Blockage: Large polyps can grow to obstruct parts of the colon, leading to symptoms of intestinal obstruction, such as abdominal pain, constipation, and bloating. This complication is relatively rare but requires immediate medical attention when it occurs.
It’s essential for individuals to undergo regular screening for colon polyps, especially if they are over the age of 50 or have risk factors such as a family history of colon cancer, a personal history of polyps, or conditions like inflammatory bowel disease. Early detection and management of polyps can prevent these complications and contribute to a healthier, longer life.
By staying informed about the potential complications of colon polyps and engaging in preventative measures, individuals can significantly reduce their risk of serious health issues. Remember, regular screenings are a key component of preventive healthcare and can lead to early detection and treatment of polyps before they develop into more severe conditions.
However, while colon polyps are common and often harmless, being vigilant about screening and treatment can prevent the development of cancer and other complications. If you’re due for a screening or have concerns about colon polyps, consult your healthcare provider to discuss the most appropriate steps for your health and well-being.
Diagnosis of Colon Polyps
While many colon polyps are benign, some can develop into cancer, making early detection and diagnosis crucial for preventing colorectal cancer. This article outlines the methods used for diagnosing colon polyps and emphasizes the importance of regular screening and early detection.
Diagnosis Methods for Colon Polyps
Diagnosing colon polyps typically involves several steps and procedures, each aimed at identifying polyps and assessing their potential to develop into cancer. Here are the most common diagnostic methods:
- Colonoscopy: This is the most effective and widely used method for detecting colon polyps. During a colonoscopy, a long, flexible tube equipped with a video camera (colonoscope) is inserted into the rectum to examine the entire colon. If polyps are found, they can often be removed during the procedure.
- Flexible Sigmoidoscopy: Similar to a colonoscopy, this procedure examines the rectum and the lower part of the colon. A flexible sigmoidoscopy can detect polyps and cancers in these areas but does not allow viewing of the entire colon.
- CT Colonography (Virtual Colonoscopy): This imaging method uses CT scans to produce detailed pictures of the colon and rectum. It can detect polyps and other abnormalities without inserting a tube into the colon. However, if polyps are found, a traditional colonoscopy may still be necessary to remove them.
- Stool Tests: Certain tests can detect changes in DNA or the presence of blood in the stool, which may indicate the presence of polyps or colorectal cancer. Stool tests need to be done more frequently and are less invasive but may require follow-up with a colonoscopy if abnormal results are found.
Importance of Regular Screening and Early Detection
Regular screening is vital for the early detection and removal of colon polyps before they can develop into cancer. The American Cancer Society recommends that adults at average risk of colorectal cancer start regular screening at age 45. People with a family history of colorectal cancer or polyps and those with other risk factors may need to start screening earlier and undergo screenings more frequently.
Early detection of colon polyps can significantly reduce the risk of developing colorectal cancer. Since polyps can take years to develop into cancer, regular screening provides a critical window for early intervention. Removing polyps during a colonoscopy can prevent them from becoming malignant, offering an effective prevention strategy against colorectal cancer.
However, understanding the methods for diagnosing colon polyps and the importance of regular screening and early detection can save lives. By undergoing recommended screenings, individuals can significantly lower their risk of developing colorectal cancer, highlighting the crucial role of preventive healthcare measures in combating this disease.
Treatment and Management of Colon Polyps
With appropriate treatment and management, the risk can be significantly reduced. This guide outlines the various treatment options available for colon polyps and provides advice on lifestyle changes and prevention strategies to maintain a healthy colon.
Treatment Options for Colon Polyps
The treatment for colon polyps largely depends on their size, number, and histology (cell structure). Here are the primary treatment methods:
- Polypectomy: The most common treatment, a polypectomy involves the removal of polyps during a colonoscopy. This procedure is minimally invasive and can prevent the progression of polyps into cancer.
- Endoscopic Mucosal Resection (EMR): For larger polyps, EMR is preferred. This technique involves injecting a solution under the polyp to lift it and then removing it with a snare.
- Surgery: In cases where polyps are too large or too numerous to be removed endoscopically, or if they contain cancer cells, surgery may be necessary. This can involve removing part of the colon.
- Follow-up Surveillance: After removal, regular follow-up colonoscopies are crucial to check for new polyps. The frequency of these exams depends on the initial number and type of polyps found.
Lifestyle Changes and Prevention Strategies
In addition to medical treatments, making certain lifestyle changes can help prevent the formation of new polyps or reduce the risk of colon cancer:
- Diet: Adopt a diet high in fruits, vegetables, and whole grains while reducing red meat and processed foods. Fiber is particularly important as it helps to keep the colon healthy.
- Exercise: Regular physical activity can significantly lower the risk of developing colon polyps and colon cancer.
- Weight Management: Maintaining a healthy weight is crucial for reducing the risk of many types of cancer, including colon cancer.
- Limit Alcohol and Quit Smoking: Reducing alcohol intake and quitting smoking can decrease the risk of colon polyps and improve overall health.
- Calcium and Vitamin D: Some studies suggest that increasing intake of calcium and vitamin D may help prevent the formation of polyps, although the evidence is not definitive.
- Aspirin: In some cases, doctors may recommend aspirin to reduce the risk of polyps, especially for those with a history of polyps or colon cancer. However, aspirin therapy comes with its own risks and should only be started under the advice of a healthcare provider.
By combining these treatment options with healthy lifestyle choices, individuals can effectively manage and reduce the risk of colon polyps, contributing to long-term colon health. Always consult with a healthcare professional to determine the most appropriate treatment and prevention strategy for your specific situation.
Prevention: Reducing Your Risk of Developing Colon Polyps
There are proactive steps you can take to significantly reduce your risk of developing colon polyps. By focusing on diet and lifestyle modifications and adhering to regular screenings and medical advice, you can protect your colon health.
Diet and Lifestyle Modifications
- Eat More Fruits and Vegetables: A diet rich in fruits, vegetables, and whole grains provides essential nutrients and antioxidants that can help prevent colon polyps. These foods are high in fiber, which helps keep your digestive system running smoothly and reduces the risk of polyps forming.
- Limit Red and Processed Meats: Studies have shown that consuming large amounts of red meat (such as beef, pork, and lamb) and processed meats (such as hot dogs and some luncheon meats) can increase your risk of developing colon polyps. Opt for lean protein sources like chicken, fish, and plant-based proteins instead.
- Maintain a Healthy Weight: Being overweight or obese increases your risk of developing colon polyps. Engaging in regular physical activity and managing your weight through a healthy diet can significantly reduce your risk.
- Quit Smoking and Limit Alcohol Consumption: Both smoking and excessive alcohol consumption are linked to an increased risk of colon polyps. Quitting smoking and limiting alcohol intake can improve your overall health and reduce your risk.
Regular Screenings and Medical Advice
- Follow Screening Guidelines: Regular colon cancer screenings are the most powerful weapon in preventing colon polyps and detecting them early when they are most treatable. Most people should start screening for colon cancer at age 45, but if you have a family history of the disease, talk to your doctor about starting earlier.
- Listen to Your Body: Be attentive to changes in your bowel habits, such as persistent constipation or diarrhea, and report any symptoms like blood in your stool or abdominal pain to your doctor promptly.
- Discuss Your Risk Factors with Your Doctor: Your family history, age, and lifestyle can affect your risk of developing colon polyps. Discuss these factors with your healthcare provider to develop a personalized prevention plan.
- Consider Genetic Counseling: If you have a family history of colon polyps or colon cancer, genetic counseling can help assess your risk and guide you in taking preventative measures.
By making informed diet and lifestyle choices and adhering to recommended screening schedules, you can significantly reduce your risk of developing colon polyps. Remember, early detection and prevention are key to maintaining your colon health and overall well-being.
FAQs About Colon Polyps
What are colon polyps?
Colon polyps are clumps of cells that form on the lining of the colon. They can be flat or raised and vary in size. While most polyps are harmless, some can become cancerous over time.
What causes colon polyps?
The exact cause of colon polyps is not fully understood, but they are believed to develop when there are abnormal cell growths in the colon’s lining. Factors that may increase the risk include age (over 50), a family history of colon polyps or colon cancer, a high-fat, low-fiber diet, obesity, smoking, and certain genetic disorders.
What are the symptoms of colon polyps?
Many colon polyps do not cause symptoms and are often discovered during routine screenings. When symptoms do occur, they may include rectal bleeding, blood in the stool, abdominal pain, or a change in bowel habits. However, these symptoms can also be caused by other conditions, so it’s important to consult a healthcare provider for an accurate diagnosis.
How are colon polyps diagnosed?
Colon polyps are most commonly diagnosed through colonoscopy, a procedure that allows a doctor to examine the inside of the colon with a camera on a flexible tube. Other diagnostic methods include sigmoidoscopy, CT colonography, and stool tests.
Can colon polyps be prevented?
While there’s no guaranteed way to prevent colon polyps, you can reduce your risk by adopting a healthy lifestyle. This includes eating a diet rich in fruits, vegetables, and whole grains, maintaining a healthy weight, quitting smoking, limiting alcohol consumption, and exercising regularly.
How are colon polyps treated?
Treatment for colon polyps usually involves removing them during a colonoscopy. This is a preventive measure to reduce the risk of colon cancer. For larger or more numerous polyps, additional surgery may be required.
Are there any complications associated with colon polyps?
If left untreated, some types of colon polyps can turn into colon cancer, which can be life-threatening. This is why regular screening and early removal of polyps are crucial.
How often should I be screened for colon polyps?
Screening recommendations depend on your risk factors. For most adults, screening for colon cancer and polyps should start at age 45 to 50. People with a higher risk, such as those with a family history of colon cancer or polyps, may need to start screening earlier and be screened more frequently.
Can diet affect colon polyps?
Yes, diet plays a role in the development of colon polyps. Diets high in red meats and processed foods can increase the risk, while diets high in fiber from fruits, vegetables, and whole grains can reduce the risk.
Conclusion:
Managing and preventing colon polyps is intrinsically linked to adopting a healthy lifestyle. Diets rich in fruits, vegetables, and whole grains, coupled with regular physical activity, contribute significantly to lowering the risk of polyps. Additionally, moderating the consumption of alcohol and avoiding smoking can further reduce risks. It’s also essential to follow through with the medical advice and screening schedules recommended by healthcare providers to stay ahead in prevention.
In conclusion, the journey to understanding, managing, and preventing colon polyps is a testament to the power of awareness, early detection, and proactive health management. By recognizing symptoms, understanding causes, and adhering to recommended screening schedules, we can collectively mitigate the risks associated with colon polyps. Let’s commit to a lifestyle that prioritizes health and wellness, ensuring a proactive stance against colon polyps and their potential complications. Together, we can pave the way for a healthier future, underscored by vigilance, education, and proactive health practices.