Coarctation of the Aorta Symptoms: Coarctation of the aorta is a congenital condition that can significantly impact an individual’s cardiovascular health.
This condition, characterized by the narrowing of the aorta, the main artery carrying blood from the heart to the rest of the body, can lead to various symptoms and complications if not diagnosed and treated promptly.
Our comprehensive guide delves into the symptoms, causes, and understanding of this condition, aiming to provide invaluable information for affected individuals and their families.
What is Coarctation of the Aorta?
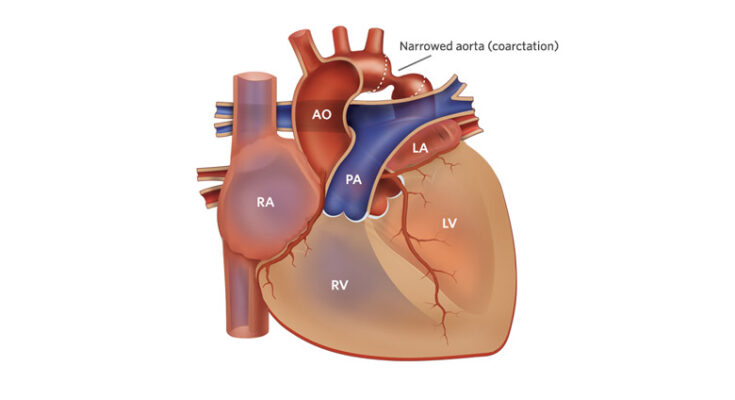
Coarctation of the aorta is a congenital condition, meaning it’s present at birth, where a section of the aorta, the major artery carrying blood from the heart to the body, is narrowed. This narrowing can increase blood pressure above the constriction and reduce blood flow to the parts of the body below the constriction. Understanding the role of the aorta in the cardiovascular system is crucial to comprehending how coarctation affects heart function and overall health.
The Role of the Aorta in the Cardiovascular System
The aorta is the largest artery in the body and plays a pivotal role in the cardiovascular system. It originates from the left ventricle of the heart, arcs over the heart, descending into the chest and abdomen. The aorta distributes oxygen-rich blood from the heart to the rest of the body through its various branches. Given its vital function, any condition affecting the aorta can significantly impact the body’s ability to circulate blood effectively.
How Coarctation Affects Heart Function and Overall Health
Coarctation of the aorta forces the heart to work harder than normal to pump blood through the narrowed section of the aorta. Over time, this extra effort can lead to thickening of the heart muscle (left ventricular hypertrophy), which can affect the heart’s ability to pump blood efficiently and increase the risk of heart failure.
The increased pressure in the arteries leading from the heart can also lead to other health problems, such as high blood pressure (hypertension), which is a risk factor for stroke, heart attack, and other cardiovascular diseases. Additionally, the reduced blood flow to the lower part of the body can cause fatigue, weakness, and in severe cases, damage to organs due to insufficient blood supply.
Furthermore, coarctation of the aorta can be associated with other congenital heart defects, which may compound the impact on an individual’s health. Early diagnosis and treatment are crucial to prevent long-term complications and improve the quality of life for those affected by this condition.
However, coarctation of the aorta is a serious congenital condition that affects the heart’s function and overall health by causing increased pressure in the heart and reduced blood flow to the body. Understanding the role of the aorta and the implications of its narrowing highlights the importance of early intervention and management to mitigate health risks associated with this condition.
Symptoms of Coarctation of the Aorta
Understanding these signs is pivotal for early diagnosis and effective management. This guide outlines the early signs, advanced symptoms, and the differences in symptoms across age groups—infants, children, and adults—providing an accessible and comprehensive overview for caregivers and patients alike.
Early Signs
In many cases, Coarctation of the Aorta may not manifest noticeable symptoms immediately, particularly in mild cases or shortly after birth. However, early signs can include:
- Difficulty Feeding: Infants may show signs of fatigue or become easily exhausted during feedings.
- Failure to Thrive: A noticeable lag in weight gain or growth compared to age-appropriate milestones.
- Shortness of Breath: Infants and young children may exhibit labored breathing, even during rest or mild activities.
- Lethargy: An unusual level of tiredness or lack of energy could be an early indicator.
Advanced Symptoms
As the condition progresses without diagnosis or treatment, more severe symptoms can emerge, including:
- High Blood Pressure: Elevated blood pressure is common and can be significantly higher in the upper body compared to the lower body.
- Headaches: Frequent or persistent headaches can occur due to hypertension.
- Leg Cramps or Weakness: Reduced blood flow to the lower body can cause pain, cramps, or weakness in the legs, especially after physical activity.
- Nosebleeds: Increased frequency of nosebleeds may be related to high blood pressure.
- Chest Pain: Occurs especially during exercise due to reduced blood flow to the heart.
Differences in Symptoms by Age Group
The manifestation of Coarctation of the Aorta symptoms can differ markedly across age groups:
- Infants: The most vulnerable age group, infants may present with severe symptoms early on, such as significant difficulty feeding, failure to gain weight, and a pale or grayish skin tone indicating poor blood circulation.
- Children: Symptoms in children might be more subtle or develop over time. They may complain of leg pain during physical activities, exhibit high blood pressure during routine check-ups, or show signs of stunted growth.
- Adults: Adult diagnosis is less common but possible, often during routine medical examinations revealing hypertension. Symptoms in adults can include high blood pressure, headaches, leg cramps, and chest pain during physical exertion.
Meanwhile, early detection and intervention can significantly improve outcomes, highlighting the importance of regular pediatric check-ups and monitoring for any signs of heart defects. If you or your child exhibit any of these symptoms, consulting with a healthcare provider for a comprehensive evaluation is essential.
Potential Causes and Risk Factors of Coarctation of the Aorta
Understanding the potential causes and risk factors associated with this condition is crucial for early detection and management. This section delves into genetic factors, environmental influences, and associated conditions that contribute to the development of CoA.
Genetic Factors
Research indicates a strong genetic component in the occurrence of coarctation of the aorta. Individuals with certain genetic disorders, such as Turner syndrome, Williams syndrome, and certain types of chromosomal abnormalities, are at a higher risk of developing CoA. These conditions can affect the overall development of the cardiovascular system, leading to structural defects including the narrowing of the aorta. A family history of congenital heart defects also increases the likelihood of CoA, suggesting a hereditary pattern in some cases.
Environmental Influences
Although genetic factors play a significant role, environmental influences during pregnancy can also contribute to the risk of a child developing coarctation of the aorta. Factors such as maternal alcohol consumption, smoking, and the use of certain medications during pregnancy have been associated with a higher incidence of congenital heart defects, including CoA. Additionally, poor maternal nutrition and exposure to environmental toxins can potentially affect fetal development, leading to structural abnormalities in the heart.
Associated Conditions
Coarctation of the aorta often occurs in conjunction with other congenital heart defects, such as bicuspid aortic valve, ventricular septal defects, and patent ductus arteriosus. The presence of these associated conditions can complicate the diagnosis and management of CoA. Furthermore, individuals with CoA are at an increased risk for developing hypertension, even after the aortic narrowing has been corrected. It is crucial for healthcare providers to monitor for these associated conditions and manage them alongside CoA to optimize patient outcomes.
Meanwhile, the multifactorial causes and risk factors of coarctation of the aorta is essential for early detection, intervention, and management of this congenital heart defect. Genetic predispositions, environmental factors during pregnancy, and the presence of associated conditions all contribute to the complexity of CoA, highlighting the importance of comprehensive care and monitoring for affected individuals.
Diagnosis and Importance of Early Detection of Coarctation of the Aorta
Early detection and diagnosis are vital for managing this condition effectively. This section delves into the various methods used for diagnosing coarctation of the aorta and underscores the importance of recognizing symptoms early for a timely diagnosis.
Diagnostic Methods for Coarctation of the Aorta
Several diagnostic tools and methods play a crucial role in identifying coarctation of the aorta, each with its own advantages in providing detailed insights into the heart’s structure and function:
- Echocardiogram: This is the primary diagnostic tool for coarctation of the aorta. It uses sound waves to create images of the heart, allowing doctors to see the condition of the heart and the aorta.
- Chest X-ray: Although not definitive for coarctation, a chest X-ray can show signs of heart enlargement or changes in the shape of the aorta.
- Magnetic Resonance Imaging (MRI): An MRI provides detailed images of the heart and aorta, offering precise information about the location and severity of the narrowing.
- Computed Tomography (CT) Scan: Similar to an MRI, a CT scan provides detailed images of the aorta and can help in planning surgical interventions if necessary.
- Cardiac Catheterization: This invasive procedure involves threading a catheter through the blood vessels to the heart to measure the pressure and look at the aorta more closely.
- Blood Pressure Measurements: Discrepancies in blood pressure readings between the arms and legs can be an indicator of coarctation of the aorta.
Importance of Early Detection
Early detection of coarctation of the aorta is crucial for several reasons. Recognizing symptoms early can lead to a timely diagnosis, which is essential for preventing complications such as hypertension, heart failure, aortic rupture, and other potentially life-threatening conditions. Symptoms may include difficulty breathing, heavy sweating, poor weight gain in infants, high blood pressure, and cold legs or feet due to reduced blood flow.
Early diagnosis allows for prompt treatment, which may involve surgical repair or balloon angioplasty, depending on the severity and location of the narrowing. Early intervention can significantly improve the quality of life and prognosis for individuals with coarctation of the aorta.
It’s important for parents, caregivers, and healthcare providers to be aware of the signs and symptoms associated with this condition and to seek medical advice if coarctation of the aorta is suspected. Through awareness, early diagnosis, and timely intervention, individuals with coarctation of the aorta can lead healthier and more active lives.
Recognizing the signs and seeking prompt medical evaluation are essential steps in ensuring the best possible outcomes for those affected by this condition.
Complications of Untreated Coarctation of the Aorta
Coarctation of the aorta is a serious congenital heart defect characterized by a narrowing of the aorta, the major artery carrying blood from the heart to the body. If left untreated, this condition can lead to severe complications that significantly impact an individual’s health and quality of life. Understanding these risks is crucial for early diagnosis and treatment.
High Blood Pressure
One of the primary complications arising from untreated coarctation of the aorta is high blood pressure (hypertension). This condition occurs because the heart must work harder to pump blood through the narrowed section of the aorta, leading to increased pressure in the arteries. Over time, untreated high blood pressure can cause a range of health issues, including but not limited to, damage to the blood vessels, kidneys, and other vital organs. The risks associated with untreated hypertension can be severe, leading to life-threatening conditions such as stroke, heart attack, and kidney failure.
Heart Damage
The strain placed on the heart by coarctation of the aorta can also lead to long-term damage. The heart’s increased workload can cause the left ventricle to thicken and stiffen, a condition known as left ventricular hypertrophy. This change in the heart’s structure can impair its ability to pump blood efficiently, leading to heart failure over time. Additionally, the stress on the heart can increase the risk of developing endocarditis, an infection of the heart’s inner lining, which can further complicate the condition and lead to significant health issues.
Other Health Risks
Beyond high blood pressure and heart damage, untreated coarctation of the aorta can affect other organs and systems in the body. The brain, for instance, can be adversely affected due to the potential for reduced blood flow or the increased risk of stroke. The kidneys may also suffer damage over time due to the high blood pressure, leading to chronic kidney disease or failure. Furthermore, the skeletal system can be affected, as hypertension can impact bone density and health.
However, coarctation of the aorta, if left untreated, poses significant health risks that extend far beyond the heart and blood vessels. These complications highlight the importance of early detection, monitoring, and treatment to mitigate the adverse effects on the body. Individuals diagnosed with coarctation of the aorta should work closely with their healthcare provider to develop an effective treatment plan that addresses their specific needs and reduces the risk of these severe complications.
Management and Treatment Options for Coarctation of the Aorta
Managing and treating Coarctation of the Aorta (CoA) involves a tailored approach that focuses on alleviating symptoms and correcting the narrowing of the aorta. Treatment options range from non-surgical methods to surgical procedures, each chosen based on the severity of the condition, the patient’s age, and overall health. Here, we delve into the available treatments for CoA, highlighting non-invasive approaches and surgical interventions.
Non-surgical Methods
For mild cases of CoA and in patients where surgery may pose a significant risk, non-surgical methods may offer a viable pathway to managing the condition. These include:
- Medication: Drugs may be prescribed to help control blood pressure, reduce heart muscle thickening, and manage other symptoms associated with CoA. Beta-blockers, ACE inhibitors, and calcium channel blockers are commonly used medications.
- Lifestyle Changes: Adopting a heart-healthy lifestyle can significantly impact the management of CoA. This includes maintaining a healthy weight, engaging in regular physical activity compatible with the individual’s health status, following a balanced diet low in sodium and saturated fats, and avoiding smoking.
- Regular Monitoring: Close and regular monitoring by a healthcare professional is essential for managing the condition without surgery. This includes routine echocardiograms, MRI, or CT scans to monitor the aorta’s condition and blood pressure measurements.
Surgical Procedures
When coarctation significantly affects the aorta or when non-surgical methods are insufficient in managing the condition, surgical intervention becomes necessary. The main goals of surgery are to relieve the narrowing and improve blood flow. Common surgical options include:
- Balloon Angioplasty: This minimally invasive procedure involves inserting a catheter through the blood vessels to the site of the narrowing. A balloon at the catheter’s tip is then inflated to stretch open the narrowed section. Balloon angioplasty is often preferred for treating re-coarctation (narrowing that recurs after initial treatment).
- Stent Placement: Similar to balloon angioplasty, a stent (a small wire mesh tube) is placed at the narrowed area to keep it open. Stent placement is becoming increasingly common and can be used in adolescents and adults.
- Surgical Repair: Open-heart surgery may be required in severe cases or in infants. The narrowed section of the aorta is either removed and the two ends reconnected (resection with end-to-end anastomosis) or repaired with a patch to widen the area (patch aortoplasty).
The outcomes of these surgical procedures are generally positive, with many patients leading healthy lives post-operation. However, long-term follow-up is crucial to monitor for potential complications or recurrence of the narrowing.
However, the management and treatment of Coarctation of the Aorta involve a comprehensive approach that includes both non-surgical methods for mild cases and surgical procedures for more severe forms. Through appropriate management, individuals with CoA can achieve a good quality of life. Regular follow-ups with a healthcare provider are essential to monitor the condition and adjust treatments as necessary.
FAQs: Understanding Coarctation of the Aorta
What is Coarctation of the Aorta?
Coarctation of the aorta (CoA) is a congenital heart defect characterized by the narrowing of the aorta, the major artery carrying blood from the heart to the body. This narrowing can increase blood pressure above the constriction and reduce blood flow to parts of the body below the narrowing.
Who is at Risk for Coarctation of the Aorta?
CoA can occur in any baby but is more common in those with certain genetic conditions, such as Turner syndrome. It’s also more frequently diagnosed in males. A family history of heart defects can also increase the risk.
What are the Symptoms of Coarctation of the Aorta?
Symptoms vary depending on the severity of the condition. In infants, signs may include difficulty breathing, heavy sweating, or poor growth. Older children and adults may experience high blood pressure, headache, muscle weakness, leg cramps, or cold feet.
How is Coarctation of the Aorta Diagnosed?
CoA is diagnosed through various tests, including echocardiograms, MRI, CT scans, and chest X-rays. Doctors also consider the patient’s symptoms and physical examination findings, such as a difference in blood pressure between the arms and legs.
What Treatments are Available for Coarctation of the Aorta?
Treatment depends on the age at diagnosis and the severity of the condition. Options include surgical repair or balloon angioplasty. In some cases, medication may be used to manage symptoms or conditions associated with CoA, such as high blood pressure.
Can Coarctation of the Aorta be Cured?
While surgery or angioplasty can repair the narrowing of the aorta, monitoring for potential long-term complications, such as high blood pressure or re-narrowing of the aorta, is necessary. Regular follow-up with a cardiologist is essential.
Is Exercise Safe for Individuals with Coarctation of the Aorta?
Physical activity is often encouraged, but it’s important for individuals with CoA to discuss their exercise plans with their healthcare provider. Some may need to avoid high-intensity sports.
Can Coarctation of the Aorta Affect Pregnancy?
Women with CoA can have successful pregnancies. However, they are considered high-risk and require careful monitoring by a team of healthcare providers.
Conclusion
In summary, understanding and recognizing the symptoms of Coarctation of the Aorta (CoA) is crucial for early intervention and optimal health outcomes. This condition, characterized by the narrowing of the aorta, can lead to significant health issues if not diagnosed and treated promptly. Symptoms such as high blood pressure, leg fatigue, nosebleeds, and the disparity in pulse and blood pressures between the arms and legs are key indicators that should not be overlooked.
Early detection of CoA plays a pivotal role in managing and treating the condition effectively, preventing potential complications such as heart failure, aortic rupture, or stroke. It underscores the importance of awareness and knowledge about the symptoms associated with this congenital heart defect.
We strongly encourage anyone who suspects they or someone they know might be showing signs of Coarctation of the Aorta to seek professional medical advice immediately. Consulting with a healthcare provider can lead to timely diagnosis and appropriate treatment, significantly improving the prognosis for individuals affected by this condition.
Remember, your health and well-being are paramount. Taking proactive steps towards identifying and addressing symptoms of CoA can make a substantial difference in your life or the life of someone you care about. Don’t hesitate to reach out for medical support when needed—it could be a decision that saves a life.