Chronic Pelvic Pain Treatment: Chronic pelvic pain (CPP) presents a significant challenge to healthcare professionals due to its complex etiology and the impact it has on patients’ quality of life.
Addressing CPP requires a multidisciplinary approach that encompasses accurate diagnosis and tailored treatment strategies.
This article delves into the nuances of diagnosing CPP and outlines the most effective treatments available, aiming to provide a comprehensive resource for individuals seeking relief from this condition.
What is Chronic Pelvic Pain?
Chronic Pelvic Pain (CPP) is a complex condition that affects both men and women, characterized by persistent pain in the lower abdomen and pelvic area that lasts for six months or longer. This pain can significantly impact an individual’s daily activities, mental health, and overall quality of life. Unlike acute pain, which serves as a warning signal for the body to react to an injury or illness, chronic pelvic pain can persist long after the initial cause has healed or may occur without any apparent reason.
Epidemiology and Significance
Chronic Pelvic Pain is a prevalent health issue with a substantial impact on individuals and healthcare systems worldwide. Studies estimate that CPP affects approximately 15% to 20% of women in the United States aged 18 to 50, and a smaller percentage of men also suffer from this condition. The prevalence of CPP contributes to a significant number of medical visits each year, emphasizing its importance as a public health concern. The condition not only leads to high healthcare costs but also affects the productivity and quality of life of those affected, making it a critical area for medical research and healthcare intervention.
Common Symptoms and How They Affect Quality of Life
Chronic Pelvic Pain manifests in various ways, with symptoms that can vary widely from person to person. Some of the most common symptoms include:
- Persistent Lower Abdominal Pain: This can range from a dull ache to sharp pains that may fluctuate in intensity.
- Pain During Intercourse: Often described as deep pain during or after sexual activity.
- Painful Menstruation: Severe cramping and pelvic pain before and during menstrual periods.
- Urinary Symptoms: Such as urgency, frequency, or pain during urination.
- Gastrointestinal Symptoms: Including bloating, constipation, or diarrhea.
- Musculoskeletal Pain: In the pelvic floor, hips, or lower back.
These symptoms can severely affect an individual’s quality of life by:
- Impairing Physical Function: Pain and discomfort can limit mobility and the ability to perform daily activities, contributing to a sedentary lifestyle and physical deconditioning.
- Affecting Mental Health: Chronic pain is associated with increased rates of anxiety, depression, and other mental health disorders due to its persistent nature and the stress it causes.
- Disrupting Social and Family Life: Pain during intercourse can strain intimate relationships, while the constant management of symptoms can affect social interactions and responsibilities.
- Economic Impact: Frequent medical appointments and treatments, along with reduced productivity, can lead to significant financial strain on individuals and their families.
Understanding Chronic Pelvic Pain, its epidemiology, symptoms, and the profound effects it can have on quality of life is crucial for patients, healthcare providers, and the community. It highlights the need for effective management strategies, supportive care, and ongoing research to improve outcomes for those affected by this challenging condition.
Causes of Chronic Pelvic Pain
The potential causes of CPP is crucial for accurate diagnosis and effective treatment. This article will explore the various conditions that can contribute to the development of chronic pelvic pain, shedding light on how these conditions intersect with CPP.
List of Potential Causes
- Endometriosis: This condition occurs when tissue similar to the lining inside the uterus grows outside of it, often causing severe pain and fertility problems. Endometriosis is a leading cause of CPP, as the misplaced tissue can lead to inflammation and scarring.
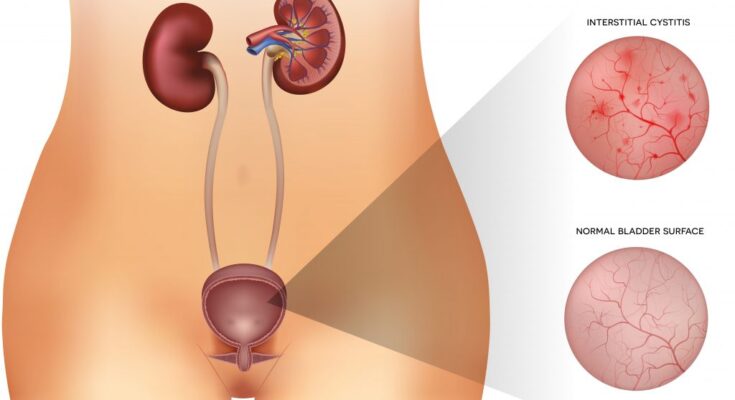
- Interstitial Cystitis (Painful Bladder Syndrome): A chronic condition characterized by bladder pressure, bladder pain, and sometimes pelvic pain, ranging from mild discomfort to severe pain.
- Pelvic Inflammatory Disease (PID): An infection of the female reproductive organs, often caused by sexually transmitted bacteria, can lead to significant pelvic pain if left untreated.
- Ovarian Cysts: Fluid-filled sacs within or on the surface of an ovary can cause pelvic pain, especially if they rupture or cause the ovary to move from its usual position.
- Fibroids: Noncancerous growths in the uterus can cause a heavy or painful sensation in the lower abdomen or pelvic area.
- Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS) in Men: A long-standing inflammation of the prostate gland, causing pelvic pain and urinary symptoms in men.
- Pelvic Adhesions: Bands of scar tissue that bind organs after pelvic infection, appendicitis, or surgery can cause ongoing pelvic pain.
- Irritable Bowel Syndrome (IBS): A disorder affecting the large intestine, causing cramping, abdominal pain, bloating, gas, and diarrhea or constipation, can contribute to CPP.
How These Conditions Contribute to CPP
Each of these conditions contributes to chronic pelvic pain through various mechanisms, often involving inflammation, structural changes, or nerve sensitivity. For example, endometriosis leads to CPP through the formation of inflammatory lesions and scar tissue that can cause pain during menstrual cycles and sexual activity. Similarly, conditions like interstitial cystitis affect the bladder’s lining, leading to persistent pain and pressure sensations.
Conditions such as pelvic inflammatory disease and ovarian cysts contribute to CPP by causing acute episodes of pain that can evolve into chronic conditions if not properly treated. Fibroids and pelvic adhesions physically alter pelvic anatomy, which can lead to discomfort and pain due to pressure on surrounding tissues and organs.
Furthermore, chronic prostatitis in men and irritable bowel syndrome affect CPP by inducing chronic inflammation and discomfort in the pelvic region, highlighting the interconnectivity of pelvic health and overall well-being.
Diagnosing Chronic Pelvic Pain
Chronic pelvic pain (CPP) is a complex condition that can significantly impact a person’s quality of life. Accurate diagnosis is crucial for effective treatment. This guide outlines the key steps in diagnosing CPP, ensuring the process is thorough and patient-focused.
Initial Assessment and Medical History
The first step in diagnosing chronic pelvic pain involves a detailed initial assessment and medical history. Healthcare professionals will ask about the pain’s characteristics, including its location, duration, intensity, and any factors that alleviate or exacerbate it. Understanding the patient’s medical history, including previous surgeries, infections, or treatments, is essential. This comprehensive approach helps to identify underlying conditions and guide further diagnostic steps.
Physical Examination Specifics
Following the initial assessment, a targeted physical examination is conducted. This examination focuses on the abdominal and pelvic areas to identify any abnormalities or signs of underlying conditions. It may involve checking for tenderness, masses, or other physical signs that could indicate the source of pain. The physical examination is a critical step in the diagnostic process, providing valuable insights that support the overall assessment.
Diagnostic Tests and Procedures
To further investigate chronic pelvic pain, healthcare providers may recommend several diagnostic tests and procedures. Key among these are:
- Pelvic Ultrasound: A non-invasive imaging test that uses sound waves to create pictures of the organs within the pelvic region. It helps in identifying abnormalities such as cysts, fibroids, and other potential sources of pain.
- Laparoscopy: A minimally invasive surgical procedure that allows doctors to see inside the pelvic area. Using a camera inserted through a small incision, laparoscopy can diagnose conditions like endometriosis, adhesions, or pelvic inflammatory disease.
These tests are essential for making an accurate diagnosis and formulating an effective treatment plan.
The Role of Differential Diagnosis
Differential diagnosis plays a pivotal role in diagnosing chronic pelvic pain. This process involves considering and ruling out multiple potential conditions that could cause the symptoms. By systematically evaluating each possibility—based on the patient’s history, physical examination, and diagnostic tests—healthcare providers can narrow down the cause of the pain. This method ensures a comprehensive approach, reducing the risk of overlooking an underlying condition and allowing for targeted treatment.
Diagnosing chronic pelvic pain is a detailed process that requires a patient-centered approach. Through careful assessment, physical examination, and the use of specific diagnostic tests and procedures, healthcare professionals can identify the underlying causes of CPP. The role of differential diagnosis is crucial in this context, ensuring a thorough evaluation and the formulation of an effective treatment plan. Understanding these steps can empower patients and clinicians alike, leading to improved outcomes and quality of life for those affected by chronic pelvic pain.
Treatment Options for Chronic Pelvic Pain
There are various treatment options available, ranging from non-pharmacological and pharmacological methods to surgical interventions and alternative therapies. Understanding these treatments can empower individuals to work with their healthcare providers in finding the most effective strategy for managing their symptoms.
Non-pharmacological Treatments
Non-pharmacological treatments focus on alleviating pain without medication. These options often serve as the first line of defense in managing chronic pelvic pain and include:
- Physical Therapy: Tailored exercises and manual techniques can improve pelvic floor muscle function, reducing pain and discomfort.
- Psychological Support: Counseling or cognitive-behavioral therapy can help individuals cope with the psychological impact of chronic pain, addressing any associated anxiety or depression.
- Lifestyle Modifications: Changes in diet, exercise, and daily activities can significantly impact pain levels. Identifying and avoiding triggers that exacerbate pain is also crucial.
Pharmacological Treatments
When non-pharmacological methods are insufficient, medications may be prescribed to manage pain more effectively. These include:
- Pain Relievers: Over-the-counter (OTC) pain medications, such as ibuprofen or acetaminophen, can help manage mild to moderate pain.
- Antidepressants: Certain antidepressants have been found to be effective in managing chronic pain, even in the absence of depression.
- Anticonvulsants: Originally designed to treat epilepsy, these drugs can also help in managing nerve pain associated with CPP.
Surgical Interventions
Surgery may be considered when other treatments have failed to provide relief, especially if there’s an identifiable cause of the pain that can be corrected surgically. Options include:
- Laparoscopy: A minimally invasive surgery used to diagnose and sometimes treat sources of pelvic pain, such as endometriosis or adhesions.
- Hysterectomy: The removal of the uterus may be considered in severe cases, particularly when other treatments have not been effective and the individual does not plan to have children.
Alternative and Complementary Therapies
Many individuals find relief through alternative and complementary therapies, which can be used alongside conventional treatments. These include:
- Acupuncture: This traditional Chinese medicine technique involves inserting thin needles into specific body points to relieve pain.
- Biofeedback: A technique that teaches control over muscle tension, blood flow, and pain perception through real-time feedback from physiological sensors.
- Herbal Supplements: Certain herbs and supplements are believed to offer pain relief, though it’s important to discuss these with a healthcare provider to avoid interactions with other treatments.
However, managing chronic pelvic pain often requires a multifaceted approach. Collaboration with healthcare providers, openness to a variety of treatment options, and patience in finding the right combination of therapies are key to effectively managing CPP. Always consult with a healthcare professional before starting any new treatment to ensure it’s safe and suitable for your specific situation.
Managing Chronic Pelvic Pain
Effective management of chronic pelvic pain requires a comprehensive strategy that includes a multidisciplinary approach, patient education, and the adoption of self-care techniques. In this section, we will explore these key components to provide a guide on managing chronic pelvic pain effectively.
Strategies for Pain Management
The first step in managing chronic pelvic pain is to establish a pain management strategy that is personalized to the individual’s needs. This often involves a combination of medical treatments and lifestyle modifications. Medications, such as non-steroidal anti-inflammatory drugs (NSAIDs), pain relievers, and hormone therapies, may be prescribed to alleviate symptoms. Additionally, physical therapy can be crucial in strengthening pelvic floor muscles and reducing discomfort.
Alternative therapies, such as acupuncture, massage therapy, and biofeedback, have also shown promise in managing pelvic pain. These treatments can help reduce stress levels, which may, in turn, decrease pain perception. It’s essential for individuals to work closely with their healthcare providers to find the most effective combination of treatments for their specific situation.
Importance of a Multidisciplinary Approach
A multidisciplinary approach is vital in the management of chronic pelvic pain. This approach involves the collaboration of various healthcare professionals, including gynecologists, urologists, pain management specialists, physical therapists, and mental health professionals. Each specialist brings a unique perspective and expertise, ensuring a comprehensive evaluation and treatment plan.
The multidisciplinary approach not only addresses the physical aspects of pelvic pain but also considers the psychological, social, and emotional factors contributing to the condition. By addressing these multiple dimensions, patients are more likely to experience significant improvements in their quality of life.
Patient Education and Self-Care Techniques
Educating patients about chronic pelvic pain and its management is crucial for empowering them to take an active role in their treatment. Understanding the condition helps demystify the pain and reduces anxiety related to symptoms. Healthcare providers should offer resources and tools for patients to learn about their condition, treatment options, and strategies for coping with pain.
Self-care techniques play a significant role in managing chronic pelvic pain. Patients should be encouraged to adopt healthy lifestyle habits, such as regular exercise, a balanced diet, and sufficient sleep, which can help mitigate pain symptoms. Stress reduction techniques, such as mindfulness, meditation, and yoga, can also be beneficial in managing the emotional aspects of chronic pain.
Practicing pelvic floor relaxation exercises can specifically target the muscles affected by chronic pelvic pain, offering relief and improving function. Additionally, heat therapy, such as warm baths or heating pads, can provide temporary pain relief and comfort.
However, managing chronic pelvic pain effectively requires a holistic and personalized approach. By combining medical treatments, adopting a multidisciplinary strategy, and emphasizing patient education and self-care, individuals can achieve better pain management and improve their overall quality of life. Collaboration between patients and healthcare providers is essential to tailor the management plan to meet the unique needs of each individual, offering hope and support to those affected by chronic pelvic pain.
Emerging Therapies and Research in Chronic Pelvic Pain Treatment
The landscape of chronic pelvic pain management is evolving rapidly, with emerging therapies and ongoing research opening new avenues for relief and recovery. In this section, we will delve into the latest advancements in chronic pelvic pain treatment, as well as highlight ongoing research and clinical trials that promise to reshape our understanding and approach to this debilitating condition.
Latest Advancements in Chronic Pelvic Pain Treatment
In recent years, the field of chronic pelvic pain treatment has seen remarkable progress, with new therapies emerging that target the condition more effectively and with fewer side effects. One significant advancement is the development of neuromodulation techniques, such as transcutaneous electrical nerve stimulation (TENS) and spinal cord stimulation (SCS). These methods work by altering nerve activity to reduce pain signals sent to the brain, offering relief to many patients who have found little success with traditional treatments.
Another promising area is the use of minimally invasive surgical techniques for conditions that contribute to CPP, such as endometriosis and pelvic varicosities. These surgeries aim to remove or alleviate the source of pain with less recovery time and lower risk of complications, improving the quality of life for sufferers.
Pharmacological advances also play a crucial role, with new medications and compound therapies being developed to target pain more effectively. This includes the use of certain antidepressants and anticonvulsants that have shown efficacy in reducing neuropathic pain associated with CPP.
Ongoing Research and Clinical Trials
The horizon of chronic pelvic pain treatment is further expanded by ongoing research and clinical trials that aim to uncover the underlying mechanisms of CPP and explore new treatment modalities. Several studies are focused on understanding the role of the central nervous system in CPP to develop targeted therapies that can address the neurogenic aspect of the pain.
Clinical trials are also investigating the efficacy of alternative and complementary therapies, such as acupuncture, yoga, and mindfulness meditation, in managing CPP symptoms. These approaches emphasize a more holistic view of pain management, integrating physical, emotional, and psychological aspects of health.
Additionally, research into the role of hormones and inflammation in CPP could lead to novel treatments that address these systemic factors. This includes the exploration of anti-inflammatory diets, supplements, and hormone therapy as potential tools for managing chronic pelvic pain.
The landscape of chronic pelvic pain treatment is undoubtedly evolving, with emerging therapies and ongoing research offering hope to those affected. As our understanding of CPP deepens, the development of more effective and personalized treatment strategies becomes possible, promising a future where chronic pelvic pain can be managed more successfully.
However, the progress in emerging therapies and research in the field of chronic pelvic pain is a testament to the dedication of the medical community to tackle this challenging condition. With continued advancements and a growing body of evidence, the goal of achieving better outcomes for CPP patients is within reach, marking a new era in the management of chronic pelvic pain.
Finding Support and Resources for Chronic Pelvic Pain
Living with chronic pelvic pain (CPP) can be challenging, but finding the right support and resources can make a significant difference. Whether you’re looking for understanding communities or practical tools to manage your condition, a wealth of options are available. This section will guide you through navigating support groups, communities, and online resources tailored to those experiencing CPP, ensuring you have the support you need to manage your symptoms effectively.
Support Groups and Communities
Joining a support group or community can be incredibly beneficial for individuals dealing with chronic pelvic pain. These groups offer a sense of belonging, understanding, and shared experiences. They can provide emotional support, practical advice, and insights into managing your condition. Here’s how to find them:
- Local Support Groups: Check with hospitals, clinics, and community centers in your area. Many offer meetings for individuals with various chronic conditions, including CPP.
- Online Forums and Social Media: Platforms like Reddit, Facebook, and specialized health forums host numerous CPP-focused groups. These online communities are accessible 24/7, allowing you to connect with others from the comfort of your home.
- Nonprofit Organizations: Organizations dedicated to pelvic pain awareness and support often have directories of support groups and community resources, both online and in-person.
When joining these groups, look for environments that are positive, inclusive, and focused on constructive support. Everyone’s experience with CPP is unique, so finding a group that respects individual differences is key.
Online Resources and Tools for Managing Chronic Pelvic Pain
In addition to support groups, various online resources and tools can help you manage CPP more effectively. These include:
- Educational Websites: Reputable medical websites like Mayo Clinic, WebMD, and specific nonprofit organizations focused on pelvic pain offer articles, research updates, and management tips.
- Pain Management Apps: Apps designed to track pain levels, triggers, and effective relief strategies can be instrumental in managing CPP. They can help you identify patterns in your pain and effectiveness of various treatments or activities.
- Online Therapy and Counseling Services: Mental health support is crucial for managing chronic pain. Online platforms provide access to therapists specializing in chronic pain management, offering coping strategies and emotional support.
- Webinars and Online Workshops: Many organizations and health professionals offer online learning opportunities. These can include webinars on pain management techniques, mental health support, and lifestyle adjustments to alleviate symptoms.
Finding the right combination of support and resources for chronic pelvic pain may take time, but it’s a crucial step toward managing your condition and improving your quality of life. Remember, you’re not alone in this journey—there’s a community and a wealth of information out there to support you every step of the way.
By leveraging these support groups, communities, and online tools, you can gain the knowledge and emotional support needed to navigate the complexities of CPP. Always consult with healthcare professionals before making significant changes to your management plan, and use these resources to complement their advice.
Conclusion:
If you’re experiencing symptoms of CPP, it’s crucial to seek professional help. Healthcare professionals are equipped with the knowledge and tools to provide comprehensive care. By collaborating closely with your doctor, exploring various treatment options, and possibly integrating multidisciplinary approaches, you can pave the way towards significant relief and recovery. Remember, reaching out for help is a sign of strength. It’s the first step towards understanding your condition and navigating the path to wellness.
Looking towards the future, there’s optimism in the field of CPP treatment. Advances in medical research are continuously uncovering new insights into the causes and mechanisms behind chronic pelvic pain. These developments promise more effective, personalized treatment strategies. From innovative medications and therapies to cutting-edge surgical techniques, the future holds the potential for even greater successes in managing CPP. Furthermore, the growing emphasis on patient-centered care and holistic approaches underscores a comprehensive strategy to address not only the physical but also the emotional and psychological aspects of CPP.
In conclusion, while the journey with Chronic Pelvic Pain may seem daunting, there’s a wealth of support and an ever-expanding array of treatment options available. With the right help, individuals can navigate this challenging path and look forward to a future where pain does not define their existence. Let’s embrace the advancements in medical science with optimism and continue to advocate for compassionate, individualized care.