Chronic Granulomatous Disease Symptoms: Chronic Granulomatous Disease (CGD) is a rare and complex immune deficiency disorder that significantly impacts the lives of those affected and their families.
This article provides an in-depth analysis of the symptoms and causes of CGD, with the aim of offering comprehensive information that can help individuals better understand this condition.
What is Chronic Granulomatous Disease?
Chronic Granulomatous Disease (CGD) is a rare and inherited disorder that severely impairs the immune system’s ability to fight off certain infections. This condition primarily affects white blood cells, which play a crucial role in protecting the body against bacteria and fungi. Individuals with CGD are more susceptible to infections that would be relatively harmless to people with a fully functioning immune system.
Brief History and Prevalence
The medical community first identified CGD in the mid-20th century, with formal documentation of the disease occurring in the 1950s. Since then, ongoing research has helped to understand the genetic mutations responsible for CGD, leading to advancements in diagnosis and treatment. Although CGD is considered rare, affecting about 1 in 200,000 to 250,000 individuals worldwide, its exact prevalence may vary across different populations and regions.
How CGD Affects the Immune System
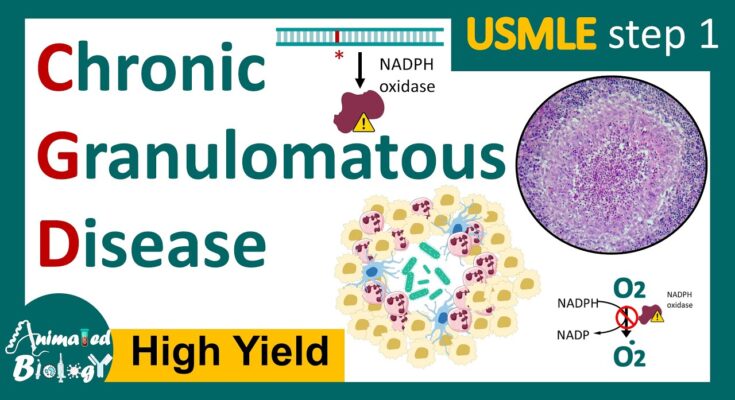
CGD is caused by mutations in the genes responsible for producing certain proteins that white blood cells need to generate reactive oxygen species. These reactive oxygen species are crucial for killing bacteria and fungi. Without this critical defense mechanism, individuals with CGD have compromised immune systems, making them more vulnerable to infections. The hallmark of CGD is the formation of granulomas, which are clusters of immune cells that form in response to chronic inflammation, often in response to an infection that the body cannot clear.
These granulomas can form anywhere in the body, leading to a range of symptoms depending on their location, such as skin abscesses, pneumonia, gastrointestinal issues, and more. The inability to effectively deal with infections means that people with CGD require lifelong management of the condition, including preventive antibiotics, antifungal medications, and in some cases, bone marrow transplants.
Understanding CGD is crucial for early diagnosis and treatment, which can significantly improve the quality of life for those affected by this condition. Ongoing research continues to offer hope for better treatments and potentially a cure in the future.
Symptoms of Chronic Granulomatous Disease (CGD)
The symptoms of CGD is crucial for early diagnosis and management. This article provides a comprehensive overview of the common and uncommon symptoms of CGD, as well as a comparison of symptoms observed in children and adults.
Common Symptoms of CGD
Patients with CGD typically exhibit symptoms related to infections caused by bacteria and fungi that a healthy immune system would ordinarily be able to combat. The most common symptoms include:
- Frequent Infections: These can be of the skin, lungs, lymph nodes, liver, and gastrointestinal tract. Infections are more severe and recur despite treatment.
- Granulomas: Inflammatory masses or nodules called granulomas can form in various organs, potentially causing blockages or disruption in normal organ function.
- Skin Issues: Skin infections, abscesses, and dermatitis are frequent. Patients might notice boils, rashes, or other skin abnormalities that do not heal with standard treatments.
- Respiratory Problems: Recurrent pneumonia, bronchitis, and other respiratory infections are common, often leading to chronic cough or difficulty breathing.
- Gastrointestinal Complaints: Symptoms can include stomach pain, diarrhea, nausea, and vomiting. In some cases, granulomas in the gastrointestinal tract can lead to blockages.
Uncommon or Rare Symptoms
While the above symptoms are more frequently observed, CGD can also present with less common manifestations, which include:
- Autoimmune Disorders: Some patients develop autoimmune disorders such as lupus, rheumatoid arthritis, or Crohn’s disease.
- Growth Delays: Children with CGD may experience growth delays or failure to thrive due to frequent infections and chronic inflammation.
- Eye Infections: Rarely, CGD can lead to infections in the eyes, causing symptoms like irritation, redness, and vision problems.
Comparison of Symptoms in Children and Adults
The presentation of CGD symptoms can vary between children and adults, although there is considerable overlap:
- Children: Symptoms in children often appear early in life, sometimes shortly after birth. Frequent and severe infections are the most common signs, along with growth delays. Children may also be more susceptible to skin and respiratory infections.
- Adults: While adults can experience the same range of symptoms as children, they may also face complications from long-standing inflammation, such as granuloma formation in various organs. Autoimmune disorders and certain types of cancers may be more common in adults with CGD.
Understanding the spectrum of symptoms associated with Chronic Granulomatous Disease is essential for prompt diagnosis and treatment. Early intervention can significantly improve the quality of life for individuals with CGD. If you or someone you know is experiencing symptoms consistent with CGD, it is important to consult a healthcare provider for a comprehensive evaluation.
Causes of Chronic Granulomatous Disease
The causes of CGD involves delving into its genetic background, the role of genes, inheritance patterns, the effects of genetic mutations on immune cell function, and the impact of environmental factors on the severity of the disease. This article aims to elucidate these aspects in an SEO and readability-friendly manner.
Genetic Background of CGD
CGD is primarily caused by mutations in genes that are crucial for the proper functioning of certain immune system cells. These mutations affect the cells’ ability to produce reactive oxygen species (ROS), which are essential for killing bacteria and fungi. Without this ability, individuals with CGD are more susceptible to infections, particularly from certain bacteria and fungi that would otherwise be easily managed by a healthy immune system.
The Role of Genes in CGD
The genes implicated in CGD are those that encode components of the NADPH oxidase enzyme complex. This complex is responsible for generating the ROS needed to combat pathogens. The most common mutations are found in the CYBB gene on the X chromosome, which accounts for the X-linked pattern of inheritance seen in the majority of CGD cases. Other mutations can occur in genes that are autosomal (not on the X chromosome), leading to autosomal recessive forms of CGD.
Inheritance Patterns
CGD can be inherited in two primary patterns: X-linked and autosomal recessive. X-linked CGD is the most prevalent form and occurs almost exclusively in males. This is because males have only one X chromosome, and a single mutated gene on this chromosome can cause the disease. Females, having two X chromosomes, are typically carriers unless both X chromosomes carry the mutation, which is extremely rare. Autosomal recessive CGD, on the other hand, requires both parents to pass on a copy of the mutated gene. Individuals with this form of CGD can be of any gender.
How Genetic Mutations Affect Immune Cell Function
The mutations that cause CGD disrupt the function of phagocytes, a type of white blood cell crucial for the immune response. Normally, phagocytes engulf pathogens and then use ROS to destroy them. In CGD, due to the genetic mutations, the NADPH oxidase complex does not function correctly, preventing the phagocytes from producing ROS. This defect leaves individuals vulnerable to infections, as their immune system cannot effectively eliminate certain bacteria and fungi.
Environmental Factors and Their Impact on CGD Severity
While the primary cause of CGD is genetic, environmental factors can influence the severity and frequency of infections in individuals with the disease. Exposure to certain pathogens, particularly in environments where specific bacteria and fungi are more prevalent, can lead to more severe or frequent infections. Additionally, lifestyle choices and medical interventions that enhance overall health can mitigate some of the risks associated with CGD, such as vaccinations and prophylactic antibiotics to prevent infections.
Understanding the causes of CGD is crucial for managing the disease effectively. Advances in genetic research and improved environmental management strategies offer hope for better outcomes for individuals with CGD. By exploring the genetic underpinnings and acknowledging the role of environmental factors, we move closer to more effective treatments and, ultimately, a cure for this challenging condition.
Diagnosing Chronic Granulomatous Disease
Diagnosing CGD is crucial for managing its symptoms and preventing severe infections. Below, we explore the various diagnostic methods and underscore the importance of early diagnosis.
List of Diagnostic Methods
- Nitroblue Tetrazolium (NBT) Test: The NBT test is a cornerstone in diagnosing CGD. It measures the ability of neutrophils (a type of white blood cell) to produce reactive oxygen species to kill bacteria. In individuals with CGD, these cells cannot generate reactive oxygen, resulting in a negative NBT test.
- Dihydrorhodamine 123 (DHR) Flow Cytometry Test: This test is more sensitive and specific than the NBT test. It assesses the neutrophils’ oxidative burst activity, which is impaired in CGD patients. The DHR test is particularly useful for identifying female carriers of the disease and differentiating CGD from other phagocyte disorders.
- Genetic Testing: Since CGD is a genetic disorder, identifying mutations in the genes responsible for the disease can confirm the diagnosis. Genetic testing is valuable for familial screening and prenatal diagnosis.
- Immunoblotting and Cytochrome c Reduction Test: These tests evaluate the presence and function of certain proteins essential for the oxidative burst in phagocytes. They help in identifying specific subtypes of CGD, which is critical for personalized treatment approaches.
The Importance of Early Diagnosis
Early diagnosis of CGD is vital for several reasons:
- Preventing Infections: Early intervention can help prevent the occurrence of severe, life-threatening infections. Prophylactic antibiotics and antifungal medications, along with interferon-gamma therapy, can significantly reduce the risk of infections in CGD patients.
- Improving Quality of Life: Timely diagnosis allows for the management of CGD symptoms and complications, thereby improving the overall quality of life for affected individuals.
- Guiding Treatment Plans: Identifying CGD early helps in planning appropriate treatments, including hematopoietic stem cell transplantation (HSCT), which can be curative in some cases.
- Family Planning: For families with a history of CGD, early diagnosis in affected members can inform future family planning decisions and allow for genetic counseling.
However, diagnosing Chronic Granulomatous Disease involves a series of specialized tests that assess the function of the immune system’s neutrophils. Early and accurate diagnosis is crucial for effective management, prevention of severe infections, and improvement in the quality of life for those affected by CGD. Through advancements in diagnostic methods, individuals with CGD can receive the care and treatment they need to lead healthier lives.
Management and Treatment Options for Chronic Granulomatous Disease (CGD)
Managing CGD involves a comprehensive approach that includes current medical treatments, lifestyle adjustments, and continuous monitoring by healthcare professionals. Here, we explore the various strategies for managing and treating CGD, aiming to enhance the quality of life for individuals living with this condition.
Current Treatments for CGD
Antibiotics and Antifungals: Preventative medication is fundamental in managing CGD. Regular use of antibiotics and antifungal medications can help prevent infections that people with CGD are susceptible to.
Interferon-gamma (IFN-γ): This synthetic version of a naturally occurring protein boosts the immune system. IFN-γ is administered several times a week to help prevent infections.
Corticosteroids: In cases of severe inflammation caused by the overactive immune response in CGD, corticosteroids can be prescribed to reduce inflammation.
Hematopoietic Stem Cell Transplantation (HSCT): For some individuals, HSCT (also known as bone marrow transplant) offers a potential cure by replacing the defective immune cells with healthy ones from a donor. This option depends on the availability of a suitable donor and the patient’s overall health condition.
Gene Therapy: Although still in the experimental phase for CGD, gene therapy holds promise as a future treatment option by correcting the genetic defect responsible for the disease.
Lifestyle and Home Care Strategies
Living with CGD requires adjustments to minimize exposure to infections and maintain overall health:
Avoid Infection Risks: Simple measures like regular handwashing, avoiding unpasteurized foods, and staying clear of environments with a high risk of fungal exposure (such as construction sites) can significantly reduce infection risks.
Healthy Diet: A balanced diet rich in fruits, vegetables, and whole grains supports the immune system.
Regular Exercise: Engaging in moderate exercise, as recommended by a healthcare provider, can improve overall health without overstraining the immune system.
The Role of Regular Monitoring and Healthcare Team
Continuous monitoring is crucial in managing CGD effectively:
Regular Check-ups: Frequent visits to a healthcare provider specializing in immunodeficiency disorders allow for the timely adjustment of treatments and the early detection of infections or inflammation.
Immunization: Keeping up with vaccinations, under the guidance of a healthcare provider, is important for preventing certain infections.
Multi-disciplinary Team: Managing CGD often involves a team of specialists, including immunologists, infectious disease experts, and other healthcare professionals, to address the various aspects of the disease comprehensively.
With the right strategies and a dedicated healthcare team, individuals with CGD can lead fulfilling lives. It’s essential for patients and their families to stay informed about the latest developments in CGD treatment and care to navigate the challenges of this condition effectively.
Living with Chronic Granulomatous Disease (CGD) presents unique challenges and requires comprehensive management strategies to ensure a quality life. Individuals diagnosed with CGD, a rare genetic disorder that affects the immune system, need to navigate daily life with caution and awareness. However, with the right support systems and an eye on the future of medical advancements, managing CGD can become more manageable and hopeful.
Daily Life and Management
Managing CGD involves a multifaceted approach that includes regular medical care, adherence to treatments, and lifestyle adjustments to minimize infection risks. Patients and their caregivers must be vigilant in recognizing signs of infection, as individuals with CGD are more susceptible to bacterial and fungal infections. This vigilance extends to everyday activities, dietary choices, and personal hygiene practices to reduce exposure to potential pathogens.
Prophylactic antibiotics and antifungal medications are often prescribed to prevent infections before they start. Immunoglobulin replacement therapy may also be recommended to boost the immune system. Additionally, advancements in gene therapy and stem cell transplantation offer promising treatment avenues, though these options are considered on a case-by-case basis.
Support Systems: Family, Community, and Online Resources
The role of support systems in managing CGD cannot be overstated. Family members play a critical role in providing emotional and physical support. From accompanying patients to medical appointments to assisting in the administration of daily medications, the support from family is invaluable.
Beyond the family unit, community support groups offer a network of understanding and resources. These groups provide a platform for sharing experiences, tips, and encouragement. They can be a vital source of information on managing the practical aspects of living with CGD.
In the digital age, online resources have become an indispensable tool for individuals with CGD and their families. Websites, forums, and social media groups dedicated to CGD offer access to a global community of individuals facing similar challenges. These online platforms provide an opportunity to connect, share knowledge, and find emotional support from people around the world.
Future Outlook: Research and Advancements in CGD Treatment
The future outlook for CGD treatment is brighter today than ever before, thanks to ongoing research and technological advancements. Scientists are continuously working on understanding the genetic and molecular basis of CGD, which paves the way for innovative treatments and potentially a cure.
Emerging gene therapy techniques offer hope for correcting the genetic defects that cause CGD. While still in the experimental phase, these therapies have the potential to provide long-lasting solutions for individuals with CGD. Additionally, advances in stem cell transplantation, particularly in the use of matched unrelated donors, have shown promising results in curing CGD.
As research progresses, it’s essential for patients and families to stay informed about the latest developments in CGD treatment. Participating in clinical trials may also provide access to cutting-edge therapies and contribute to the advancement of medical knowledge.
However, living with Chronic Granulomatous Disease requires careful daily management, a strong support network, and optimism about future medical advancements. Through diligent care, community support, and staying informed about treatment options, individuals with CGD can lead fulfilling lives while looking forward to a future where this condition can be more effectively treated or even cured.
FAQs about Chronic Granulomatous Disease
What is Chronic Granulomatous Disease (CGD)?
Chronic Granulomatous Disease (CGD) is a rare, genetic disorder that affects the immune system. It occurs due to mutations in the genes responsible for the production of certain proteins needed by immune cells (phagocytes) to produce reactive oxygen species that kill bacteria and fungi. Individuals with CGD have difficulty fighting off infections, leading to frequent and sometimes severe infections.
How is CGD diagnosed?
CGD is usually diagnosed through a series of tests that evaluate the function of the immune system’s phagocytes. The most common test is the dihydrorhodamine 123 (DHR) flow cytometry test, which measures the production of reactive oxygen species by neutrophils. Genetic testing can also identify mutations in the genes associated with CGD, confirming the diagnosis.
What are the symptoms of CGD?
Symptoms of CGD can vary widely but typically include recurrent infections, such as pneumonia, abscesses, and infections of the skin or organs. Granulomas, which are masses or nodules resulting from chronic inflammation, may also form in various parts of the body, causing complications like blockages or organ dysfunction.
Can CGD be cured?
While there is no cure for CGD, treatments are available to help manage symptoms and reduce the frequency of infections. These treatments may include antibiotics, antifungal medications, and interferon-gamma therapy. In some cases, a hematopoietic stem cell transplant (HSCT) may offer a potential cure by replacing the defective immune cells with healthy ones from a donor.
Is CGD contagious?
No, CGD is not contagious. It is a genetic disorder passed down from parents to their children. The condition itself cannot be transmitted from one person to another.
How is CGD inherited?
CGD is most commonly inherited in an X-linked recessive pattern, which means the defective gene is located on the X chromosome. Males, having only one X chromosome, are more frequently affected when they inherit the defective gene from their mothers. Females can be carriers if they have one defective gene, but they usually do not show symptoms because they have a second, normal X chromosome as a backup. However, CGD can also be inherited in an autosomal recessive pattern, affecting both males and females equally, where both parents must carry and pass on the defective gene.
What is the life expectancy for someone with CGD?
With advances in medical care and treatments, individuals with CGD can lead longer, healthier lives than in the past. Life expectancy varies depending on the severity of the disease, the frequency and type of infections, and how well the condition is managed. Regular follow-up with healthcare providers and adherence to treatment plans are crucial for improving outcomes.
How can I support someone with CGD?
Supporting someone with CGD involves understanding their needs and helping them manage their health. This can include reminding them to take their medications, accompanying them to doctor appointments, and being mindful of their increased risk of infections. Emotional support and understanding are also vital, as living with a chronic condition can be challenging.
Conclusion
In summary, recognizing the symptoms of Chronic Granulomatous Disease, understanding its causes, and seeking medical advice are pivotal steps in managing this condition. The advancements in medical research and treatment options offer hope and demonstrate the power of scientific progress.
Let’s remain informed and supportive of those affected by CGD, as we look forward to a future where this disease can be more effectively treated or even cured.