Chronic Granulomatous Disease Treatment: Chronic Granulomatous Disease (CGD) is a rare, inherited immunodeficiency disorder that affects the body’s ability to fight off certain infections.
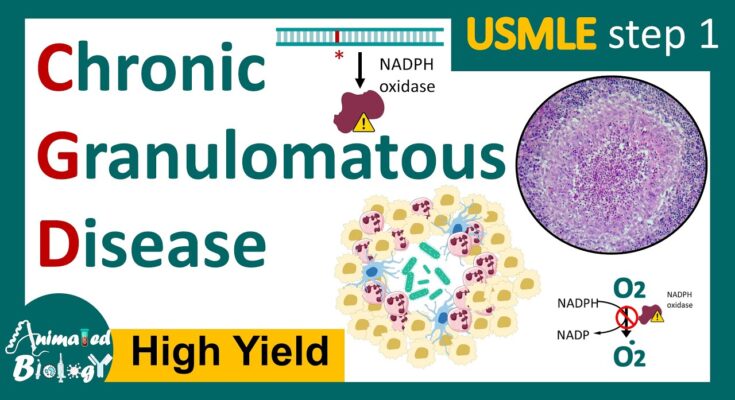
This condition is characterized by the inability of phagocytes, a type of white blood cell, to produce reactive oxygen species (ROS) necessary for killing bacteria and fungi.
As a result, individuals with CGD are more susceptible to infections, particularly those caused by certain bacteria and fungi that are otherwise harmless to people with normal immune systems.
What is Chronic Granulomatous Disease
Chronic Granulomatous Disease (CGD) is a rare and inherited disorder that affects the immune system’s ability to fight off certain types of bacteria and fungi. This condition is characterized by the formation of granulomas, which are clusters of immune cells that form in various parts of the body, attempting to wall off the infections. CGD is caused by mutations in the genes responsible for producing certain proteins necessary for the immune cells, known as phagocytes, to produce reactive oxygen species that kill invading pathogens.
Causes of CGD
CGD is primarily caused by genetic mutations that are inherited from one’s parents. These mutations affect the genes responsible for the production of components of the NADPH oxidase enzyme complex. This enzyme plays a crucial role in the immune system’s ability to generate reactive oxygen species that kill bacteria and fungi. Depending on the specific gene mutation, CGD can be inherited in an X-linked recessive manner, which is more common and affects mainly males, or an autosomal recessive manner, affecting both males and females equally.
Symptoms and How They Manifest
The symptoms of CGD can vary widely among affected individuals but typically manifest in recurrent infections that are difficult to treat. These infections can affect various parts of the body, including the lungs, skin, lymph nodes, liver, and bones. Common symptoms include:
- Persistent and recurrent bacterial and fungal infections
- Formation of granulomas, which can lead to obstruction and dysfunction of affected organs
- Swollen lymph nodes
- Fever and chills
- Skin rashes and abscesses
- Gastrointestinal issues, such as diarrhea and abdominal pain
These symptoms usually appear in childhood, but the severity and frequency of infections can vary.
Statistics: Prevalence and Demographics
CGD is a rare condition, with an estimated prevalence of approximately 1 in 200,000 to 250,000 individuals worldwide. However, the prevalence can vary by region and population. The X-linked form of CGD is more common, accounting for about 65-70% of cases, making the disease more prevalent in males. However, the autosomal recessive form affects both genders equally. CGD can occur in any ethnic group, but the distribution of specific gene mutations may vary among different populations.
Understanding CGD is crucial for early diagnosis and treatment, which can significantly improve the quality of life for those affected. Advances in medical research and treatment strategies continue to offer hope for individuals with CGD and their families.
Diagnosis of Chronic Granulomatous Disease
Early and accurate diagnosis is crucial for managing the condition effectively. This article provides a comprehensive overview of the diagnostic process for CGD, highlighting the importance of initial screening, symptom recognition, diagnostic tests, and the challenges faced during diagnosis.
Initial Screening and Symptom Recognition
The journey to diagnosing CGD often begins with the recognition of recurring infections that are unusually severe or caused by specific organisms. Patients, especially children, may experience frequent bouts of pneumonia, skin infections, abscesses, and other infections that do not respond well to standard treatments. Early detection through careful observation of these symptoms can prompt further investigation.
Diagnostic Tests for CGD
Several specialized tests are used to confirm a diagnosis of CGD. These tests assess the function of neutrophils, a type of white blood cell essential for combating infections.
Nitroblue Tetrazolium (NBT) Test
The NBT test is a traditional method used to screen for CGD. It measures the ability of neutrophils to produce reactive oxygen species (ROS), which are crucial for killing bacteria and fungi. In this test, a yellow dye (NBT) turns blue when it is exposed to ROS. Neutrophils from individuals with CGD fail to change the color of the dye, indicating a dysfunction in ROS production.
Dihydrorhodamine (DHR) Flow Cytometry Test
The DHR test is a more sensitive and specific test compared to the NBT test. It uses flow cytometry to measure the oxidative burst, or the production of ROS, by neutrophils. Patients with CGD show a reduced or absent oxidative burst, confirming the diagnosis. Due to its accuracy, the DHR test has become the preferred diagnostic test for CGD.
Genetic Testing for Identifying Mutations
Genetic testing plays a critical role in diagnosing CGD by identifying mutations in the genes responsible for the production of the components necessary for the neutrophils’ bactericidal activity. Identifying the specific genetic mutation helps in understanding the disease’s severity and can guide treatment options. It is also invaluable for family planning and prenatal diagnosis.
The Role of Medical History and Physical Examination
A thorough medical history and physical examination complement the diagnostic tests. A history of recurrent or severe infections, especially if there is a family history of similar issues, can indicate CGD. Physical examination may reveal signs of current or past infections, including swollen lymph nodes, skin lesions, or organomegaly.
Challenges in Diagnosing CGD
Diagnosing CGD poses several challenges. The rarity of the disease and the nonspecific nature of its symptoms can lead to misdiagnosis or delayed diagnosis. Moreover, the complexity of the diagnostic tests requires specialized equipment and expertise, which may not be readily available in all healthcare settings. Awareness and education among healthcare providers about CGD and its presenting symptoms are crucial for improving diagnosis rates.
However, diagnosing Chronic Granulomatous Disease involves a multifaceted approach that includes initial symptom recognition, specialized diagnostic tests, and a thorough medical history and physical examination. Despite the challenges, early and accurate diagnosis is essential for effective management and treatment of CGD, improving the quality of life for those affected.
Treatment Options for Chronic Granulomatous Disease
Patients with CGD are more susceptible to bacteria and fungi, leading to frequent and sometimes severe infections. Fortunately, advances in medical science have led to various effective treatment options. This article explores the treatment goals and strategies for managing CGD, focusing on antibiotics and antifungal medications, Interferon-gamma (IFN-γ) therapy, Hematopoietic stem cell transplantation (HSCT), gene therapy, managing complications, and the importance of a multidisciplinary approach.
Overview of Treatment Goals and Strategies
The primary goal in treating CGD is to prevent infections, manage complications, and improve the quality of life for patients. Treatment strategies are tailored to each patient’s needs and may include a combination of medications, therapies, and in some cases, surgery to address specific complications.
Antibiotics and Antifungal Medications: Preventing Infections
A cornerstone of managing CGD is the prevention of infections through the use of prophylactic (preventive) antibiotics and antifungal medications. These drugs are used to protect patients from the bacteria and fungi they are particularly vulnerable to. The choice of medication depends on the patient’s specific susceptibility and the types of infections they are most at risk for.
Interferon-gamma (IFN-γ) Therapy: Enhancing Immune Function
Interferon-gamma (IFN-γ) therapy is another critical component of treatment for CGD. IFN-γ is a cytokine that plays a significant role in activating the immune system. Regular injections of IFN-γ can help boost the immune response, reducing the frequency and severity of infections in CGD patients.
Hematopoietic Stem Cell Transplantation (HSCT): Potential Cure
Hematopoietic stem cell transplantation (HSCT) offers a potential cure for CGD by replacing the defective immune cells with healthy ones from a compatible donor. This procedure carries significant risks, including the risk of graft-versus-host disease (GVHD), but it can be life-changing for patients who have a suitable donor and respond well to the treatment.
Gene Therapy: Emerging Treatments and Research
Gene therapy represents an exciting frontier in the treatment of CGD. By correcting the genetic defect that causes CGD, gene therapy has the potential to offer a long-term cure. While still in the experimental stages, early results from clinical trials are promising, offering hope for a future where CGD can be effectively cured with minimal side effects.
Managing Complications and Associated Conditions
Managing the complications of CGD, such as inflammatory conditions, requires a tailored approach. This may include medications to control inflammation, surgery to address obstructions or abscesses, and treatments for associated conditions like autoimmune disorders.
The Importance of a Multidisciplinary Approach
Effective management of CGD requires a multidisciplinary approach, involving specialists from immunology, infectious diseases, hematology, and other fields. A team of healthcare professionals can provide comprehensive care, addressing not only the medical but also the psychological and social needs of CGD patients and their families.
However, while CGD poses significant challenges, the availability of various treatment options offers hope for effective management and improved outcomes. Advances in medical research continue to provide new insights into potential cures, making the future brighter for those affected by this condition.
Living with Chronic Granulomatous Disease
Living with Chronic Granulomatous Disease (CGD) presents unique challenges that require careful management, lifestyle adjustments, and a robust support system to maintain a high quality of life. CGD is a rare immune disorder that affects the body’s ability to fight off certain infections, making preventive care and daily management crucial for those diagnosed with the condition. In this article, we explore the lifestyle adjustments, preventive care strategies, and support systems essential for navigating the challenges of CGD, as well as the impact of the disease on quality of life and mental health.
Lifestyle Adjustments and Preventive Care
For individuals living with CGD, making specific lifestyle adjustments can significantly reduce the risk of infections and improve overall well-being. These adjustments often include:
- Hygiene Practices: Implementing meticulous hygiene practices is crucial. Regular handwashing, avoiding exposure to known pathogens, and maintaining a clean living environment can help prevent infections.
- Diet and Nutrition: A balanced diet rich in vitamins and minerals supports the immune system. Some individuals may also require dietary adjustments to avoid certain foods that could pose a risk of infection.
- Regular Exercise: Engaging in moderate exercise can strengthen the body and enhance immune function. However, it’s important to consult with a healthcare provider to tailor an exercise plan that considers individual health status.
Preventive care is equally important and typically involves regular medical check-ups, vaccinations (as recommended by healthcare providers), and prompt treatment of infections. Prophylactic antibiotics or antifungal medications may be prescribed to prevent infections before they occur.
Support Systems: Navigating Challenges with Professional and Community Support
The complexity of CGD means that professional healthcare support is vital. This support can come from a multidisciplinary team of doctors, nurses, and other specialists who understand CGD and can offer comprehensive care, including medical treatment, psychological support, and guidance on lifestyle management.
Community support also plays a critical role in navigating the challenges of CGD. Support groups, either online or in-person, can provide a platform for sharing experiences, advice, and emotional support. Connecting with others who understand the lived experience of CGD can be incredibly validating and empowering.
The Impact on Quality of Life and Mental Health
Living with CGD can have a significant impact on quality of life and mental health. The constant vigilance against infections, frequent medical appointments, and potential social isolation can be stressful and may lead to anxiety or depression. Acknowledging and addressing the psychological impact of CGD is essential. Counseling or therapy, along with strong social support, can help individuals cope with the emotional challenges posed by the disease.
Moreover, fostering a positive outlook, focusing on what can be controlled, and engaging in activities that bring joy and satisfaction can enhance quality of life. It’s important for individuals with CGD and their families to seek out resources and support that can help them live full and rewarding lives despite the challenges of the disease.
However, living with Chronic Granulomatous Disease requires careful management, but with the right lifestyle adjustments, preventive care, and support systems, individuals can lead healthy and fulfilling lives. Recognizing the impact of CGD on mental health and quality of life is crucial, and support from healthcare professionals, alongside a strong community network, can provide the resilience and coping strategies needed to navigate the journey with CGD.
Recent Advances and Research in Chronic Granulomatous Disease Treatment
Recent years have witnessed significant strides in the understanding and treatment of CGD, paving the way for more effective management strategies and improved patient outcomes. This section delves into the latest findings and ongoing clinical trials in CGD treatment, along with exploring the future directions in therapy and management.
Summary of the Latest Findings and Ongoing Clinical Trials
Recent advances in the treatment of CGD have been largely driven by a deeper understanding of the disease’s genetic and molecular underpinnings. Gene therapy has emerged as a promising avenue, with several studies demonstrating its potential to correct the genetic defects causing CGD. For instance, clinical trials utilizing lentiviral vectors to introduce functional copies of the gene affected in CGD patients have shown encouraging results, including sustained restoration of immune function in treated individuals.
Another area of active research is the development of new antimicrobial and immunomodulatory therapies. These treatments aim to enhance the body’s ability to fight infections and reduce inflammation, thereby mitigating the symptoms of CGD. For example, the use of interferon-gamma has been shown to significantly reduce the frequency of infections in CGD patients by boosting their immune response.
Ongoing clinical trials are exploring the efficacy of stem cell transplantation, with a focus on reducing the procedure’s risks and improving its success rates. Advances in donor matching and conditioning regimens have already resulted in better outcomes for patients undergoing this potentially curative treatment.
Future Directions in Therapy and Management
Looking ahead, the field of CGD treatment is poised for transformative changes, with several key areas of focus. One of the most anticipated developments is the refinement of gene therapy techniques. Researchers are working on enhancing the safety and efficiency of gene transfer methods, which could make gene therapy a mainstream treatment option for CGD in the near future.
Another promising area is the application of precision medicine in CGD management. By tailoring treatment strategies to the specific genetic and immunological profile of each patient, healthcare providers can optimize outcomes and minimize side effects. This personalized approach could also include the use of novel biologic agents designed to target specific pathways involved in the disease process.
Additionally, there is an increasing interest in developing strategies to prevent the complications of CGD, such as chronic inflammation and autoimmune disorders. This could involve the use of advanced immunomodulatory therapies and lifestyle interventions aimed at maintaining immune balance and promoting overall health.
However, the landscape of CGD treatment is rapidly evolving, with ongoing research and clinical trials offering hope for more effective and personalized therapies. As we continue to unravel the complexities of this condition, the future holds the promise of not only extending the lives of CGD patients but also significantly enhancing their quality of life.
Conclusion
Personalized treatment plans are paramount in the care of individuals with CGD. Given the variability in how CGD presents and progresses among patients, treatments must be tailored to meet each individual’s specific needs. Advances in medical research have led to a variety of treatment options, including antibiotics, antifungals, gene therapy, and bone marrow transplantation. These treatments, when customized to the patient’s unique situation, offer the best chance for managing symptoms and improving outcomes.
Moreover, the journey towards a cure for CGD is ongoing, and continued research is essential. The development of new and innovative treatments depends on the dedication of scientists and the support of funding bodies. It’s crucial that we maintain momentum in research efforts to uncover breakthroughs that can lead to more effective and less invasive treatment options.
Finally, the support for patients dealing with CGD and their families cannot be overstated. Living with a chronic condition is challenging, and having access to a supportive community and resources can make a significant difference in the lives of those affected. Patient advocacy groups, online communities, and healthcare providers play a vital role in offering the necessary support and information.
In conclusion, our understanding of Chronic Granulomatous Disease has come a long way, but there is still much to learn. Early detection, personalized treatment plans, ongoing research, and patient support are the cornerstones of improving care and outcomes for individuals with CGD. As we continue to advance in our knowledge and treatment approaches, there is hope for a future where CGD can be managed more effectively, or perhaps, even cured. Let’s remain committed to supporting research, providing comprehensive care, and fostering a supportive community for those affected by CGD.