Cholecystitis Symptoms: Cholecystitis, an inflammation of the gallbladder, is a condition that requires immediate attention due to its potential to cause significant discomfort and complications.
This comprehensive guide aims to delve deep into the symptoms and causes of cholecystitis, providing readers with essential information to understand, recognize, and seek appropriate treatment for this medical condition.
What is Cholecystitis?
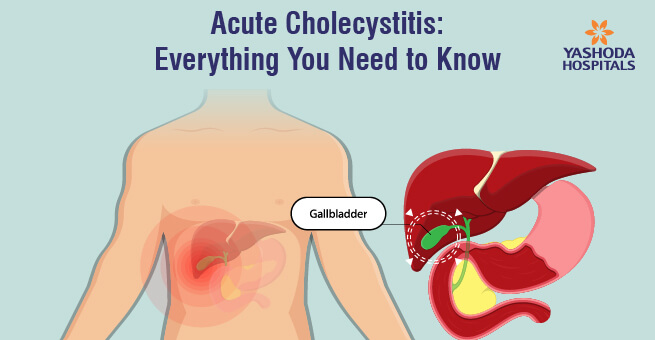
Cholecystitis is an inflammation of the gallbladder, a small, pear-shaped organ located under the liver. The gallbladder plays a crucial role in the digestive system by storing bile, a fluid produced by the liver to digest fats. When the flow of bile is blocked, it can lead to cholecystitis, causing severe pain, infection, and other serious complications.
The Gallbladder’s Role in the Digestive System
The gallbladder serves as a storage reservoir for bile, which is essential for the digestion and absorption of fats and fat-soluble vitamins in the small intestine. Bile helps in breaking down fats into fatty acids, which can be easily absorbed by the digestive tract. After a meal, the gallbladder contracts and releases stored bile into the small intestine through the bile ducts. This process ensures efficient digestion and nutrient absorption, highlighting the gallbladder’s vital role in maintaining digestive health.
Different Types of Cholecystitis
Cholecystitis can be classified into two main types: acute and chronic, each with distinct characteristics and implications for health.
- Acute Cholecystitis: This type occurs suddenly, often due to a gallstone blocking the cystic duct, which leads to inflammation and infection. Symptoms include severe pain in the upper right abdomen, fever, nausea, and vomiting. Acute cholecystitis is a medical emergency that requires prompt treatment to prevent complications such as gallbladder rupture.
- Chronic Cholecystitis: Chronic cholecystitis is the result of repeated episodes of acute cholecystitis or long-term inflammation of the gallbladder. It is characterized by less severe, but more persistent, symptoms that may gradually worsen over time. Chronic cholecystitis can lead to a thickening and hardening of the gallbladder walls, decreased gallbladder function, and sometimes, the formation of gallstones.
Understanding the distinctions between acute and chronic cholecystitis is crucial for diagnosis and treatment. While both conditions share similar symptoms, their management strategies differ significantly, emphasizing the importance of early detection and appropriate medical intervention.
Symptoms of Cholecystitis: Understanding the Warning Signs
Recognizing these symptoms early can lead to timely diagnosis and treatment, preventing complications. This article outlines the primary and secondary symptoms of cholecystitis and explains how these symptoms differ between acute and chronic forms of the condition.
Primary Symptoms Associated with Cholecystitis
The onset of cholecystitis is often marked by intense pain in the upper right abdomen, which can radiate to the back or right shoulder blade. This pain typically escalates rapidly and can become constant. Key primary symptoms include:
- Severe abdominal pain: Particularly in the upper right quadrant, which may intensify within minutes to hours.
- Fever: A moderate to high fever, often accompanied by chills, indicates an infection within the gallbladder.
- Nausea and vomiting: These are common reactions to the intense pain and the body’s attempt to alleviate irritation and inflammation.
These symptoms can be triggered by fatty meals, which stimulate the gallbladder to release bile, exacerbating the inflammation and discomfort.
Secondary Symptoms and Their Implications
As cholecystitis progresses, secondary symptoms may emerge, highlighting the severity of the condition and its impact on the body. These include:
- Jaundice: A yellowing of the skin and eyes, suggesting that the inflammation has affected bile flow.
- Changes in stool and urine color: Light-colored stools and dark urine indicate a bile duct blockage.
- Tenderness in the abdomen upon touching: This suggests an inflamed gallbladder.
These secondary symptoms often require immediate medical attention, as they suggest complications that could extend beyond the gallbladder itself.
How Symptoms Differ Between Acute and Chronic Cholecystitis
The distinction between acute and chronic cholecystitis lies in the duration and intensity of symptoms.
- Acute Cholecystitis: Symptoms appear suddenly and are typically severe. Acute cholecystitis may lead to complications such as gallbladder rupture if not treated promptly. The pain is sharp and may be accompanied by fever, nausea, and vomiting.
- Chronic Cholecystitis: This form develops over time, with symptoms less intense but more persistent. Individuals may experience recurrent episodes of discomfort, particularly after meals. Chronic cases often result from repeated episodes of acute cholecystitis or continuous gallstone irritation.
Understanding these differences is crucial for diagnosis and treatment, emphasizing the importance of medical evaluation when symptoms first appear.
Whether acute or chronic, cholecystitis requires medical attention to prevent further health complications. If you experience any of the symptoms described, consult a healthcare provider for an accurate diagnosis and appropriate treatment.
Causes of Cholecystitis
Understanding the causes of this condition is crucial for both prevention and treatment. The primary cause of cholecystitis is gallstones, but several other factors can also lead to its development. This article delves into the various causes of cholecystitis, including gallstones, gallbladder sludge, tumors, bile duct blockage, and identifies risk factors contributing to its occurrence.
Gallstones as the Primary Cause
Gallstones are the most common cause of cholecystitis. These hard particles form from cholesterol and bilirubin in the gallbladder and can block the flow of bile, leading to inflammation. When the bile duct is blocked, the bile becomes trapped, causing the gallbladder to swell and potentially get infected. This condition, known as acute cholecystitis, requires immediate medical attention.
Other Causes Leading to Cholecystitis
While gallstones account for the majority of cholecystitis cases, other conditions can also lead to the inflammation of the gallbladder.
- Gallbladder Sludge: Also known as biliary sludge, it is a mixture of particulate matter and mucus that can accumulate in the gallbladder. It may lead to gallstones or cholecystitis directly if it blocks the bile ducts.
- Tumors: Tumors in the gallbladder or bile ducts can obstruct the flow of bile, causing cholecystitis. Although less common, these need to be identified early for appropriate treatment.
- Bile Duct Blockage: Apart from gallstones, other blockages in the bile ducts, such as scars from previous injuries, can prevent bile from draining and lead to cholecystitis.
Risk Factors Contributing to the Development of Cholecystitis
Certain factors can increase the risk of developing cholecystitis:
- Age and Gender: Women, especially those over 40, are more likely to develop gallstones and, consequently, cholecystitis.
- Obesity: Excess body weight increases the risk of gallstones.
- Diet: A diet high in fat and cholesterol and low in fiber can contribute to the formation of gallstones.
- Rapid Weight Loss: Losing weight very quickly can lead to the formation of gallstones.
- Other Health Conditions: Diabetes, liver disease, and certain blood disorders can increase the risk of gallstones.
Keeping a healthy lifestyle, managing weight, and eating a balanced diet can also help reduce the risk of developing this painful condition.
Diagnosing Cholecystitis
Early diagnosis is crucial to manage symptoms and prevent severe complications. In this section, we explore the common diagnostic tests and procedures for cholecystitis and underscore the importance of early diagnosis.
Common Diagnostic Tests and Procedures
- Blood Tests: Initial tests often include a complete blood count (CBC) to check for signs of infection or inflammation in the body. Liver function tests (LFTs) can assess the health of the liver and gallbladder.
- Ultrasound: A primary tool for diagnosing cholecystitis, an abdominal ultrasound can visualize gallstones, gallbladder inflammation, and bile duct issues, which are common causes of the condition.
- Hepatobiliary Iminodiacetic Acid (HIDA) Scan: This nuclear imaging test evaluates how well the gallbladder functions and is highly effective in diagnosing acute cholecystitis when ultrasound results are inconclusive.
- Computed Tomography (CT) Scan: A CT scan can provide detailed images of the gallbladder and surrounding structures, helping to identify inflammation, gallstones, or complications of cholecystitis.
- Magnetic Resonance Imaging (MRI): MRI scans can offer comprehensive details about the bile ducts and gallbladder, particularly useful in diagnosing complications or for planning surgical interventions.
Importance of Early Diagnosis
Early diagnosis of cholecystitis is paramount for several reasons:
- Preventing Complications: Untreated cholecystitis can lead to serious complications such as gallbladder rupture, abscess formation, and sepsis. Early detection allows for timely intervention to avoid these outcomes.
- Managing Pain and Symptoms: Early diagnosis enables the implementation of effective pain management strategies and treatments to alleviate symptoms, improving the patient’s quality of life.
- Guiding Treatment Decisions: Identifying cholecystitis early helps in deciding the most appropriate treatment course—whether it be conservative management, medication, or surgery.
- Reducing Healthcare Costs: By preventing complications and guiding effective treatment strategies, early diagnosis can significantly reduce healthcare costs associated with advanced cholecystitis and its management.
However, employing the right diagnostic tests and procedures for cholecystitis is crucial for an accurate diagnosis. Early detection plays a pivotal role in managing the condition effectively, preventing complications, and ensuring a better outcome for the patient. Healthcare providers and patients alike should be vigilant for symptoms of cholecystitis and seek medical evaluation promptly to facilitate early diagnosis and treatment.
Treatment Options for Cholecystitis
There are several treatment options available, ranging from initial home management to medical and surgical interventions, as well as lifestyle and diet adjustments post-diagnosis. Here’s a closer look at the various ways to manage and treat cholecystitis effectively.
Initial Treatments: Managing Symptoms at Home
In the early stages of cholecystitis, or for mild cases, symptoms can often be managed at home. This includes applying heat to the abdomen to reduce pain, staying hydrated, and avoiding fatty foods that can exacerbate symptoms. While these measures can provide temporary relief, it’s important to consult a healthcare professional for a proper diagnosis and to discuss long-term treatment options.
Medical Treatments: Antibiotics and Pain Management
For cases of cholecystitis caused by bacterial infection, antibiotics are a key component of treatment to eliminate the infection. Pain management is also critical, and doctors may prescribe medications to alleviate discomfort. It’s essential to follow your healthcare provider’s instructions closely when taking these medications to ensure effectiveness and reduce the risk of complications.
Surgical Options: Cholecystectomy and Its Types
When medical treatments are not sufficient to resolve cholecystitis, or in cases of severe or recurrent inflammation, surgery may be necessary. The most common surgical procedure for cholecystitis is a cholecystectomy, which is the removal of the gallbladder. There are two types of cholecystectomy:
- Laparoscopic Cholecystectomy: A minimally invasive surgery where small incisions are made, and a camera and surgical tools are inserted to remove the gallbladder. This method is preferred due to its shorter recovery time and less postoperative pain.
- Open Cholecystectomy: A more invasive procedure requiring a larger abdominal incision. This method may be necessary in complicated cases or when laparoscopic surgery is not feasible.
Lifestyle and Diet Adjustments Post-Diagnosis
After treatment for cholecystitis, making lifestyle and diet adjustments is crucial to prevent future issues and promote overall health. This includes eating a well-balanced, low-fat diet, maintaining a healthy weight, and engaging in regular physical activity. Avoiding foods high in saturated fats and choosing foods rich in fiber can also help support a healthy digestive system.
By understanding and exploring these treatment options for cholecystitis, individuals can work with their healthcare providers to find the most effective strategies for managing and overcoming this condition. Remember, early intervention and adherence to recommended treatments are key to preventing complications and ensuring a swift recovery.
Preventing Cholecystitis: Effective Strategies to Reduce Risk
There are proactive steps you can take to minimize your risk of developing gallstones and cholecystitis. Adhering to a healthy lifestyle, focusing on dietary habits, and understanding the importance of regular medical check-ups are key measures in preventing this condition.
Adopt a Healthy Diet
One of the most effective ways to prevent gallstones and subsequently cholecystitis is through a balanced and healthy diet. A diet rich in fruits, vegetables, whole grains, and healthy fats can reduce the risk of gallstones by ensuring proper digestion and reducing cholesterol levels in the bile, which is a common contributor to gallstone formation. It’s also advisable to:
- Limit saturated fats and cholesterol: High-fat diets can increase cholesterol in the bile, leading to gallstone formation. Opt for lean protein sources and incorporate healthy fats like those from avocados, nuts, and olive oil.
- Increase fiber intake: Foods high in fiber, such as legumes, whole grains, and a variety of fruits and vegetables, can help maintain a healthy weight and reduce the risk of gallstones.
- Stay hydrated: Drinking plenty of water throughout the day helps keep the bile in your gallbladder fluid, making it less likely to form stones.
Maintain a Healthy Weight
Obesity and rapid weight loss are significant risk factors for the development of gallstones. Maintaining a healthy weight through a balanced diet and regular exercise is crucial in preventing cholecystitis. If weight loss is necessary, aim for a gradual reduction in weight, as rapid weight loss can increase the risk of gallstones by causing the liver to release extra cholesterol into the bile.
Importance of Regular Medical Check-ups
Regular medical check-ups play a vital role in preventing cholecystitis by early detection and management of risk factors for gallstones. During these check-ups, healthcare professionals can monitor your weight, diet, and overall health, providing guidance on preventive measures tailored to your specific health needs. They can also perform necessary screenings to detect any early signs of gallstone formation, allowing for timely intervention before complications arise.
In addition to these lifestyle and dietary modifications, it’s essential to:
- Avoid crash diets and fasting: These can lead to a concentration of bile that promotes gallstone formation.
- Manage blood sugar levels: For individuals with diabetes or insulin resistance, managing blood sugar levels can help prevent the development of gallstones.
Implementing these strategies can significantly reduce the risk of developing gallstones and cholecystitis. Adopting a healthy lifestyle, being mindful of dietary choices, and ensuring regular medical check-ups are key steps towards maintaining a healthy gallbladder and preventing the painful and potentially serious complications associated with cholecystitis.
FAQ Section: Understanding Cholecystitis Symptoms and Causes
What is cholecystitis?
Cholecystitis is an inflammation of the gallbladder, a small, pear-shaped organ located under the liver. The gallbladder stores bile, a fluid produced by the liver to digest fats. When the flow of bile is blocked, it can lead to inflammation and infection, resulting in cholecystitis.
What causes cholecystitis?
The most common cause of cholecystitis is gallstones. Gallstones are hard particles that form from cholesterol or bilirubin in the bile and can block the ducts leading out of the gallbladder, causing inflammation. Other causes include bile duct problems, tumors, serious illness, and infection.
What are the symptoms of cholecystitis?
Symptoms of cholecystitis can vary but often include:
- Severe pain in the upper right or center abdomen, which may extend to the back or right shoulder
- Fever
- Nausea and vomiting
- Tenderness over the abdomen when touched
- Jaundice (yellowing of the skin and eyes) The pain associated with cholecystitis may intensify after eating a fatty meal.
How is cholecystitis diagnosed?
Cholecystitis is typically diagnosed through a combination of physical examination, medical history, and imaging tests. Common diagnostic tools include ultrasound, which can detect gallstones, and other imaging tests like CT scans or HIDA scans to evaluate the gallbladder’s function and look for inflammation.
Can cholecystitis be prevented?
While not all cases of cholecystitis can be prevented, reducing the risk of gallstones can help. This includes maintaining a healthy weight, eating a balanced diet rich in fiber and low in cholesterol and fats, and staying active. It’s also important to manage underlying health conditions that may increase the risk of gallstones.
What treatments are available for cholecystitis?
Treatment for cholecystitis often involves managing the symptoms and treating the infection. In mild cases, this may include fasting, fluid replacement, and antibiotics. For severe cases or recurrent cholecystitis, surgery to remove the gallbladder (cholecystectomy) may be necessary. Pain management is also an important aspect of treatment.
Conclusion:
In wrapping up our discussion, it’s crucial to underscore the significance of recognizing the symptoms of cholecystitis and understanding its underlying causes. Cholecystitis, an inflammation of the gallbladder, can lead to severe complications if not promptly addressed. Symptoms such as intense abdominal pain, fever, and nausea should not be overlooked, as they are indicative of this condition.
Understanding the causes of cholecystitis, including gallstones, bacterial infections, and other factors, empowers us to take proactive steps towards prevention and early detection. Awareness of these causes is the first line of defense against the progression of this potentially life-threatening condition.
We strongly encourage anyone who suspects they may be experiencing symptoms of cholecystitis to seek medical advice without delay. Timely consultation with a healthcare professional is essential for accurate diagnosis and appropriate treatment. Remember, prioritizing your health is not just about addressing current issues but also about preventing future complications.
Let this be a reminder of the importance of listening to our bodies and taking action when something feels amiss. By staying informed and vigilant, we can better navigate the complexities of our health and ensure a prompt response to conditions like cholecystitis. Your health is invaluable—never hesitate to seek the guidance and support of medical professionals when you need it.