Cholangiocarcinoma Treatment: Cholangiocarcinoma, known as bile duct cancer, is a rare and aggressive form of cancer that arises from the cells lining the bile ducts. These ducts are essential for transporting bile, a fluid made by the liver to help digest fats.
Due to its complexity and rarity, diagnosing and treating cholangiocarcinoma requires a comprehensive approach.
What is Cholangiocarcinoma?
Cholangiocarcinoma, often referred to as bile duct cancer, is a rare but aggressive form of cancer that originates in the bile ducts. These ducts are critical pathways that carry bile, a fluid produced by the liver to aid in digestion, from the liver to the gallbladder and small intestine. Due to its complex nature and the vital functions of the bile ducts, cholangiocarcinoma presents significant health challenges and requires early diagnosis and comprehensive treatment.
Types of Cholangiocarcinoma
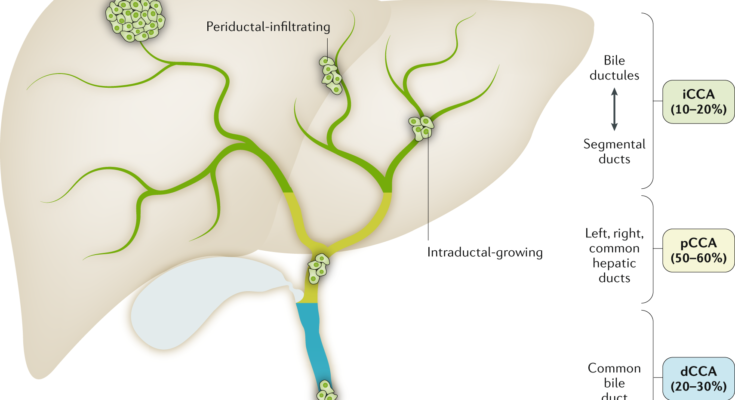
Cholangiocarcinoma is classified based on its location in the bile duct system:
1. Intrahepatic Cholangiocarcinoma: This type occurs within the liver’s bile ducts. It’s less common but tends to be diagnosed at an advanced stage due to the lack of specific symptoms in its early stages.
2. Extrahepatic Cholangiocarcinoma: This category includes cancers that develop outside the liver. It’s further divided into:
- Perihilar Cholangiocarcinoma, also known as Klatskin tumor, occurs at the junction where the left and right bile ducts meet outside the liver.
- Distal Cholangiocarcinoma develops further down the bile duct, closer to the small intestine.
Understanding the type of cholangiocarcinoma is crucial for determining the most effective treatment approach.
Causes and Risk Factors
While the exact cause of cholangiocarcinoma is not fully understood, several factors have been identified that may increase the risk of developing this cancer. These include:
- Primary Sclerosing Cholangitis (PSC): A chronic liver disease that causes scarring and narrowing of bile ducts.
- Chronic Liver Disease: Conditions such as hepatitis B and C, cirrhosis, and fatty liver disease can elevate the risk.
- Infections: Parasitic infections, particularly with liver flukes which are more common in certain parts of Asia, can lead to cholangiocarcinoma.
- Bile Duct Abnormalities: Congenital abnormalities in the bile ducts, such as choledochal cysts, are associated with a higher risk.
- Lifestyle Factors: Obesity and smoking may also contribute to the risk of developing bile duct cancer.
Statistics and Prevalence
Cholangiocarcinoma is considered a rare disease, with varying incidence rates globally. The prevalence is higher in regions where liver fluke infections are endemic, such as Southeast Asia. According to recent statistics, the incidence of cholangiocarcinoma in the United States is approximately 1 to 2 cases per 100,000 people annually. However, rates appear to be rising globally, possibly due to improved diagnostic methods and increased awareness of the disease.
Despite its rarity, cholangiocarcinoma poses significant challenges due to its aggressive nature and the complexity of treatment. Early detection and understanding of risk factors are key components in managing this disease effectively.
Symptoms and Early Detection of Cholangiocarcinoma
Recognizing the common symptoms and understanding the importance of early detection are crucial steps toward a timely diagnosis and effective treatment. In this section, we will explore the common symptoms of Cholangiocarcinoma, the significance of identifying early signs, and the screening and diagnostic tests available for this condition.
Common Symptoms of Cholangiocarcinoma
The symptoms of Cholangiocarcinoma often appear in the disease’s advanced stages, making early detection difficult. However, some early signs may include:
- Jaundice: A yellowing of the skin and eyes resulting from the buildup of bilirubin, a byproduct of old red blood cells.
- Itching: Severe itching is a common symptom due to the accumulation of bile salts in the skin.
- Abdominal Pain: Pain in the upper right abdomen, sometimes extending to the back or shoulder, can occur.
- Weight Loss and Fatigue: Unintended weight loss and a general feeling of fatigue or weakness.
- Dark Urine and Pale Stools: Changes in urine and stool color due to bile duct blockage.
Importance of Recognizing Early Signs for Timely Diagnosis
Identifying the early signs of Cholangiocarcinoma can significantly improve the prognosis and effectiveness of treatment. Early detection allows for a broader range of treatment options, including surgery, which can be curative. It also reduces the risk of complications associated with advanced disease stages. Awareness of the symptoms and seeking medical advice promptly when they appear are vital steps in achieving an early diagnosis.
Screening and Diagnostic Tests
For individuals at risk of Cholangiocarcinoma or those presenting with symptoms, various screening and diagnostic tests are essential for confirming the diagnosis:
1. Blood Tests: Tests such as liver function tests (LFTs) can indicate abnormalities in the liver, although they are not specific to Cholangiocarcinoma. Tumor markers like CA 19-9 may also be elevated in some patients with bile duct cancer.
2. Imaging Tests:
- Magnetic Resonance Imaging (MRI): Provides detailed images of the bile ducts and surrounding structures.
- Computed Tomography (CT) Scan: Offers cross-sectional images of the abdomen, helping to identify the tumor’s location and size.
- Ultrasound: A non-invasive test that uses sound waves to produce images of the liver and bile ducts.
3. Biopsy and Pathology: The definitive diagnosis of Cholangiocarcinoma is made by examining tissue samples under a microscope. A biopsy can be obtained through techniques such as endoscopic retrograde cholangiopancreatography (ERCP) or percutaneous needle biopsy, guided by imaging tests.
Early detection of Cholangiocarcinoma remains a challenge but is crucial for improving patient outcomes. Understanding the symptoms and the importance of timely diagnosis, coupled with the appropriate use of screening and diagnostic tests, can lead to more effective management and treatment of this rare but serious cancer.
Diagnosis of Cholangiocarcinoma: A Comprehensive Guide
With advancements in medical imaging and endoscopic techniques, early and accurate diagnosis is becoming increasingly feasible. This guide delves into the detailed process of diagnosing cholangiocarcinoma, highlighting the role of advanced imaging, endoscopic methods, and the importance of staging in treatment planning.
Detailed Process of Diagnosing Bile Duct Cancer
The diagnosis of cholangiocarcinoma typically begins with a thorough medical history and physical examination, followed by a series of tests to confirm the presence of the tumor and assess its extent. Symptoms such as jaundice, itching, weight loss, and abdominal pain may prompt further investigation.
Role of Advanced Imaging and Endoscopic Techniques
Advanced imaging and endoscopic techniques play a pivotal role in diagnosing cholangiocarcinoma. These methods not only help in detecting the tumor but also in determining its location, size, and whether it has spread to nearby tissues or organs.
ERCP (Endoscopic Retrograde Cholangiopancreatography)
ERCP is a crucial endoscopic technique used in the diagnosis and sometimes treatment of conditions affecting the bile ducts and pancreas. During ERCP, a flexible tube with a camera on the end (endoscope) is inserted through the mouth, passing through the stomach and into the small intestine. A dye is then injected into the bile and pancreatic ducts, and X-rays are taken to visualize blockages or abnormalities. This procedure can also allow for the collection of tissue samples (biopsy) for further analysis.
MRCP (Magnetic Resonance Cholangiopancreatography)
MRCP is a non-invasive imaging technique that uses magnetic resonance imaging (MRI) to produce detailed images of the bile ducts, pancreatic duct, and liver. Unlike ERCP, MRCP does not require the insertion of an endoscope or dye injection. It is particularly useful for visualizing the bile ducts’ structure and identifying obstructions, tumors, or other abnormalities.
Staging of Cholangiocarcinoma and Its Importance in Treatment Planning
Staging is a critical step in the management of cholangiocarcinoma, as it determines the extent of the disease and guides the selection of the most appropriate treatment options. The staging process involves evaluating the size of the tumor, the degree of invasion into surrounding tissues, and whether the cancer has spread to nearby lymph nodes or distant organs (metastasis).
The stage of cholangiocarcinoma significantly influences treatment decisions. Early-stage cancers may be candidates for surgical removal, offering the best chance for a cure. In contrast, advanced stages may require a combination of therapies, including chemotherapy, radiation therapy, and palliative care to manage symptoms and improve quality of life.
However, the diagnosis of cholangiocarcinoma is a complex process that requires a combination of clinical evaluation, advanced imaging, and endoscopic techniques. Understanding the role of these diagnostic tools and the importance of accurate staging is essential for developing an effective treatment plan tailored to the individual patient’s needs. As research advances, it is hoped that earlier detection and more precise treatments will become available, improving outcomes for patients with this challenging disease.
Cholangiocarcinoma Treatment Options
The treatment approach for Cholangiocarcinoma varies depending on the stage of the cancer, its location, and the overall health of the patient. Treatment modalities can be broadly categorized into surgical and non-surgical options, each with its criteria, benefits, and considerations.
Surgical Treatments and Their Criteria
Resection for Early-Stage Cancer: Surgical removal of the tumor, known as resection, is often considered the most effective treatment for early-stage Cholangiocarcinoma. The feasibility of resection depends on the tumor’s size, location, and whether it has spread to surrounding tissues or organs. A successful resection aims to remove all cancerous cells, potentially offering a cure.
Liver Transplant Considerations: For certain patients, especially those with unresectable tumors confined to the liver, a liver transplant might be an option. Candidates for a liver transplant must meet strict criteria, including the absence of cancer outside the liver and a tumor size within specified limits. Liver transplants offer a chance for a cure but come with the risk of complications and the need for lifelong immunosuppression.
Non-surgical Treatments
Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop them from growing. It can be administered systemically or directly into the liver through a process called hepatic artery infusion. Chemotherapy may be used before surgery to shrink tumors or after surgery to eliminate any remaining cancer cells.
Radiation Therapy: This treatment uses high-energy rays to target and destroy cancer cells. Radiation therapy can be external or internal (brachytherapy) and is often used in combination with other treatments to control symptoms or slow the progression of the disease.
Targeted Therapy and Immunotherapy: These newer forms of treatment focus on specific aspects of cancer cells or the body’s immune response to fight the disease. Targeted therapies can block the growth and spread of cancer cells, while immunotherapies boost the body’s natural defenses to attack cancer cells. Both therapies offer a more personalized treatment approach, potentially with fewer side effects than traditional chemotherapy.
Emerging Treatments and Clinical Trials
The landscape of Cholangiocarcinoma treatment is continually evolving, with ongoing research and clinical trials exploring new therapies. Emerging treatments include novel targeted therapies, immunotherapies, and combination treatments that aim to improve outcomes and quality of life for patients. Participation in clinical trials can provide access to cutting-edge treatments and contribute to the advancement of medical knowledge in the fight against Cholangiocarcinoma.
However, the treatment of Cholangiocarcinoma requires a multifaceted approach tailored to the individual patient’s condition. While surgical options offer the potential for a cure in early-stage cancer, non-surgical treatments play a crucial role in managing advanced disease and improving survival rates. Emerging treatments and clinical trials continue to push the boundaries of what is possible, offering hope for more effective therapies in the future. Patients are encouraged to discuss all available treatment options with their healthcare team to determine the best course of action for their specific situation.
Managing Side Effects and Aftercare for Cholangiocarcinoma Treatments
Managing these side effects effectively and adhering to aftercare guidelines are crucial for improving the quality of life of patients and monitoring for potential recurrence. In this guide, we will explore the common side effects associated with cholangiocarcinoma treatments, strategies for managing these side effects, and the importance of follow-up care.
Common Side Effects of Cholangiocarcinoma Treatments
Treatments for cholangiocarcinoma, including surgery, chemotherapy, radiation therapy, and targeted therapy, can cause a range of side effects. These may vary based on the type of treatment, the individual’s overall health, and other factors. Common side effects include:
- Fatigue: A pervasive sense of tiredness that doesn’t improve with rest.
- Nausea and Vomiting: Particularly common with chemotherapy and radiation therapy.
- Appetite Loss: Treatment can affect taste and smell, reducing interest in food.
- Digestive Issues: Including diarrhea or constipation, often resulting from medication or the cancer itself.
- Liver Function Changes: Since the liver is closely involved, treatments may affect its function, indicated by jaundice or changes in blood tests.
Strategies for Managing Side Effects
Effective management of side effects is pivotal for maintaining the patient’s comfort and ensuring the continuation of treatment. Strategies include:
- Medication: Prescriptions can help manage nausea, pain, and digestive issues.
- Nutritional Support: Working with a dietitian to maintain a balanced diet can help manage appetite loss and maintain strength.
- Physical Activity: Gentle exercise, as recommended by a healthcare provider, can combat fatigue and improve overall well-being.
- Psychological Support: Counseling or support groups can help address the emotional and psychological impact of cancer treatment.
Importance of Follow-up Care and Monitoring for Recurrence
After completing treatment, ongoing follow-up care is essential to monitor for any signs of cancer recurrence and to manage long-term side effects. This care typically includes:
- Regular Check-ups: Including physical exams, blood tests, and imaging studies to detect any changes as early as possible.
- Managing Long-term Side Effects: Some side effects may persist or emerge long after treatment ends, requiring continued management.
- Lifestyle Adjustments: Recommendations for a healthy lifestyle to support recovery and overall health.
The journey through cholangiocarcinoma treatment is challenging, but with a comprehensive approach to managing side effects and dedicated aftercare, patients can achieve a better quality of life and effectively monitor for recurrence. Always communicate openly with your healthcare team about any side effects you experience so they can adjust your care plan as needed.
The Role of Lifestyle and Support in Cholangiocarcinoma Treatment
Cholangiocarcinoma, a form of cancer that affects the bile ducts, requires comprehensive treatment approaches that extend beyond medical interventions. Incorporating lifestyle modifications and leveraging robust support systems can significantly impact treatment outcomes and enhance the overall well-being of patients and their families. This article delves into the importance of lifestyle changes, psychological support, and the availability of resources and support groups in the treatment of cholangiocarcinoma.
Lifestyle Changes and Their Impact on Treatment Outcomes
Adopting healthy lifestyle habits plays a crucial role in the treatment and management of cholangiocarcinoma. Patients are encouraged to engage in regular physical activity, maintain a nutritious diet, and avoid tobacco and excessive alcohol consumption. These lifestyle adjustments can help improve the effectiveness of treatment, reduce the side effects of chemotherapy and radiation, and enhance the patient’s quality of life.
- Physical Activity: Moderate exercise can help mitigate fatigue, improve mood, and boost physical function without overtaxing the body.
- Nutritious Diet: A balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support the body’s healing process and immune function.
- Avoiding Harmful Substances: Eliminating tobacco use and limiting alcohol intake are essential, as these substances can interfere with treatment effectiveness and recovery.
Psychological Support and Coping Strategies for Patients and Families
The diagnosis of cholangiocarcinoma can be overwhelming, not just for the patient but also for their loved ones. Psychological support through counseling, support groups, and stress-reduction techniques is vital for managing the emotional and mental health challenges that come with the disease.
- Counseling Services: Professional therapists can provide coping strategies to deal with anxiety, depression, and the emotional toll of the disease.
- Support Groups: Joining support groups allows patients and families to connect with others facing similar challenges, fostering a sense of community and shared understanding.
- Stress-Reduction Techniques: Practices such as meditation, yoga, and deep-breathing exercises can help reduce stress and improve mental well-being.
Resources and Support Groups
A wealth of resources and support groups are available to cholangiocarcinoma patients and their families. These resources offer educational materials, emotional support, and practical advice to navigate the complexities of the disease.
- Educational Resources: Reliable information about cholangiocarcinoma, treatment options, and research developments is crucial for informed decision-making.
- Online and Local Support Groups: Both online platforms and local community groups provide invaluable spaces for sharing experiences, advice, and encouragement.
- Financial Assistance Programs: Many organizations offer financial aid and guidance to help manage the costs associated with treatment.
Meanwhile, psychological support and access to resources and support groups play essential roles in navigating the emotional and practical challenges of the disease. Together, these elements form a comprehensive treatment strategy that addresses the needs of patients and their families, fostering resilience and hope during a challenging time.
FAQs on Cholangiocarcinoma Treatment
What is Cholangiocarcinoma?
Cholangiocarcinoma, also known as bile duct cancer, is a rare and aggressive form of cancer that forms in the bile ducts, the tubes that carry bile from the liver to the gallbladder and small intestine. This type of cancer can cause significant health complications and requires prompt and specialized treatment.
How is Cholangiocarcinoma diagnosed?
Diagnosis of Cholangiocarcinoma typically involves a combination of blood tests, imaging studies (such as MRI, CT scans, and ultrasounds), and biopsy procedures. Doctors may also use advanced techniques like endoscopic retrograde cholangiopancreatography (ERCP) to examine the bile ducts and collect tissue samples for analysis.
What treatment options are available for Cholangiocarcinoma?
Treatment options for Cholangiocarcinoma depend on the stage of the cancer, its location, and the overall health of the patient. Common treatments include surgery to remove the tumor, liver transplantation for certain early-stage cancers, chemotherapy, radiation therapy, and targeted therapy. Sometimes, a combination of these treatments is used to achieve the best outcome.
Are there any side effects of Cholangiocarcinoma treatments?
Yes, treatments for Cholangiocarcinoma can have side effects, which vary depending on the type of treatment and the individual patient. Common side effects include fatigue, nausea, vomiting, loss of appetite, and changes in liver function. Targeted therapies and radiation may have specific side effects, and surgery carries risks of infection, bleeding, and complications related to anesthesia.
What is the prognosis for Cholangiocarcinoma?
The prognosis for Cholangiocarcinoma varies widely based on the cancer’s stage at diagnosis, the tumor’s location, and how well the cancer responds to treatment. Early-stage cancers that can be fully removed surgically tend to have a better prognosis. Advanced cancers, especially those that have spread to other parts of the body, typically have a more challenging outlook.
Can Cholangiocarcinoma be cured?
In some cases, Cholangiocarcinoma can be cured, especially if caught early and treated aggressively. However, due to its often late diagnosis and the cancer’s aggressive nature, achieving a cure can be difficult. Treatment may focus on extending life and improving the quality of life for those with advanced disease.
How can I manage the side effects of treatment?
Management of side effects involves close communication with your healthcare team. They can provide medications to help control symptoms such as nausea and pain, dietary recommendations to manage nutritional needs, and referrals to support services for emotional and psychological support.
Is there support available for patients with Cholangiocarcinoma?
Yes, there are numerous support resources available for patients with Cholangiocarcinoma and their families. These include patient advocacy organizations, support groups, counseling services, and educational resources. Your healthcare team can provide information on support networks that can help navigate the challenges of this disease.
Conclusion:
In conclusion, while cholangiocarcinoma remains a challenging diagnosis, the continuous evolution of research and treatment options brings us closer to a future where this disease can be managed more effectively.
Patients and their families are encouraged to stay informed, seek out specialized care, and consider all avenues of treatment.
With the collective efforts of the medical community, patients, and research scientists, the fight against cholangiocarcinoma is progressively becoming more promising.
Let us move forward with hope, knowing that every step taken is a step closer to overcoming cholangiocarcinoma.