Chagas Disease Symptoms: Chagas disease, also known as American trypanosomiasis, is a tropical parasitic illness caused by the protozoan parasite Trypanosoma cruzi.
This disease is primarily transmitted to humans through the feces of infected triatomine bugs, often referred to as “kissing bugs,” due to their propensity for biting the faces of humans.
Despite its concentration in Latin America, globalization and migration have expanded its presence to non-endemic countries, making it a global health concern.
What is Chagas Disease?
Chagas Disease, also known as American trypanosomiasis, is a tropical infectious disease caused by the parasite Trypanosoma cruzi. The disease is primarily transmitted to humans through the feces of infected triatomine bugs, often referred to as “kissing bugs”, due to their tendency to bite the faces of humans while they sleep. Transmission can also occur through contaminated food or drink, blood transfusions, organ transplants, and from mother to child during pregnancy.
Brief History and Geographic Prevalence
The disease was first discovered in 1909 by the Brazilian physician Carlos Chagas. It has since been identified primarily in Latin America where it is endemic in 21 countries. Chagas Disease affects millions of people and poses a significant public health challenge in rural areas where poverty is widespread and access to healthcare is limited. However, due to globalization and migration, the disease has spread to other continents, including North America and Europe, making it a global health concern.
Importance of Awareness and Diagnosis
Raising awareness about Chagas Disease is crucial for early diagnosis and treatment, which can significantly reduce the risk of chronic complications. The disease has an acute phase that is often symptom-free or presents with mild symptoms, leading many to overlook the need for medical attention. If left untreated, it can progress to a chronic phase, leading to severe cardiovascular and digestive system damage. Early detection and treatment can prevent these complications, underscoring the importance of awareness, especially in endemic regions and among at-risk populations. Enhanced diagnostic efforts, along with education on preventive measures, are key to controlling the spread of Chagas Disease and safeguarding public health.
Causes of Chagas Disease
Understanding the transmission routes, along with the environmental and social factors contributing to its spread, is crucial for prevention and control. This article delves into these aspects, aiming to enhance awareness and knowledge about the disease.
Transmission Routes
Chagas disease is primarily transmitted through the feces of infected triatomine bugs, often referred to as “kissing bugs.” These bugs become infected by feeding on the blood of an animal or person with Chagas disease. They then transmit the disease to humans in the following ways:
- Direct Contact: When the bug defecates on the skin, usually near the eyes or mouth, and the feces enter the body through mucous membranes or breaks in the skin.
- Contaminated Food or Drink: Consumption of food or beverages contaminated with T. cruzi from infected bug feces or infected animals.
- Congenital Transmission: From a pregnant person to their baby, which can occur during pregnancy or childbirth.
- Blood Transfusion and Organ Transplants: Through transfusions of blood or transplants of organs from infected donors.
- Accidental Laboratory Exposure: Laboratory personnel may be exposed to the parasite accidentally.
Environmental and Social Factors
The spread of Chagas disease is significantly influenced by environmental and social factors, including:
- Poor Housing Conditions: Homes made of materials such as mud, straw, and palm thatch offer ideal hiding spots for triatomine bugs, facilitating their contact with humans.
- Deforestation and Urbanization: These processes disrupt the natural habitat of triatomine bugs and their wild animal hosts, leading to bugs moving closer to human habitats.
- Socioeconomic Status: Poverty is closely linked to the prevalence of Chagas disease due to the association with living conditions that favor the presence of triatomine bugs.
- Migration: Infected individuals moving to non-endemic areas can lead to the spread of the disease through blood transfusions, organ transplants, and congenital transmission.
However, tackling Chagas disease requires a multifaceted approach that addresses its complex transmission routes and the environmental and social determinants that fuel its spread. Efforts must include improving living conditions, educating at-risk populations, and implementing effective vector control measures. Awareness and understanding of these factors are vital for the development of strategies to combat this neglected tropical disease effectively.
Symptoms of Chagas Disease
Understanding these symptoms is crucial for early detection and treatment, which can significantly improve outcomes for those affected. This article aims to elucidate the symptoms associated with both phases of Chagas disease, highlighting the variability and progression of symptoms.
Acute Phase Symptoms
The acute phase of Chagas disease typically begins soon after infection, lasting for about 4-8 weeks. This phase is often asymptomatic or presents with mild symptoms, making it difficult to diagnose. However, when symptoms do appear, they may include:
- Fever or unexplained high temperature
- Swelling at the infection site (where the parasite entered the body)
- Fatigue or general feeling of being unwell
- Swollen glands
- Rash or skin lesions
- Headache and body aches
- Loss of appetite, nausea, or diarrhea
- Swelling around the eye if infected through the ocular route
In children, the symptoms can be more pronounced than in adults. Despite these potential symptoms, the acute phase often goes unnoticed because they are nonspecific and can be mistaken for other common illnesses.
Chronic Phase Symptoms
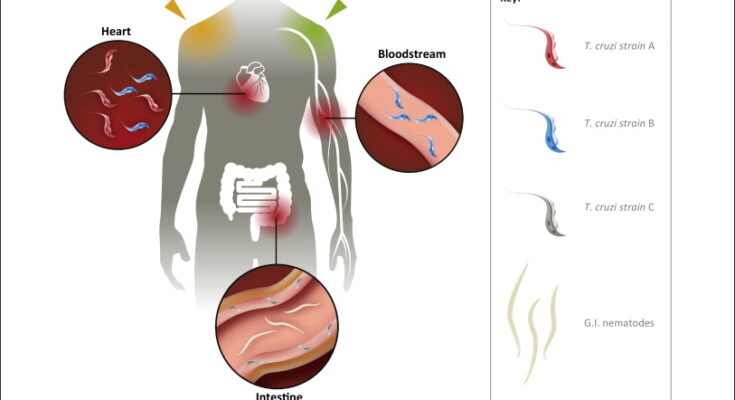
The chronic phase of Chagas disease may remain silent for years or even decades after initial infection, with about 60-70% of individuals never experiencing further symptoms. However, approximately 30-40% of infected people will develop severe and potentially life-threatening complications, including:
- Cardiac complications: enlarged heart (cardiomyopathy), heart failure, altered heart rate or rhythm (arrhythmias), and sudden cardiac arrest
- Gastrointestinal complications: enlarged esophagus (megaesophagus) or colon (megacolon), leading to difficulties in swallowing, chronic constipation, and abdominal pain
The transition from the acute to the chronic phase is often gradual, and without noticeable symptoms, making the chronic phase particularly dangerous. The variability in symptom progression underscores the importance of early diagnosis and monitoring for individuals at risk of or suspected to have Chagas disease.
Highlighting the Variability and Progression of Symptoms
The progression from the acute to the chronic phase of Chagas disease and the variability of symptoms pose significant challenges for diagnosis and treatment. Many affected individuals may not realize they are infected until the disease has progressed to the chronic phase, which can lead to severe health complications.
Awareness of the potential signs and symptoms, particularly for those living in or traveling to endemic areas, is crucial for early intervention. Additionally, individuals who have been diagnosed with Chagas disease should undergo regular monitoring to manage and mitigate the impact of chronic phase complications.
However, Chagas disease symptoms vary widely from the acute phase to the chronic phase, emphasizing the need for awareness and early detection. By understanding the symptoms associated with each phase, individuals and healthcare providers can better identify and treat this potentially life-threatening disease.
For those at risk, early consultation with a healthcare provider upon noticing any related symptoms can lead to timely diagnosis and treatment, significantly improving the prognosis for individuals with Chagas disease.
Diagnosis of Chagas Disease
Chagas disease, caused by the protozoan parasite Trypanosoma cruzi, is a significant public health issue in Latin America and has been spreading to other parts of the world due to increased mobility and migration. Accurate and timely diagnosis is critical for effective management and treatment of the disease. This section delves into the various diagnostic tests and criteria for Chagas disease, highlights the importance of early detection, and discusses the challenges involved in diagnosing this complex disease.
Diagnostic Tests and Criteria
The diagnosis of Chagas disease involves a combination of clinical evaluation, serological tests, and parasitological techniques. The approach to diagnosis may vary depending on the stage of the disease—acute or chronic—and the availability of diagnostic resources. The main diagnostic methods include:
Serological Tests: These are the cornerstone for diagnosing chronic Chagas disease. Tests such as Enzyme-linked Immunosorbent Assay (ELISA), Indirect Immunofluorescence (IIF), and Western Blot are used to detect antibodies against T. cruzi in the blood. A positive result from two different serological tests is generally required for confirmation.
Parasitological Tests: Direct visualization of parasites in blood samples is crucial for acute phase diagnosis. Techniques such as microscopic examination of fresh blood or its derivatives, and the Strout method, are commonly employed. Polymerase Chain Reaction (PCR) tests can also detect T. cruzi DNA in blood, which is especially useful in the early acute phase and for congenital transmissions.
Xenodiagnosis and Hemoculture: These are more traditional methods where live, non-infected triatomine bugs are allowed to feed on the patient’s blood (xenodiagnosis) or blood samples are cultured to promote parasite growth (hemoculture). While these methods can be effective, they are less commonly used due to their complexity and longer time frames for obtaining results.
Importance of Early Detection
Early detection of Chagas disease is paramount for several reasons. In the acute phase, the disease is more amenable to treatment, with antiparasitic therapies being most effective. Early treatment can significantly reduce the risk of chronic complications, such as cardiac and gastrointestinal disorders, which are associated with high morbidity and mortality. Furthermore, identifying and treating infected individuals can help prevent transmission, especially in cases of congenital Chagas disease, blood transfusion, and organ transplantation.
Challenges in Diagnosis
Despite the availability of diagnostic methods, several challenges hinder the early detection and accurate diagnosis of Chagas disease:
- Lack of Awareness and Access: In many endemic regions, there is a lack of awareness about Chagas disease among healthcare providers and the population. Combined with limited access to healthcare services, this results in underdiagnosis and delayed treatment.
- Asymptomatic Nature: The acute phase of Chagas disease is often asymptomatic or presents with non-specific symptoms, making it difficult to recognize and diagnose early.
- Cross-reactivity and False Positives: Serological tests may cross-react with other parasitic infections, leading to false-positive results. This necessitates confirmatory testing, which can be resource-intensive.
- Limited Resources: In non-endemic countries, there may be a lack of laboratory facilities equipped to perform the necessary diagnostic tests, delaying diagnosis and treatment.
However, the diagnosis of Chagas disease relies on a combination of serological and parasitological tests, with early detection playing a critical role in effective disease management. However, challenges such as lack of awareness, asymptomatic presentation, and limited resources complicate the diagnosis process. Addressing these challenges is crucial for improving the outcomes for individuals affected by Chagas disease and for controlling its spread.
Treatment and Management of Chagas Disease
Effective treatment and management are crucial for mitigating its impact on health. This article explores the current treatment options available for Chagas disease and underscores the importance of medical care and follow-up.
Current Treatment Options
The treatment for Chagas disease primarily involves antiparasitic medications, which are most effective when administered during the acute phase of the infection. The two main drugs used are:
- Benznidazole: This medication is the cornerstone of Chagas disease treatment. It is most effective in the early stages of the disease but can also be used in chronic cases to reduce disease progression.
- Nifurtimox: An alternative to Benznidazole, Nifurtimox is also used to treat both acute and chronic stages of Chagas disease. Its effectiveness varies depending on the geographic origin of the infection due to differing strains of the T. cruzi parasite.
These drugs work by killing the T. cruzi parasite in the bloodstream. However, their efficacy diminishes the longer the infection has been present, highlighting the importance of early diagnosis and treatment.
Side Effects
Both Benznidazole and Nifurtimox can have side effects, ranging from mild to severe, including allergic reactions, gastrointestinal symptoms, and neurological symptoms. Regular monitoring by healthcare professionals is necessary to manage these side effects effectively.
The Importance of Medical Care and Follow-Up
Continuous medical care and follow-up are paramount in the treatment of Chagas disease, especially considering the potential for chronic complications such as heart disease and gastrointestinal issues. Regular check-ups allow healthcare providers to monitor the effectiveness of treatment, manage side effects, and adjust therapeutic strategies as needed.
Early intervention and consistent care can significantly improve the quality of life for those affected by Chagas disease. It’s essential for patients to adhere to treatment plans and for healthcare systems to support access to necessary medications and follow-up care.
However, while there is no vaccine for Chagas disease, current treatment options can be effective, especially when started early. The management of the disease requires a comprehensive approach that includes antiparasitic therapy, symptom management, and regular monitoring by healthcare professionals to address any complications that arise. The key to combating Chagas disease lies in early detection, effective treatment, and continuous care and support for patients throughout their recovery journey.
Prevention of Chagas Disease
Here are essential strategies to prevent Chagas disease, focusing on avoiding infection, improving living conditions, ensuring food and drink safety, and screening blood and organ donations.
Preventive Measures to Avoid Infection
One of the primary ways to prevent Chagas disease is to avoid contact with the triatomine bugs, also known as “kissing bugs,” that transmit the parasite. This can be achieved through:
- Installing screens on windows and doors to keep bugs out.
- Using insect repellent on exposed skin and sleeping areas.
- Ensuring pets sleep indoors, as they can also be carriers of the bugs.
Improving Living Conditions to Prevent Bug Infestation
Improving housing and living conditions is a vital step in preventing Chagas disease. The triatomine bugs thrive in cracks and crevices of poorly constructed homes. To reduce bug infestations, consider the following:
- Repairing and sealing cracks in walls, floors, and roofs.
- Moving beds away from walls and ensuring that beddings do not touch the floor.
- Utilizing plaster or cement to smooth walls and eliminate bug hiding places.
- Encouraging community-wide efforts to maintain clean living environments, reducing the places where triatomine bugs can breed.
Safe Food and Drink Practices
Transmission of Chagas disease can also occur through the consumption of contaminated food and drink. To mitigate this risk, it is important to:
- Wash and cook all fruits and vegetables thoroughly to kill any parasites.
- Ensure that juices and other beverages are from safe, treated sources, especially in areas where Chagas disease is endemic.
- Educate food handlers on safe preparation practices to prevent contamination.
Screening Blood and Organ Donations
Since Chagas disease can be transmitted through blood transfusions and organ transplants, screening donors is a critical preventive measure. Health facilities should:
- Implement routine screening for Chagas disease in blood banks and organ donation programs.
- Use validated tests to detect Trypanosoma cruzi infection in potential donors.
- Ensure that individuals diagnosed with Chagas disease receive appropriate counseling and care to prevent transmission to others.
Preventing Chagas disease requires a comprehensive approach that includes both individual and community efforts. By taking steps to avoid infection, improve living conditions, practice safe food and drink habits, and screen blood and organ donations, we can significantly reduce the incidence and spread of this disease. Public health education and community engagement are key to implementing these preventive measures effectively and sustainably.
Global Impact and Efforts to Combat Chagas Disease
Chagas disease, also known as American trypanosomiasis, is a tropical parasitic disease that has garnered significant attention due to its widespread impact and the challenges associated with its control and elimination. This section delves into the global prevalence of Chagas disease and outlines the concerted efforts by health organizations worldwide to combat this enduring health issue.
Global Prevalence of Chagas Disease
Chagas disease primarily affects populations in Latin America, where it is endemic. However, globalization and migration have extended its reach to other continents, making it a global health concern. According to the World Health Organization (WHO), an estimated 6 to 7 million people worldwide are infected with Trypanosoma cruzi, the parasite responsible for Chagas disease. The disease manifests in two phases: the acute phase, which often goes unnoticed due to its mild symptoms, and the chronic phase, which can lead to severe cardiac and digestive problems.
The distribution of Chagas disease is not uniform, with significant variations in prevalence rates across different countries and regions. In endemic countries, the disease disproportionately affects rural and impoverished communities, where living conditions favor the proliferation of the triatomine bugs that transmit the parasite.
Efforts to Combat Chagas Disease
Recognizing the severity of Chagas disease and its impact on public health, various health organizations have initiated efforts to control and eliminate the disease. These efforts are multifaceted, addressing both the immediate need for treatment and the long-term goal of transmission reduction.
- Screening and Diagnosis: Improving access to diagnostic tools and screening programs is crucial for early detection and treatment. Initiatives to enhance diagnostic capacities in endemic and non-endemic countries aim to reduce the burden of the disease.
- Vector Control: Vector control programs focus on reducing the population of triatomine bugs through insecticide spraying and housing improvements to prevent bug infestation. These measures have been successful in reducing transmission rates in several regions.
- Access to Treatment: Enhancing access to antiparasitic treatment for infected individuals, especially during the acute phase of the disease, is a priority. Efforts are also underway to develop more effective and less toxic treatment options.
- Education and Awareness: Raising awareness about Chagas disease among healthcare professionals and at-risk populations is vital for early detection and treatment. Educational campaigns aim to inform communities about prevention methods and the importance of seeking treatment.
- International Collaboration: The global nature of Chagas disease necessitates international collaboration. Organizations like the WHO, the Pan American Health Organization (PAHO), and various non-governmental organizations (NGOs) are working together to coordinate research, control efforts, and funding to combat the disease more effectively.
However, while the global impact of Chagas disease remains significant, concerted efforts by health organizations are making strides in controlling and aiming to eliminate the disease. Through improved diagnosis, vector control, access to treatment, education, and international collaboration, there is hope for reducing the burden of Chagas disease on affected populations worldwide. Achieving these goals requires sustained commitment and resources, highlighting the importance of continued global attention to this neglected tropical disease.
FAQs about Chagas Disease
What is Chagas Disease?
Chagas disease is a condition transmitted by the triatomine bug, often referred to as the “kissing bug.” These bugs become infected with T. cruzi by biting an infected animal or person. Once infected, the bug can transmit the parasite to humans and other mammals. The disease has two phases: the acute phase, which occurs shortly after infection, and the chronic phase, which can develop over many years.
How is Chagas Disease Transmitted?
The primary route of transmission is through the feces of infected triatomine bugs. These bugs bite and then defecate on the skin, allowing the parasite to enter the host through the bite wound or mucous membranes. Other transmission methods include congenital transmission (from a pregnant mother to her baby), blood transfusions, organ transplantation from infected donors, and consumption of food contaminated with the parasite.
What are the Symptoms of Chagas Disease?
In its acute phase, Chagas disease may cause symptoms like fever, fatigue, body aches, headache, rash, loss of appetite, diarrhea, and vomiting. The most noticeable sign can be a swelling at the infection site, known as a chagoma, or an eyelid swelling called Romaña’s sign. However, up to 70% of people may not show any symptoms during the acute phase. In the chronic phase, the disease can lead to serious heart and digestive system disorders.
How is Chagas Disease Diagnosed?
Diagnosis in the acute phase is typically through detection of the parasite in the blood using microscopic examination or polymerase chain reaction (PCR) tests. In the chronic phase, diagnosis is often made through serological tests, which detect antibodies against T. cruzi.
Can Chagas Disease be Treated?
Yes, Chagas disease can be treated, especially if caught early. The two medications used are benznidazole and nifurtimox, both of which can be almost 100% effective in curing the disease if given soon after infection. Treatment in the chronic phase is also possible but focuses more on managing symptoms and preventing the progression of the disease.
Is There a Vaccine for Chagas Disease?
Currently, there is no vaccine available for Chagas disease. Prevention mainly involves controlling triatomine bugs, screening blood donations, and testing organ donors and pregnant women in endemic areas to prevent congenital transmission.
How Can I Prevent Chagas Disease?
Prevention strategies include improving living conditions to prevent bug infestation, using insecticide-treated bed nets, applying insect repellent, and eating food that is safely prepared and stored to avoid contamination. In endemic areas, regular screening for the disease is also important for early detection and treatment.
Conclusion
For those among us who find themselves at risk, whether due to genetic factors, environmental exposure, or lifestyle choices, the encouragement to seek testing and treatment cannot be overstated. Taking proactive steps towards health screening and medical consultations can make a profound difference in one’s quality of life. It’s a gesture of self-care that extends its benefits to our loved ones by safeguarding our health and ensuring our ability to participate fully in our shared lives.
In conclusion, the journey towards health and well-being is a collective endeavor. By recognizing the importance of symptom awareness, advocating for early testing and treatment, and contributing to global health improvement efforts, we take essential steps towards a healthier, more informed world. Let’s commit to this path, not just for our sake, but for the well-being of future generations. Together, we can make a significant impact in the global fight against disease and ill-health, paving the way for a brighter, healthier future for all.