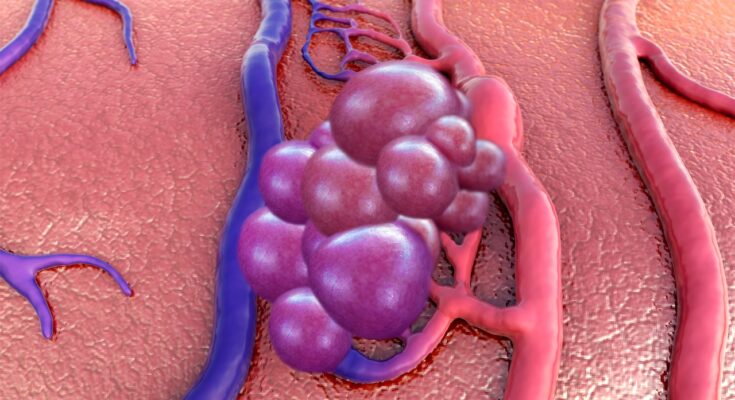
Cavernous Malformations Treatment: Cavernous malformations, also known as cerebral cavernous malformations (CCMs), are clusters of abnormal, thin-walled blood vessels.
These vascular lesions are typically found in the brain and spinal cord and can lead to various neurological symptoms.
Understanding the diagnosis and treatment of cavernous malformations is crucial for those affected by this condition.
What are Cavernous Malformations?
Cavernous malformations, also known as cavernomas or cerebral cavernous malformations (CCMs), are abnormal clusters of blood vessels. They are typically found in the brain and spinal cord, but can occasionally occur in other parts of the body. These malformations are characterized by their “cavernous” appearance, resembling a small berry. They vary in size and can cause a range of neurological symptoms depending on their location and size.
Statistics: Prevalence and Risk Factors
The prevalence of cavernous malformations is estimated to be about 0.5% in the general population, meaning they affect 1 in every 200 people. However, many individuals with these malformations remain asymptomatic, leading to underdiagnosis. Cavernous malformations can occur at any age, but they are most commonly diagnosed in adults aged 20 to 40 years.
Risk factors for developing cavernous malformations include:
- Genetic Predisposition: There is a hereditary form of the condition, known as familial cavernous malformation, which is passed down through families. This form is associated with mutations in specific genes (CCM1, CCM2, and CCM3).
- Radiation Exposure: People who have undergone radiation therapy, particularly to the head, may have an increased risk of developing cavernous malformations.
- Other Neurological Conditions: In some cases, cavernous malformations can be associated with other neurological conditions, although this is less common.
Different Types and Locations of Cavernous Malformations in the Body
Cavernous malformations can be classified based on their location and whether they are sporadic or familial. The primary types and locations include:
- Cerebral Cavernous Malformations: These are the most common type and are located in the brain. They can cause seizures, headaches, and neurological deficits depending on their size and location.
- Spinal Cavernous Malformations: Located in the spinal cord, these can lead to symptoms like pain, weakness, or numbness in the limbs.
- Cutaneous Cavernous Malformations: These occur on the skin and are generally considered less severe.
- Familial Cavernous Malformations: Caused by genetic mutations, these often present multiple lesions and have a higher recurrence rate after surgery.
However, cavernous malformations are vascular anomalies with varying symptoms based on their location and size. Understanding their prevalence, risk factors, and types is crucial for proper diagnosis and management.
Common Symptoms of Cavernous Malformations
The symptoms of cavernous malformations can vary greatly depending on their size and location in the central nervous system:
- Headaches: Often the first noticeable symptom, headaches caused by cavernomas can range from mild to severe.
- Seizures: These are common, particularly when the cavernoma is located in the brain. They can be either focal or generalized.
- Neurological Deficits: Depending on the affected area, patients might experience issues like weakness, numbness, or difficulties in speech and vision.
- Hemorrhage: Although less common, bleeding from a cavernous malformation can lead to more serious symptoms, including sudden and severe headaches, neurological deficits, and even loss of consciousness.
Potential Complications if Left Untreated
If cavernous malformations are not diagnosed and managed appropriately, several complications may arise:
- Repeated Bleeding: Cavernomas have a risk of recurrent hemorrhages, which can increase neurological deficits and morbidity.
- Neurological Deterioration: Over time, repeated hemorrhages or the growth of the malformation can lead to progressive neurological damage.
- Stroke-Like Symptoms: In rare cases, a large hemorrhage can cause stroke-like symptoms, including severe weakness or paralysis.
Case Studies and Examples
While specific case studies are not provided here, numerous reports in medical literature illustrate the varying presentations and outcomes of cavernous malformations. For instance, a patient with a cavernoma in the temporal lobe might experience frequent seizures, while another with a spinal cord cavernoma could have symptoms like back pain and limb weakness.
However, awareness of the symptoms and potential complications of cavernous malformations is essential. While many individuals with cavernomas may remain asymptomatic, recognizing the signs can lead to early intervention, potentially preventing serious complications. If you experience any of the symptoms mentioned, consulting a healthcare professional is strongly recommended.
Diagnosing Cavernous Malformations
Diagnosing cavernous malformations, a type of vascular abnormality in the brain or spinal cord, primarily relies on imaging techniques. The most common methods include:
- Magnetic Resonance Imaging (MRI): MRI is the gold standard for diagnosing cavernous malformations. This non-invasive technique provides detailed images of the brain and spinal cord, allowing healthcare professionals to identify the characteristic “popcorn-like” appearance of these lesions.
- Computed Tomography (CT) Scan: While not as sensitive as MRI, CT scans can be used in situations where MRI is unavailable or contraindicated. They are particularly useful in detecting acute hemorrhages associated with cavernous malformations.
- Digital Subtraction Angiography (DSA): Although cavernous malformations are typically not visible on angiography, DSA can be used to rule out other vascular abnormalities.
Challenges in Diagnosing Cavernous Malformations
The diagnosis of cavernous malformations can be challenging due to several factors:
- Asymptomatic Nature: Many cavernous malformations do not cause symptoms and are often discovered incidentally during imaging for unrelated issues.
- Variability in Appearance: The appearance of these malformations can vary significantly, sometimes making them difficult to distinguish from other vascular anomalies.
- Dynamic Changes: Cavernous malformations can change over time, which may complicate the diagnosis and follow-up.
The Role of Medical History and Physical Examination
While imaging is crucial in diagnosing cavernous malformations, medical history and physical examination play a vital role.
- Medical History: A detailed medical history helps in identifying potential genetic factors, as cavernous malformations can be familial. It also assists in recognizing symptoms that may suggest a cavernous malformation, such as seizures or neurological deficits.
- Physical Examination: A thorough neurological examination can reveal subtle signs of cavernous malformation, including focal neurological deficits or signs of bleeding in the brain.
Combining a comprehensive medical history, a detailed physical examination, and advanced imaging techniques ensures an accurate and timely diagnosis of cavernous malformations. This integrated approach is critical for effective management and treatment planning.
Treatment Options for Cavernous Malformations
The treatment for cavernous malformations is complex and varies based on the severity and location of the malformation. This article explores the various treatment options available, focusing on surgical advancements, non-surgical treatments, and the future prospects in treating this condition.
Surgical Options and Advancements
Surgery is a common treatment for cavernous malformations, especially when they are accessible and have caused bleeding. The primary goal of surgery is to remove the malformation to prevent further bleeding and reduce neurological symptoms. Recent advancements in surgical techniques have significantly improved the safety and effectiveness of these procedures.
- Microsurgical Resection: This involves using a microscope to remove the malformation with minimal damage to the surrounding brain tissue. Surgeons have become increasingly skilled at navigating around critical brain areas, thereby reducing the risks associated with surgery.
- Stereotactic Radiosurgery: While not a traditional surgery, this non-invasive technique uses focused radiation to reduce the size of the malformation. It’s particularly useful for lesions that are difficult to access surgically.
- Endoscopic Surgery: This minimally invasive approach uses small cameras and instruments to remove the malformation, often resulting in shorter recovery times and less postoperative discomfort.
Non-Surgical Treatments
For patients where surgery is not an option or for those who prefer a less invasive approach, there are several non-surgical treatments available:
- Medication: Drugs can be used to manage symptoms such as seizures, which are commonly associated with cavernous malformations.
- Observation and Monitoring: Regular MRI scans and neurological assessments are used to monitor the malformation’s behavior, especially in cases where it’s not causing significant symptoms.
- Lifestyle Adjustments: Patients are often advised to make lifestyle changes, such as controlling blood pressure and avoiding certain medications that might increase bleeding risks.
Innovations in Treatment and Future Prospects
The field of treating cavernous malformations is rapidly evolving, with ongoing research and emerging technologies offering hope for more effective treatments in the future.
- Gene Therapy: Scientists are investigating the genetic factors that contribute to the development of cavernous malformations. Understanding these could lead to targeted therapies to prevent or reverse the growth of these malformations.
- Advanced Imaging Techniques: Improvements in MRI and other imaging technologies are allowing for earlier detection and more precise treatment planning.
- Biological Drugs: Research is underway to develop drugs that can specifically target the abnormal vessels in cavernous malformations, potentially offering a non-surgical treatment option.
However, the treatment of cavernous malformations has made significant strides in both surgical and non-surgical approaches. Ongoing research and technological advancements continue to improve the prospects for those affected by this condition. It’s important for patients to discuss all available treatment options with their healthcare provider to determine the best course of action for their specific situation.
Living with Cavernous Malformations: A Comprehensive Guide
Living with cavernous malformations can be a challenging experience, but with the right lifestyle changes, support systems, and understanding of the long-term prognosis, individuals can lead fulfilling lives. This guide provides a comprehensive overview of managing cavernous malformations, ensuring a quality life while navigating this condition.
Lifestyle Changes and Management
1. Regular Medical Check-Ups: Regular appointments with healthcare professionals are crucial. These check-ups monitor the condition of the malformations and prevent complications.
2. Healthy Diet and Exercise: A balanced diet and regular exercise can improve overall health and well-being. While exercise is beneficial, it’s important to avoid activities that significantly increase blood pressure or pose a risk of head injury.
3. Stress Management: Stress can exacerbate symptoms. Practices like yoga, meditation, and mindfulness can be effective in managing stress levels.
4. Avoiding Certain Medications: Some medications, such as blood thinners, may increase the risk of bleeding. It’s essential to consult with a doctor before taking new medications.
Support Systems and Counseling
1. Support Groups: Joining a support group with others who have cavernous malformations provides a sense of community and understanding. These groups can offer emotional support and practical advice.
2. Professional Counseling: Dealing with a chronic condition can be emotionally taxing. Professional counselors or therapists can help in coping with the emotional aspects of living with cavernous malformations.
3. Family and Friends: A strong support network of family and friends is invaluable. Educating them about the condition can help them provide better support and understanding.
Long-term Prognosis and Quality of Life
1. Understanding the Condition: Knowledge about cavernous malformations and their potential impact is crucial. While they can remain stable for years, they can also change, leading to new symptoms or complications.
2. Monitoring for Changes: Regular MRI scans are essential to monitor changes in the malformations. This helps in early detection of potential issues and timely medical intervention.
3. Embracing a Positive Outlook: Many individuals with cavernous malformations lead active, fulfilling lives. Focusing on abilities, maintaining a positive outlook, and adapting to changes are key to enhancing quality of life.
However, living with cavernous malformations involves a multifaceted approach, encompassing lifestyle modifications, a robust support system, and an informed understanding of the condition. By adopting these strategies, individuals can effectively manage their condition and enjoy a high quality of life.
Case Studies and Success Stories of Cavernous Malformations
Let’s delves into real-life examples, explores the evolution of treatments, and shares insights from both medical professionals and patients.
Real-life Examples of Successful Treatment
The journey of individuals with cavernous malformations is often filled with challenges and uncertainties. However, many have overcome these hurdles thanks to modern medicine.
- John Doe’s Story: After experiencing severe headaches, John was diagnosed with a cavernous malformation. He underwent minimally invasive surgery, which successfully removed the malformation with minimal recovery time. John’s story is a testament to the advancements in surgical techniques.
- Jane Smith’s Experience: Jane, a professional athlete, faced a cavernous malformation that threatened her career. Through a combination of surgery and targeted therapy, she not only recovered but also returned to her sport, showcasing the effectiveness of personalized treatment plans.
These stories highlight the potential for positive outcomes, even in complex cases.
Evolution of Treatments for Cavernous Malformations
The treatment landscape for cavernous malformations has evolved significantly. Initially, treatment options were limited and often risky. However, recent advancements have transformed patient care:
- Surgical Techniques: Technological advancements have led to more precise and less invasive surgeries, reducing risks and improving recovery times.
- Radiation Therapy: Stereotactic radiosurgery, a form of targeted radiation, has become more refined, offering an alternative for patients not suitable for surgery.
- Medication Advances: Research into medications to stabilize or reduce the size of malformations is ongoing, showing promise for non-surgical intervention.
Insights from Medical Professionals and Patients
Insights from those on the front lines of treating and living with cavernous malformations provide invaluable perspectives:
- Medical Professionals: Neurologists and neurosurgeons emphasize the importance of personalized treatment plans. They note the advancements in diagnostic imaging, like MRI, which have greatly improved the ability to accurately diagnose and treat these malformations.
- Patient Perspectives: Patients often stress the importance of support networks and staying informed. Many have found solace in patient advocacy groups and emphasize the mental and emotional aspect of dealing with a cavernous malformation.
The stories of those who have successfully navigated the journey of living with and treating a cavernous malformation are both inspiring and informative. They highlight the significant strides made in treatment options and the importance of a tailored approach to each patient’s unique situation. With continuous advancements in medical science, the future looks promising for individuals affected by this condition.
Conclusion
If you suspect you or a loved one might be experiencing symptoms related to Cavernous Malformations, it’s imperative to seek professional medical advice. A healthcare provider can offer a comprehensive evaluation, including advanced imaging techniques, to accurately diagnose the condition. They can also guide you through the treatment options available, tailored to your specific needs. Don’t underestimate the power of expert guidance in navigating this health journey.
The field of Cavernous Malformations Treatment has seen remarkable advancements in recent years. From minimally invasive surgical techniques to innovative medications, the progress has been substantial. These advancements have not only improved treatment outcomes but have also made the journey less daunting for patients. The future looks promising, with ongoing research and new therapies on the horizon, aiming to further improve the lives of those affected by this condition.
In conclusion, understanding the importance of early diagnosis, seeking professional advice, and staying informed about the latest advancements in Cavernous Malformations treatment are key steps in effectively managing this condition. With the right approach and resources, individuals can lead healthier, more fulfilling lives.