Autoimmune Pancreatitis Symptoms: Autoimmune Pancreatitis (AIP) is a unique form of pancreatitis marked by the body’s immune system attacking the pancreas, causing inflammation and damage.
This relatively rare disorder is often misdiagnosed due to its similarity to other pancreatic diseases.
What is Autoimmune Pancreatitis?
Autoimmune pancreatitis (AIP) is a unique form of pancreatitis distinguished by its autoimmune characteristics. Unlike other types of pancreatitis, which are often associated with alcohol consumption or gallstones, AIP involves the immune system attacking the pancreas, leading to inflammation and damage.
Differentiation from Other Types of Pancreatitis
What sets AIP apart from other forms of pancreatitis is its autoimmune origin. Other common types, such as acute and chronic pancreatitis, usually result from alcohol abuse, gallstones, or genetic disorders. AIP, on the other hand, is an immune-mediated condition and often responds well to corticosteroid therapy, which is not typically effective in other types of pancreatitis.
Prevalence and Demographics Affected
AIP is relatively rare compared to other forms of pancreatitis. It is more prevalent in males and often occurs in middle-aged or older individuals. The exact prevalence is hard to determine due to misdiagnosis or underdiagnosis, but understanding its distinct characteristics can aid in more accurate identification and treatment. This condition also has a global presence, although the incidence rates may vary across different regions and ethnic groups.
However, autoimmune pancreatitis is a distinct, immune-mediated form of pancreatitis that requires accurate diagnosis and appropriate treatment. Its differentiation from other types of pancreatitis is crucial for effective management and improving patient outcomes.
Symptoms of Autoimmune Pancreatitis
This comprehensive guide delves into the common symptoms of autoimmune pancreatitis, contrasts them with those of other pancreatic diseases, and includes real-life case studies for a better understanding.
Common Symptoms of Autoimmune Pancreatitis
- Abdominal Pain: Often a dull ache in the upper abdomen, this is a frequent symptom. It’s less severe than the acute pain seen in other types of pancreatitis.
- Jaundice: Yellowing of the skin and eyes due to bile duct obstruction is common in autoimmune pancreatitis. This contrasts with other pancreatic conditions where jaundice might be less frequent.
- Weight Loss: Unexplained weight loss is a notable symptom, occurring as the body fails to digest food properly.
- Steatorrhea: Fatty stools, or steatorrhea, are a result of poor digestion and absorption of fats, a key sign of pancreatic dysfunction.
- Diabetes: New-onset diabetes can be a symptom due to the pancreas’ impaired ability to produce insulin.
Differentiating Symptoms from Other Pancreatic Diseases
- Pain Intensity: Autoimmune pancreatitis usually results in less severe pain compared to acute pancreatitis.
- Onset of Diabetes: Unlike in pancreatic cancer where diabetes develops rapidly, in autoimmune pancreatitis, it progresses more slowly.
- Response to Steroids: A unique aspect of autoimmune pancreatitis is its responsiveness to steroid therapy, which is not observed in other types of pancreatic diseases.
Real-Life Context: Case Studies and Anecdotes
- Case Study 1: A 45-year-old patient, initially misdiagnosed with pancreatic cancer, experienced remarkable symptom relief with steroid therapy, confirming autoimmune pancreatitis.
- Anecdote: A patient’s journey from experiencing persistent abdominal pain and weight loss to the eventual diagnosis of autoimmune pancreatitis, highlighting the importance of distinguishing symptoms.
However, understanding these symptoms and their nuances is crucial for distinguishing autoimmune pancreatitis from other pancreatic conditions. Real-life case studies further illuminate the importance of accurate diagnosis and appropriate treatment.
Causes of Autoimmune Pancreatitis
Understanding its causes can be complex, as the exact mechanism behind this condition is not entirely clear. However, research suggests that the following factors play a significant role:
- Genetic Predisposition: There is evidence that genetic factors may contribute to the development of autoimmune pancreatitis. Individuals with certain genetic markers or a family history of autoimmune disorders are at a higher risk.
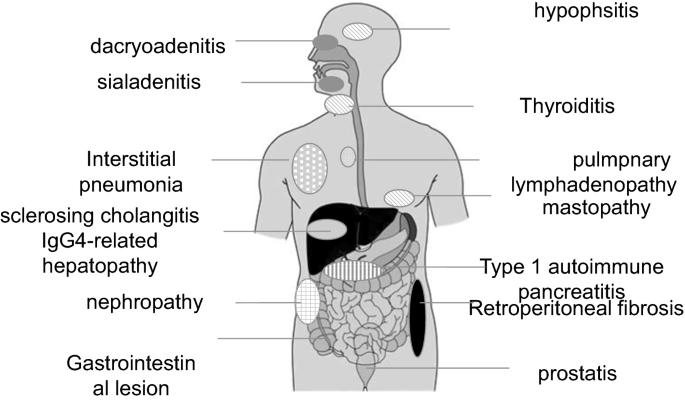
- Immune System Disorders: Autoimmune pancreatitis often occurs in association with other autoimmune conditions. This suggests that dysregulation of the immune system plays a key role in its development.
- Environmental Factors: Exposure to certain environmental factors, such as viral infections or toxins, might trigger the onset of autoimmune pancreatitis in susceptible individuals.
Risk Factors and Triggers
Identifying risk factors and triggers is crucial for both preventing and managing autoimmune pancreatitis. Some of the known risk factors and potential triggers include:
- Age and Gender: Autoimmune pancreatitis is more commonly diagnosed in middle-aged and elderly individuals, with a higher prevalence in men than in women.
- Autoimmune Disorders: People with other autoimmune diseases, such as Sjögren’s syndrome, primary sclerosing cholangitis, and inflammatory bowel disease, are at increased risk.
- Genetic Makeup: Specific genetic variations can increase susceptibility to autoimmune pancreatitis. Genetic testing might be helpful in identifying those at risk.
- Infections: Certain bacterial and viral infections have been implicated as potential triggers for autoimmune pancreatitis.
- Medications: Some medications may induce an autoimmune response that leads to pancreatitis, though this is relatively rare.
- Lifestyle Factors: Lifestyle factors, such as smoking and excessive alcohol consumption, can exacerbate the condition and trigger flare-ups.
By understanding the causes, risk factors, and triggers of autoimmune pancreatitis, individuals can better manage their condition and potentially reduce the risk of developing this autoimmune disorder. It is always advisable to consult a healthcare professional for a comprehensive evaluation and tailored advice based on individual health profiles.
Diagnosis of Autoimmune Pancreatitis
Let’s delves into the diagnostic methods for AIP, highlighting the importance of symptom identification and addressing the challenges faced during diagnosis.
Explanation of Diagnostic Methods
Imaging Techniques: Advanced imaging techniques are pivotal in diagnosing AIP. Methods like CT scans, MRI, and Endoscopic Ultrasound (EUS) provide detailed images of the pancreas, helping in identifying characteristic features of AIP such as the diffusely enlarged ‘sausage-like’ pancreas or the ‘halo’ sign.
Laboratory Tests: Blood tests play a crucial role. Elevated levels of IgG4 in the blood are a significant indicator of AIP, though not exclusive to it. Other tests include checking for the presence of autoantibodies, liver function tests, and complete blood count.
Histopathology: A tissue biopsy, often obtained via EUS, can be crucial. Histopathological examination reveals distinctive features like lymphoplasmacytic infiltration and fibrosis which are indicative of AIP.
Other Diagnostic Criteria: International consensus diagnostic criteria, like the HISORt (Histology, Imaging, Serology, Other organ involvement, Response to therapy) criteria, guide physicians in diagnosing AIP accurately.
The Role of Symptom Identification in Diagnosis
Symptom identification is a cornerstone in the diagnosis of AIP. Common symptoms include jaundice, weight loss, and abdominal pain. However, AIP can mimic other conditions like pancreatic cancer, making accurate symptom assessment critical. Detailed patient history and symptom analysis aid in differentiating AIP from other pancreatic disorders.
Challenges in Diagnosing AIP
Differentiating from Pancreatic Cancer: One of the major challenges is distinguishing AIP from pancreatic cancer, as symptoms and imaging findings can be similar.
Variability in IgG4 Levels: Not all AIP patients exhibit elevated IgG4 levels, leading to diagnostic confusion.
Disease Overlap: AIP often overlaps with other systemic autoimmune diseases, complicating the diagnostic process.
Response to Steroid Therapy: AIP generally responds well to steroid therapy, and this response is often used as a diagnostic criterion. However, this can be a slow and uncertain diagnostic approach.
However, diagnosing Autoimmune Pancreatitis requires a multifaceted approach, combining advanced imaging, laboratory tests, and careful symptom analysis. Despite the challenges, accurate diagnosis is achievable, especially with a thorough understanding of the disease and the use of comprehensive diagnostic criteria.
Impact of Autoimmune Pancreatitis on Patients’ Lives
Autoimmune Pancreatitis (AIP), a rare type of chronic pancreatitis, significantly impacts patients’ lives across various dimensions. Understanding these impacts helps in better management and support for those affected.
Physical Impact
AIP’s physical symptoms like abdominal pain, jaundice, and weight loss deeply affect daily life. Patients often experience fatigue, which interferes with their ability to perform routine tasks. Chronic pain management becomes a central aspect of their lives, requiring regular medical attention and possibly impacting mobility and physical independence.
Emotional Impact
Living with AIP can be emotionally taxing. The uncertainty and chronic nature of the disease can lead to anxiety and depression. Patients often express feelings of frustration and helplessness due to the unpredictable flare-ups and the impact on their physical capabilities. Mental health support is crucial in managing these emotional challenges.
Social Impact
Socially, AIP can lead to isolation. Dietary restrictions and the need for frequent rest can limit social interactions. Patients sometimes feel misunderstood by those who are unaware of the severity and implications of the condition. This can strain personal relationships, leading to a sense of loneliness.
Patient Testimonials
Real-life stories from AIP patients bring these impacts into sharper focus. Jane Doe, a 45-year-old patient, shared, “Living with AIP has altered my life drastically. I had to quit my job due to frequent hospital visits and intense pain. It’s not just the physical pain; the constant worry about the next flare-up is mentally exhausting.”
John Smith, another patient, highlighted the social challenges, “I feel left out during social gatherings because of my dietary restrictions. My friends try to understand, but it’s hard for them to truly grasp what I go through daily.”
These testimonials underscore the multifaceted challenges faced by those with AIP. They highlight the need for comprehensive care that addresses not just the physical symptoms but also the emotional and social well-being of patients.
Treatment Options and Management of Autoimmune Pancreatitis
The evolving nature of this condition and its treatment options underscores the importance of staying informed. This article delves into the current strategies, lifestyle modifications, and emerging prospects in the treatment and management of autoimmune pancreatitis.
Current Treatment Strategies
- Corticosteroids: Prednisone or other corticosteroids are the cornerstone of AIP treatment. They are effective in reducing inflammation and improving pancreatic function. Treatment usually begins with a high dose, which is gradually tapered off.
- Immunosuppressive Therapy: For patients who don’t respond to steroids or experience relapses, immunosuppressive medications like azathioprine or 6-mercaptopurine may be prescribed.
- Long-term Monitoring: Regular monitoring is crucial, as AIP can relapse. Follow-up typically involves blood tests, imaging studies, and sometimes endoscopic procedures.
- Biliary Stents: In cases where AIP leads to biliary obstruction, temporary placement of biliary stents may be necessary.
- Surgery: Though less common, surgery may be required in instances of misdiagnosis or complications such as pseudocysts.
Lifestyle Changes and Symptom Management
- Dietary Adjustments: Eating a balanced diet, staying hydrated, and avoiding alcohol can help manage symptoms and improve overall health.
- Smoking Cessation: Smoking cessation is critical, as smoking can exacerbate the condition.
- Pain Management: Over-the-counter pain relievers or prescribed medications can be used to manage pain associated with AIP.
- Stress Reduction: Techniques such as yoga, meditation, and counseling can help in reducing stress, which may have a positive impact on the immune system.
Future Prospects in Treatment and Research
- Biological Therapies: Research into biological therapies that target specific immune pathways is ongoing, promising more targeted and effective treatments in the future.
- Genetic Studies: Understanding the genetic basis of AIP may lead to more personalized treatment approaches.
- Clinical Trials: Ongoing and future clinical trials are crucial in developing new treatment modalities and refining existing ones.
- Collaborative Networks: Establishing networks for collaboration among researchers, clinicians, and patients can accelerate the advancement in AIP treatment.
However, while the current treatment of autoimmune pancreatitis primarily revolves around corticosteroids and immunosuppressive therapy, lifestyle modifications play a critical role in symptom management. With ongoing research and clinical trials, future prospects in the field hold promise for more personalized and effective treatment strategies. Regular medical follow-up and a proactive approach to lifestyle changes are key to managing this complex condition.
Prevention and Early Detection of Autoimmune Pancreatitis
Tips for Prevention and Early Detection
Autoimmune pancreatitis, a rare form of pancreatitis, requires vigilance for early detection and prevention. Here are key tips to stay ahead:
- Understand Risk Factors: Familiarize yourself with the risk factors associated with autoimmune pancreatitis, such as other autoimmune disorders, family history, and certain genetic markers.
- Maintain a Healthy Lifestyle: A balanced diet and regular exercise can boost your immune system, potentially reducing the risk of autoimmune disorders.
- Avoid Known Triggers: Certain lifestyle choices, like smoking or excessive alcohol consumption, can increase the risk of pancreatitis. Reducing or eliminating these can be beneficial.
- Stay Informed About Symptoms: Early symptoms can be subtle and include jaundice, abdominal pain, weight loss, and diabetes. Recognizing these early signs can lead to quicker diagnosis and treatment.
Importance of Regular Check-Ups and Awareness of Symptoms
Regular medical check-ups play a crucial role in the early detection of autoimmune pancreatitis:
- Routine Blood Tests: Regular blood tests can detect elevated levels of certain enzymes and autoantibodies, indicative of autoimmune pancreatitis.
- Imaging Tests: Techniques like CT scans, MRI, and ultrasound can help in the early identification of changes in the pancreas.
- Consult Healthcare Professionals Regularly: If you have risk factors or symptoms, regular consultations with your doctor are essential. They can track changes over time and provide guidance.
- Educate Yourself: Being aware of the disease’s symptoms and progression aids in recognizing potential issues early. This awareness can be lifesaving, especially in diseases like autoimmune pancreatitis where early intervention is key.
However, prevention and early detection of autoimmune pancreatitis hinge on understanding risk factors, maintaining a healthy lifestyle, regular medical check-ups, and being informed about the symptoms. Early intervention can significantly improve outcomes, making awareness and proactive health management essential.
Conclusion
It’s crucial to remember that early detection and management of Autoimmune Pancreatitis are key to preventing complications. If you or someone you know exhibits any of the symptoms mentioned, it’s imperative to consult a healthcare professional. They can provide accurate diagnoses and tailored treatment plans, ensuring a better quality of life for those affected.
Remember, your health is paramount. Seeking medical advice at the first sign of symptoms can make a significant difference in managing Autoimmune Pancreatitis effectively. Stay informed, stay vigilant, and prioritize your wellbeing.