Autoimmune Pancreatitis Treatment: Autoimmune pancreatitis (AIP) is a unique form of pancreatitis characterized by its autoimmune nature.
Unlike other forms of pancreatitis, AIP involves the body’s immune system mistakenly attacking the pancreas, leading to inflammation and a host of complications.
It’s essential to distinguish AIP from other pancreatic disorders for accurate treatment and management.
What is Autoimmune Pancreatitis?
Autoimmune Pancreatitis (AIP) is a unique form of pancreatitis distinguished by its autoimmune origin. Unlike other types of pancreatitis typically caused by alcohol abuse or gallstones, AIP is characterized by the immune system mistakenly attacking the pancreas. This rare condition often mimics cancer, leading to misdiagnoses. AIP falls into two categories: Type 1, linked to IgG4-related disease, and Type 2, which is not IgG4-related and often associated with inflammatory bowel disease.
Differentiating AIP from Other Types of Pancreatitis
Distinguishing AIP from other forms of pancreatitis is crucial for proper treatment. AIP typically presents with a benign course, often responding well to steroid therapy, unlike other types, where such treatment is ineffective. Key differences include:
- Symptoms: AIP often lacks the severe abdominal pain characteristic of acute pancreatitis.
- Imaging: Specific features on CT or MRI scans can help differentiate AIP from pancreatic cancer or other types of pancreatitis.
- Serology: Elevated levels of IgG4 in blood tests are indicative of AIP, particularly Type 1.
- Histopathology: Biopsy results showing lymphoplasmacytic infiltration support an AIP diagnosis.
Epidemiology and Risk Factors
AIP, while rare, affects both men and women, with a higher prevalence in males and in individuals aged 50 and above. The exact cause of AIP is unknown, but several risk factors have been identified:
- Genetics: There’s a suggested genetic predisposition to AIP.
- Autoimmune Conditions: Coexistence with other autoimmune diseases is common.
- Geographical Variation: Some studies indicate higher occurrences in Asian countries.
Understanding AIP’s unique characteristics, diagnostic criteria, and associated risk factors is essential for healthcare professionals and patients alike. Early and accurate diagnosis is key to managing AIP effectively, ensuring appropriate treatment and preventing unnecessary interventions.
Symptoms of Autoimmune Pancreatitis (AIP)
Understanding its symptoms is crucial for prompt diagnosis and effective management. This article will delve into the common symptoms associated with AIP and how these symptoms differ from other pancreatic disorders.
Common Symptoms of Autoimmune Pancreatitis
- Jaundice: A prominent symptom of AIP is jaundice, characterized by a yellowing of the skin and eyes. This occurs due to the blockage of bile ducts by the inflamed pancreas.
- Abdominal Pain: While less common than in other forms of pancreatitis, some patients may experience mild to moderate abdominal pain.
- Weight Loss: Unintentional weight loss is often reported in AIP cases, likely due to decreased appetite and malabsorption of nutrients.
- Steatorrhea: This refers to fatty stools, which occur when the pancreas does not produce enough enzymes to properly digest fat.
- Diabetes Mellitus: AIP can affect the insulin-producing cells of the pancreas, leading to diabetes.
Differentiating Symptoms from Other Pancreatic Disorders
While AIP shares some symptoms with other forms of pancreatitis, several distinctions are crucial:
- Nature of Abdominal Pain: Unlike acute pancreatitis, where pain is severe and sudden, AIP often presents with mild or even no abdominal pain.
- Onset of Symptoms: AIP symptoms typically develop more gradually compared to the abrupt onset seen in acute pancreatitis.
- Autoimmune Markers: AIP is often associated with elevated levels of IgG4, a type of antibody, and can coexist with other autoimmune disorders, which is not a characteristic of other pancreatic diseases.
- Response to Steroids: AIP usually responds well to steroid therapy, a response not seen in other types of pancreatic disorders.
- Imaging Differences: Radiological findings in AIP, such as diffuse enlargement of the pancreas and a ‘sausage-like’ appearance, are distinct from other pancreatic diseases.
However, while AIP shares some commonalities with other pancreatic conditions, its unique symptoms and response to treatment set it apart. Early recognition and differentiation from other pancreatic disorders are vital for appropriate management and improved outcomes.
Diagnosing Autoimmune Pancreatitis
Let’s delves into the diagnostic criteria for autoimmune pancreatitis, the importance of imaging tests and lab work in its diagnosis, and the role of biopsy in confirming the condition.
Diagnostic Criteria for Autoimmune Pancreatitis
The diagnosis of autoimmune pancreatitis hinges on a combination of clinical, imaging, serologic, and histologic criteria. These criteria have been refined over time to enhance accuracy. They typically include:
- Clinical Presentation: AIP often presents with jaundice and occasionally with abdominal pain. However, its symptoms can mimic those of pancreatic cancer, making clinical evaluation crucial.
- Serological Markers: Elevated levels of IgG4 in the blood are suggestive of AIP, though not definitive.
- Imaging Features: Characteristic findings on CT, MRI, or endoscopic ultrasound, such as a diffusely enlarged pancreas with a ‘sausage-like’ appearance, are indicative of AIP.
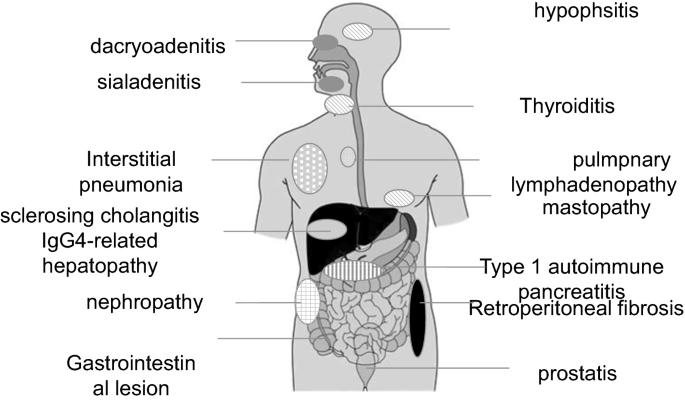
- Other Organ Involvement: AIP can be part of a systemic IgG4-related disease, affecting other organs like the bile ducts, kidneys, or salivary glands.
Imaging Tests and Lab Work in Diagnosis
Imaging tests play a pivotal role in diagnosing AIP. They not only help in identifying characteristic changes in the pancreas but also in ruling out other conditions like pancreatic cancer. Common imaging modalities include:
- CT Scan: Provides detailed images of the pancreas and surrounding tissues.
- MRI and MRCP (Magnetic Resonance Cholangiopancreatography): Offers high-resolution images of pancreatic ducts and structures.
- Endoscopic Ultrasound (EUS): Helps in examining the pancreas up close and in performing biopsies if needed.
Lab work complements imaging. Key tests include:
- Blood Tests: To check for elevated IgG4 levels and other markers of inflammation.
- Function Tests: To assess pancreatic function and detect abnormalities.
The Role of Biopsy in Confirming Autoimmune Pancreatitis
While imaging and lab tests are invaluable, a biopsy is often the definitive test for diagnosing AIP. It involves examining a small tissue sample from the pancreas. Biopsy findings that support the diagnosis of AIP include:
- Lymphoplasmacytic Infiltration: Dense infiltration by lymphocytes and plasma cells.
- Fibrosis: A characteristic pattern of fibrosis known as storiform fibrosis.
- IgG4-Positive Cells: An increased number of IgG4-positive plasma cells.
However, diagnosing autoimmune pancreatitis requires a comprehensive approach that includes a thorough assessment of clinical symptoms, imaging studies, laboratory tests, and often, a biopsy. This multifaceted approach ensures an accurate diagnosis, differentiating AIP from other pancreatic disorders and guiding appropriate treatment.
Autoimmune Pancreatitis Treatment
This complex condition requires a nuanced approach to treatment, one that addresses both the underlying autoimmune response and the resultant inflammation of the pancreas.
General Approach to Treating AIP
- Corticosteroids: The frontline treatment for AIP is typically corticosteroids, such as prednisone. These powerful anti-inflammatory drugs can help reduce inflammation and improve pancreatic function.
- Immunosuppressants: For cases where corticosteroids are ineffective or for long-term management, immunosuppressants may be used. These drugs help in regulating the immune system’s activity.
- Pain Management: Managing abdominal pain, a common symptom of AIP, is crucial. This can involve a combination of prescription pain medications and lifestyle modifications.
- Dietary Changes: A tailored diet, often developed with a nutritionist, can help manage symptoms and improve overall pancreatic health.
- Regular Monitoring: Regular check-ups and imaging tests are essential to monitor the progress of treatment and adjust it as necessary.
Importance of a Tailored Treatment Plan
Every patient’s experience with AIP is unique, necessitating a personalized treatment plan. Factors like the severity of the disease, the presence of other autoimmune disorders, and individual patient responses to medication all play a role in shaping this plan. Collaboration between gastroenterologists, immunologists, and nutritionists is often required to create an effective, comprehensive treatment strategy.
Key Takeaways
- AIP treatment primarily involves corticosteroids and, in some cases, immunosuppressants.
- Pain management and dietary changes are crucial aspects of treatment.
- Regular monitoring is essential to adapt the treatment plan as needed.
- A tailored approach, considering individual patient needs and responses, is fundamental for effective treatment.
Meanwhile, this tailored approach not only helps in managing the symptoms effectively but also plays a vital role in improving the quality of life for those suffering from AIP. With the right treatment plan, many patients can lead a normal, healthy life.
Medical Management of Autoimmune Pancreatitis
Let’s now delves into the most effective strategies for managing this condition, with a focus on first-line treatments, supplementary medications, and critical aspects of patient care such as side effect management and treatment monitoring.
First-Line Treatment Options: Corticosteroids
Corticosteroids stand as the cornerstone in the medical management of Autoimmune Pancreatitis. Prednisone or prednisolone are typically employed, recognized for their potent anti-inflammatory properties. These drugs have shown remarkable effectiveness in reducing pancreatic inflammation, thereby alleviating symptoms and preventing complications. Patients often experience significant improvement in clinical symptoms and imaging findings within weeks of starting corticosteroid therapy.
Effectiveness of Corticosteroids: Studies highlight that corticosteroids not only improve symptoms but also aid in normalizing laboratory abnormalities and imaging results associated with Autoimmune Pancreatitis. This makes them not just symptom relievers but disease-modifying agents. However, it’s crucial for healthcare providers to tailor the dosage and duration of treatment to each patient’s specific needs, balancing efficacy with potential side effects.
Other Medications Used in Treatment
While corticosteroids are effective, some cases may require additional medications. These include:
- Immunomodulators: Drugs like azathioprine and 6-mercaptopurine can be used, especially in steroid-resistant cases or to maintain remission.
- Biological Agents: For patients who don’t respond well to steroids and traditional immunomodulators, newer biological agents offer a promising alternative.
- Biliary Acid Sequestrants: These are used to manage associated symptoms like jaundice.
Managing Side Effects and Monitoring Treatment Response
Managing the side effects of medication is a critical aspect of treatment. Corticosteroids, while effective, can cause a range of side effects including weight gain, increased blood sugar, and bone density loss. Regular monitoring through blood tests, bone density scans, and frequent clinical evaluations is essential.
Monitoring Treatment Response: Regular follow-ups, including laboratory tests and imaging studies, help in assessing the response to treatment and in making necessary adjustments to the therapy. This continuous monitoring helps in early detection of any relapse and ensures timely intervention, thereby optimizing patient outcomes.
However, the medical management of Autoimmune Pancreatitis hinges on a well-orchestrated plan involving first-line corticosteroid therapy, the potential use of additional medications, and meticulous monitoring of treatment response and side effects. This comprehensive approach ensures the best possible outcomes for patients battling this challenging condition.
Dietary and Lifestyle Modifications for Autoimmune Pancreatitis (AIP)
Diet Recommendations for AIP Patients
1. Anti-Inflammatory Foods: Emphasize the intake of anti-inflammatory foods in your diet. This includes fruits, vegetables, whole grains, lean proteins, and healthy fats. Foods like berries, leafy greens, nuts, and olive oil are particularly beneficial.
2. Omega-3 Fatty Acids: Include foods rich in Omega-3 fatty acids, such as fatty fish (salmon, mackerel, and sardines), flaxseeds, and walnuts. These help in reducing inflammation.
3. Avoid Processed Foods: Minimize the consumption of processed and fried foods, as they can exacerbate inflammation. Also, limit foods high in sugar and salt.
4. Hydration: Stay well-hydrated. Drinking plenty of water helps in maintaining overall health and aids digestion.
5. Tailored Diet Plans: Consider working with a nutritionist to develop a diet plan that suits your specific needs, as individual responses to certain foods may vary.
Lifestyle Changes to Manage AIP Symptoms
1. Regular Exercise: Engage in regular, moderate exercise. Activities like walking, swimming, or yoga can help reduce stress, improve physical function, and boost your mood.
2. Stress Management: Stress can trigger or worsen symptoms. Practice stress-reducing techniques like meditation, deep breathing exercises, or mindfulness.
3. Adequate Sleep: Ensure you get sufficient, quality sleep. Poor sleep can exacerbate symptoms of AIP.
4. Avoid Smoking and Limit Alcohol: Smoking and excessive alcohol consumption can worsen autoimmune conditions. It’s best to avoid or limit these habits.
5. Regular Medical Check-ups: Stay in regular contact with your healthcare provider. Regular check-ups can help in effectively monitoring and managing your condition.
6. Join Support Groups: Consider joining a support group for individuals with autoimmune pancreatitis. Sharing experiences and tips can be both informative and emotionally supportive.
Remember, these dietary and lifestyle changes should complement your medical treatment. Always consult your healthcare provider before making significant changes to your diet or lifestyle.
Surgical Interventions in Autoimmune Pancreatitis
Indications for Surgical Intervention
The decision to proceed with surgery is typically based on specific indications, which include:
- Diagnostic Uncertainty: When imaging and laboratory tests fail to conclusively differentiate autoimmune pancreatitis from pancreatic cancer, surgery may be warranted for definitive diagnosis.
- Symptom Management: In cases where conservative treatments are insufficient in managing pain or other debilitating symptoms, surgery becomes a viable option.
- Complications: Surgical intervention may be required to address complications such as biliary or gastric obstruction, which are not uncommon in advanced stages of the disease.
Understanding these indications is crucial for timely and effective treatment, ensuring better patient outcomes.
Types of Surgical Procedures and Their Outcomes
Several surgical techniques can be employed in the treatment of autoimmune pancreatitis, each with its specific outcomes:
- Whipple Procedure (Pancreaticoduodenectomy): This complex surgery involves the removal of the head of the pancreas, part of the small intestine, the gallbladder, and the bile duct. While it’s a major operation, it can be highly effective in alleviating symptoms and resolving complications.
- Distal Pancreatectomy: In cases where the disease is localized to the tail of the pancreas, a distal pancreatectomy may be performed. This procedure involves the removal of the tail and, at times, a portion of the body of the pancreas.
- Total Pancreatectomy: This involves the removal of the entire pancreas and is generally reserved for severe, diffuse cases. It is a definitive solution but leads to lifelong diabetes and requires enzyme replacement therapy.
- Drainage Procedures: These are less invasive and focus on relieving obstructions, thereby alleviating symptoms like jaundice and gastric obstruction.
Each of these procedures has distinct outcomes and potential complications. The Whipple procedure, while effective, comes with a significant recovery period and risk of complications. Distal and total pancreatectomies also have substantial impacts on the patient’s quality of life due to ensuing diabetes and digestive issues. Drainage procedures, while less invasive, may offer temporary relief but do not address the underlying pancreatic inflammation.
However, surgical intervention in autoimmune pancreatitis is a critical component of treatment, especially when other therapies fail or in the presence of complex complications. Understanding the types of surgeries and their specific outcomes is essential for both healthcare providers and patients in making informed decisions about care.
Long-Term Management and Follow-Up of Autoimmune Pancreatitis
Regular monitoring is essential for maintaining health and preventing the progression of the disease.
Key Strategies for Monitoring
- Routine Blood Tests: Regular blood tests can track inflammation markers and liver function, which are crucial in detecting relapse.
- Imaging Studies: Imaging techniques like CT scans, MRI, and ultrasound help in assessing the pancreas’s condition and spotting any changes.
- Symptom Tracking: Patients should be aware of symptoms like jaundice, abdominal pain, and weight loss, which may indicate a relapse.
Ongoing Care and Lifestyle Management
Integrating Lifestyle Changes
Managing AIP isn’t just about medication; it involves comprehensive lifestyle changes. These include:
- Dietary Adjustments: A balanced diet, low in fats and rich in nutrients, helps manage symptoms and maintain overall health.
- Avoiding Alcohol and Smoking: Alcohol and smoking can exacerbate AIP symptoms and should be avoided.
- Regular Exercise: Moderate exercise can improve overall health and well-being.
The Role of Continuous Medical Care
- Regular Doctor Visits: Regular check-ups with a gastroenterologist are essential for adjusting treatment plans as needed.
- Education and Support: Patients should be educated about their condition and have access to support groups for better disease management.
Long-term management of autoimmune pancreatitis is a multi-faceted approach that requires both medical and lifestyle considerations. Regular monitoring, lifestyle changes, and continuous medical care form the pillars of effective long-term management, ensuring that patients with AIP can lead healthy, fulfilling lives.
Emerging Treatments and Research in Autoimmune Pancreatitis (AIP)
Recent Advancements in AIP Treatment
Autoimmune Pancreatitis (AIP), a complex medical condition characterized by the inflammation of the pancreas due to immune system activity, has seen significant progress in treatment methods. The recent advancements in AIP treatment focus on more effective and targeted approaches. Steroids, traditionally the first line of treatment, are now being supplemented with other immunosuppressive medications. This allows for better management of symptoms and minimizes long-term side effects.
Newer therapies are also emerging, such as biologic agents, which are designed to target specific parts of the immune system. These treatments have shown promise in reducing inflammation more effectively than general immunosuppressants. Additionally, advancements in diagnostic techniques have made it easier to differentiate AIP from other types of pancreatic disorders, leading to more accurate and timely treatment.
Ongoing Research and Future Prospects
The future of AIP treatment is bright, with ongoing research paving the way for more innovative approaches. One area of research focuses on understanding the genetic and environmental factors that contribute to the development of AIP. This could lead to personalized medicine approaches, where treatment is tailored to the individual’s specific genetic makeup.
Another promising area is the development of new biomarkers. Biomarkers are biological indicators that can help diagnose diseases more accurately and monitor the effectiveness of treatments. The discovery of new biomarkers for AIP could lead to quicker diagnosis and more efficient tracking of the disease progression and response to treatment.
Furthermore, clinical trials are underway to test new medications and therapy combinations. These trials aim to find more effective treatment regimens with fewer side effects, improving the quality of life for patients with AIP.
However, the landscape of AIP treatment and research is rapidly evolving. With continued advancements and a deeper understanding of the disease, there is hope for more effective and personalized treatments in the near future. This makes it an exciting time in the field of autoimmune pancreatitis research and treatment.
Patient Support and Resources for Autoimmune Pancreatitis
This article also aims to guide individuals affected by AIP towards effective support systems and highlight the importance of psychological support in managing chronic illnesses like autoimmune pancreatitis.
Support Groups and Resources for Patients and Caregivers
- Local and Online Support Groups: Joining support groups can be incredibly beneficial. These groups provide a platform for sharing experiences, offering practical advice, and receiving emotional support. Look for local chapters or online forums dedicated to autoimmune pancreatitis or broader autoimmune conditions.
- Educational Resources: Educating yourself about AIP is vital. Reliable sources like healthcare providers, reputable medical websites, and patient advocacy organizations offer valuable information about the disease, treatment options, and lifestyle management.
- Professional Counseling Services: Living with a chronic condition can be overwhelming. Professional counseling can help patients and caregivers cope with the emotional and psychological challenges of AIP. These services can be accessed through healthcare providers, community health centers, or mental health organizations.
- Nutritional Guidance: AIP can affect nutritional needs. Dietitians specializing in autoimmune diseases can provide personalized dietary plans that cater to the unique needs of AIP patients.
- Physical Activity Programs: Regular physical activity is important for overall health. Programs tailored for individuals with chronic conditions can help maintain physical fitness without exacerbating symptoms.
Importance of Psychological Support in Chronic Illness Management
- Enhancing Quality of Life: Psychological support helps in managing stress, anxiety, and depression, which are common in chronic illness. This support can significantly improve the quality of life for AIP patients.
- Coping Strategies: Learning coping strategies through psychological support can empower patients to handle the challenges of living with a chronic condition, leading to better disease management and a more positive outlook.
- Family and Caregiver Support: Chronic illnesses affect not just the patient but also their family and caregivers. Psychological support can provide these individuals with the tools they need to support their loved ones effectively.
- Community Connection: Engaging with a community that understands the challenges of living with AIP can reduce feelings of isolation and promote a sense of belonging.
However, accessing patient support and resources is a critical aspect of managing autoimmune pancreatitis. Support groups, educational materials, professional counseling, nutritional guidance, and physical activity programs are invaluable resources. Furthermore, psychological support plays a pivotal role in enhancing the quality of life for patients and their caregivers, providing them with essential coping mechanisms and a supportive community.
Conclusion
Autoimmune pancreatitis, though rare, is a distinct type of pancreatitis that requires a specialized approach for diagnosis and treatment. With the right combination of diagnostic techniques and treatment strategies, patients with AIP can achieve remission and maintain a good quality of life.
For more detailed information on autoimmune pancreatitis, its diagnosis, treatment, and long-term management, visit reputable medical resources and support groups. These platforms offer valuable insights and support for individuals affected by AIP.