Aspergillosis Symptoms: Aspergillosis is a condition triggered by Aspergillus, a common mold (fungus) that lives indoors and outdoors.
While most people breathe in Aspergillus spores without getting sick, those with weakened immune systems or lung diseases are at a higher risk of developing health problems due to this mold.
What is Aspergillosis?
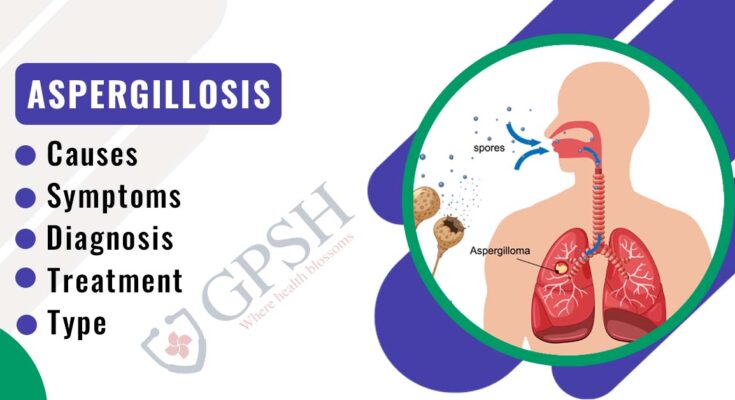
Aspergillosis is a condition caused by Aspergillus, a common mold (fungus) that lives indoors and outdoors. Most people breathe in Aspergillus spores every day without getting sick. However, people with weakened immune systems or lung diseases are at a higher risk of developing health problems due to Aspergillosis. The condition can manifest in various forms, ranging from allergic reactions to lung infections and even systemic infections that can affect multiple organs.
Types of Aspergillosis
There are several types of Aspergillosis, each with distinct features:
- Allergic Bronchopulmonary Aspergillosis (ABPA): This allergic reaction occurs mostly in people with asthma or cystic fibrosis. It leads to inflammation in the lungs and allergy symptoms.
- Aspergilloma (Fungal Ball): This form involves the growth of a fungal ball in the lungs, often in pre-existing cavities like those caused by tuberculosis.
- Chronic Pulmonary Aspergillosis: A long-lasting condition that may present with weight loss, coughing, and fatigue, often occurring in people with pre-existing lung conditions.
- Invasive Aspergillosis: The most severe form, it occurs when the infection spreads from the lungs to other parts of the body. This is a serious condition, particularly in people with severely weakened immune systems.
Statistical Data on Prevalence and Risk Factors
Aspergillosis is relatively rare in healthy individuals. However, its prevalence is higher among people with compromised immune systems, such as those undergoing chemotherapy, people living with HIV/AIDS, or those who have had organ transplants. According to the Centers for Disease Control and Prevention (CDC), the exact number of Aspergillosis cases is difficult to determine as it is not a reportable condition in many places. However, studies suggest that invasive aspergillosis can occur in up to 13-24% of leukemia patients and 5-25% of bone marrow transplant recipients. Risk factors include prolonged neutropenia, corticosteroid therapy, and lung diseases.
By understanding Aspergillosis, its types, prevalence, and risk factors, individuals and healthcare providers can better prepare for and manage this condition. Awareness is key to prevention, especially for those at higher risk due to their health status.
Symptoms of Aspergillosis
Below, we provide a detailed list of common symptoms, compare symptoms across different types of Aspergillosis, and share real-life case studies to illustrate these signs.
Common Symptoms of Aspergillosis
Aspergillosis can present a range of symptoms, depending on the type and severity of the infection. Commonly observed symptoms include:
- Respiratory Issues: Persistent cough, wheezing, and shortness of breath are typical signs.
- Fever: A low-grade fever can accompany other symptoms, particularly in invasive cases.
- Fatigue and Weakness: General malaise and tiredness are often reported by patients.
- Allergic Reactions: Symptoms like nasal congestion and itchy eyes may indicate an allergic response to Aspergillus.
- Chest Pain and Hemoptysis: In severe cases, chest pain and coughing up blood can occur.
Comparing Symptoms in Different Types of Aspergillosis
The symptoms of Aspergillosis can vary significantly based on the type of infection:
- Allergic Bronchopulmonary Aspergillosis (ABPA): This type primarily affects individuals with asthma or cystic fibrosis, causing worsening asthma symptoms, coughing, and sometimes producing brownish mucus.
- Chronic Pulmonary Aspergillosis: Characterized by weight loss, fatigue, and chronic cough, often with blood.
- Invasive Aspergillosis: This severe form, usually affecting people with weakened immune systems, can cause fever, chest pain, and difficulty breathing. It may also spread to other organs, leading to a variety of symptoms.
Case Studies and Anecdotes
To better understand the impact of these symptoms, consider the following real-life scenarios:
- Case Study 1: A 45-year-old asthma patient, initially mistaking symptoms for an asthma exacerbation, was later diagnosed with ABPA after persistent worsening of respiratory symptoms.
- Case Study 2: An immunocompromised patient developed invasive Aspergillosis post-surgery, highlighting the importance of early symptom recognition and prompt treatment in vulnerable individuals.
Recognizing the signs of Aspergillosis and understanding its varied presentations can be lifesaving, especially for individuals with underlying health conditions. If you or someone you know is experiencing these symptoms, it’s essential to consult a healthcare provider for an accurate diagnosis and appropriate treatment plan.
Causes and Risk Factors for Aspergillosis
Understanding the causes and risk factors of Aspergillosis is essential for prevention and effective treatment.
How Aspergillosis is Caused
Aspergillosis occurs when you inhale microscopic Aspergillus spores. While most people breathe in these spores every day without getting sick, individuals with weakened immune systems or lung diseases are at a higher risk of developing Aspergillosis. The infection can manifest in various forms, from allergic reactions to lung infections and even systemic infections.
Environmental Risk Factors
The environment plays a significant role in Aspergillosis infections. Environments with abundant mold spores, like construction sites, compost piles, or areas with decaying vegetation, pose a higher risk. Poor ventilation or damp conditions can also increase mold growth indoors, elevating the risk of exposure.
Health Conditions as Risk Factors
Certain health conditions significantly increase the risk of Aspergillosis. These include:
- Chronic respiratory conditions like asthma or cystic fibrosis.
- Weakened immune systems due to conditions like leukemia or HIV/AIDS.
- Long-term corticosteroid use or immunosuppressive medication.
- Lung cavities from previous health issues.
Lifestyle Factors
Lifestyle choices can also impact the risk of Aspergillosis. Smoking, for instance, can damage the lungs and make them more susceptible to infections. Activities that expose individuals to dust and soil, such as gardening without proper protective gear, can also increase the risk.
Spread of Aspergillosis
Aspergillosis is not contagious and cannot spread from person to person or from animals to humans. The primary mode of infection is through inhaling spores from the environment. Understanding this is crucial in preventing the disease, especially for those at higher risk.
However, Aspergillosis is a mold-related infection primarily caused by the inhalation of Aspergillus spores. Risk factors range from environmental exposure and pre-existing health conditions to specific lifestyle choices. Awareness and prevention are key in managing the risks associated with this infection.
Diagnosing Aspergillosis: A Comprehensive Guide
Understanding the diagnostic methods, the role of symptoms, and the inherent challenges in diagnosing this condition is crucial for effective management and treatment.
Overview of Diagnostic Methods for Aspergillosis
1. Medical Imaging: Techniques like CT scans and chest X-rays are often the first step. These imaging methods help identify characteristic signs of Aspergillosis, such as lung cavities or nodules.
2. Laboratory Tests: Blood tests, sputum culture, and tissue biopsies can detect Aspergillus organisms. Blood tests may also identify specific antigens and antibodies related to this fungus.
3. Molecular Diagnostics: PCR (Polymerase Chain Reaction) testing is a more advanced technique that detects the genetic material of Aspergillus, providing a fast and sensitive diagnosis.
The Role of Symptoms in Diagnosing Aspergillosis
Symptoms play a critical role in prompting diagnostic investigation for Aspergillosis. Common symptoms include:
- Respiratory issues: such as coughing, wheezing, and shortness of breath.
- Allergic reactions: including allergic bronchopulmonary aspergillosis (ABPA), manifesting as asthma-like symptoms.
- Systemic signs: like fever, fatigue, and weight loss, especially in invasive aspergillosis.
Recognizing these symptoms early is key to timely diagnosis and treatment.
Challenges in Diagnosing Aspergillosis
Diagnosing Aspergillosis presents several challenges:
- Non-specific Symptoms: Many symptoms of Aspergillosis are similar to other respiratory conditions, leading to potential misdiagnosis.
- Variable Disease Forms: Aspergillosis can manifest in different forms, from allergic reactions to invasive diseases, complicating the diagnosis.
- Limited Awareness: Lack of awareness among both patients and healthcare providers can delay diagnosis.
- Reliance on Specialized Testing: Advanced diagnostic methods like PCR are not universally available, hindering prompt diagnosis in some settings.
Understanding these challenges is essential for healthcare providers to improve diagnostic accuracy and ensure effective management of Aspergillosis.
Treatment Options for Aspergillosis
Effective treatment requires a nuanced understanding of the available options and how they align with the varied manifestations of the infection. This article delves into the current treatment landscape for aspergillosis, shedding light on how symptoms influence treatment choices and providing real-world insights through case studies or patient testimonials.
Navigating the Treatment Options
- Antifungal Medications: The cornerstone of aspergillosis treatment is antifungal therapy. Medications such as voriconazole, itraconazole, and amphotericin B are commonly prescribed. These drugs work by inhibiting the growth of the Aspergillus fungi, helping to alleviate the infection.
- Surgical Interventions: In severe cases, particularly those involving invasive aspergillosis, surgical removal of the infected tissue may be necessary. This approach is often used when the infection has caused significant damage or is threatening vital organs.
- Adjunctive Therapies: Depending on the patient’s condition, additional treatments like corticosteroids to reduce inflammation or immunotherapy for patients with weakened immune systems may be employed.
Symptom-Driven Treatment Choices
The choice of treatment for aspergillosis largely hinges on the type and severity of symptoms:
- Allergic Reactions: Allergic forms of aspergillosis, such as allergic bronchopulmonary aspergillosis (ABPA), often require corticosteroids in addition to antifungal medications.
- Invasive Infections: In cases of invasive aspergillosis, aggressive antifungal therapy is the primary course of action.
- Localized Infections: For less severe, localized infections, oral antifungal medications may suffice.
Real-World Perspectives: Case Studies and Patient Testimonials
Incorporating case studies and patient testimonials offers invaluable insights into the real-world application of these treatments. These narratives not only highlight the efficacy of various treatment strategies but also underscore the importance of personalized care in managing aspergillosis.
- Case Study 1: A detailed account of a patient with invasive aspergillosis responding to a combination of surgical intervention and antifungal therapy.
- Patient Testimonial: First-hand experiences from patients managing ABPA with corticosteroids and lifestyle modifications.
Aspergillosis treatment is a dynamic field, with choices deeply influenced by the specific symptoms and severity of the infection. Understanding these options, coupled with insights from case studies and patient experiences, can guide patients and healthcare professionals in making informed decisions for effective management of this challenging condition.
Preventing Aspergillosis: Tips and Strategies
Preventive Measures for At-Risk Individuals
It’s crucial for at-risk individuals to adopt preventive strategies to minimize their exposure to these fungi. Here are some effective measures:
- Avoid Areas with High Dust and Soil Exposure: Since Aspergillus spores are commonly found in soil, dust, and decaying vegetation, it’s advisable to avoid activities that involve disturbing these materials, such as gardening or construction work.
- Maintain Indoor Air Quality: Use HEPA filters in your home, especially in bedrooms and living areas, to reduce the presence of fungal spores in the air. Regular maintenance of heating and air conditioning systems is also important.
- Personal Protective Equipment (PPE): In situations where exposure to dust or mold is unavoidable, wearing masks and protective clothing can provide a barrier against spores.
Role of Environment and Lifestyle in Prevention
The environment plays a significant role in the risk of Aspergillosis. Here are some lifestyle adjustments that can help:
- Humidity Control: Keep indoor humidity levels below 50% to inhibit the growth of molds and fungi.
- Cleanliness and Hygiene: Regular cleaning and vacuuming of living spaces can greatly reduce spore counts. Pay special attention to bathrooms and kitchens, where mold tends to thrive.
- Diet and Health Maintenance: A healthy diet and regular exercise can strengthen the immune system, offering additional protection against infections.
Expert Opinions and Recommendations
Healthcare professionals and researchers emphasize the importance of awareness and proactive measures in preventing Aspergillosis. They recommend:
- Regular Health Check-Ups: Especially for those with chronic lung conditions or weakened immune systems, regular medical check-ups can help in early detection and prevention.
- Educational Resources: Stay informed about Aspergillosis through reputable sources like the Centers for Disease Control and Prevention (CDC) and World Health Organization (WHO).
- Consultation with Specialists: If you’re at high risk, consulting with an infectious disease specialist or a pulmonologist can provide personalized advice and prevention strategies.
By integrating these tips and strategies into your daily life, you can significantly reduce your risk of Aspergillosis and maintain a healthier living environment.
Living with Aspergillosis: Managing Symptoms and Health
This article provides essential tips for managing symptoms, lifestyle adjustments for better health, and information about the support and resources available for patients.
Tips for Managing Symptoms
- Medication Adherence: Follow your healthcare provider’s instructions regarding medications. Antifungal medications are often prescribed and play a crucial role in controlling Aspergillosis symptoms.
- Regular Monitoring: Keep track of your symptoms and consult your doctor regularly. Early detection of any changes can help in timely intervention.
- Air Quality Control: Since Aspergillus spores are airborne, it’s vital to maintain good indoor air quality. Use air purifiers and reduce humidity in your home to minimize the presence of these spores.
- Avoid Exposure to Molds: Stay away from environments where you’re likely to encounter mold, such as construction sites, compost heaps, or decayed vegetation.
Lifestyle Adjustments for Better Health
- Balanced Diet: Incorporate a balanced diet rich in fruits, vegetables, and lean proteins to boost your immune system.
- Exercise Regularly: Engage in light to moderate exercise to enhance your respiratory function and overall health. Always consult with your doctor before starting any new exercise regimen.
- Stress Management: Practice stress-reduction techniques like meditation, yoga, or deep breathing exercises. Stress can exacerbate health issues, making symptom management more challenging.
- Adequate Rest: Ensure you get enough sleep. Rest is crucial for your body to recover and fight infections.
Support and Resources for Patients
- Patient Support Groups: Joining support groups can provide emotional support and valuable information from others who are living with Aspergillosis.
- Educational Resources: Educate yourself about Aspergillosis through reliable sources. Understanding your condition can help you make informed decisions about your care.
- Professional Counseling: Consider professional counseling if you’re struggling to cope with your diagnosis. It can help you deal with the emotional and psychological aspects of living with a chronic condition.
- Consult Specialists: Regular consultations with specialists like pulmonologists or infectious disease experts can provide you with tailored advice and care.
However, while living with Aspergillosis can be challenging, adopting these management strategies can significantly improve your symptoms and overall quality of life. Remember, you are not alone, and there are numerous resources and support systems to help you navigate this journey.
FAQs About Aspergillosis Symptoms and Causes
1. What is Aspergillosis?
Aspergillosis is an infection caused by Aspergillus, a common mold found in the environment. It can cause various illnesses, from allergic reactions to lung infections and systemic diseases.
2. What are the common symptoms of Aspergillosis?
Symptoms vary depending on the type of Aspergillosis. Allergic forms may cause asthma-like symptoms, while invasive types can lead to fever, chest pain, cough, and breathlessness. Chronic forms can cause weight loss and fatigue.
3. Who is at risk of developing Aspergillosis?
Individuals with weakened immune systems, lung diseases, or those taking immunosuppressive medication are at higher risk. However, healthy individuals can also be affected by allergic forms of the disease.
4. How is Aspergillosis caused?
Aspergillosis is caused by inhaling Aspergillus spores. These spores are ubiquitous in the environment, found in soil, dust, and decaying vegetation.
5. Can Aspergillosis spread from person to person?
No, Aspergillosis is not contagious and cannot be spread from person to person. It results from environmental exposure to the mold.
6. Is there a treatment for Aspergillosis?
Yes, treatments are available, including antifungal medications. The choice of treatment depends on the type of Aspergillosis and the overall health of the patient.
7. How can Aspergillosis be prevented?
Preventive measures include avoiding environments with high levels of mold, such as compost heaps and construction sites, especially for those at higher risk.
8. Can Aspergillosis be cured?
The curability depends on the type of Aspergillosis and the patient’s health. While some forms can be effectively treated, others may require long-term management.
9. What are the long-term effects of Aspergillosis?
Chronic and invasive forms can lead to complications like lung damage and respiratory issues. Early detection and treatment are crucial for better outcomes.
10. Should I see a doctor if I suspect Aspergillosis?
Yes, if you experience symptoms, especially if you have an underlying health condition or a weakened immune system, consult a healthcare professional.
Conclusion
Finally, we cannot stress enough the importance of seeking medical advice if you experience any symptoms associated with Aspergillosis. Early medical intervention is key to effective treatment. It’s vital to consult healthcare professionals who can provide accurate diagnosis and appropriate treatment plans. Remember, self-diagnosis can be dangerous, and online resources should not replace professional medical advice.
In summary, awareness and vigilance are your best defenses against Aspergillosis. Stay informed, be attentive to your health, and seek medical guidance when necessary. Your health and well-being are paramount, and understanding Aspergillosis is a crucial step towards safeguarding them.