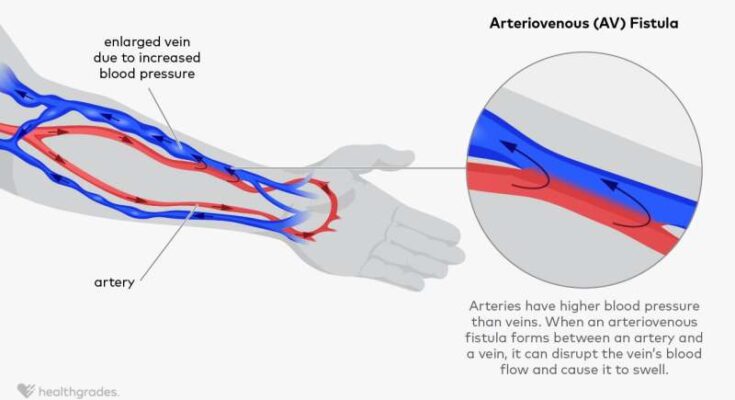
Arteriovenous Fistula Treatment: An Arteriovenous Fistula (AVF) is an abnormal connection between an artery and a vein. Normally, blood flows from your arteries to your capillaries and then to your veins.
However, in an AVF, blood flows directly from an artery into a vein, bypassing some capillaries. This condition can cause complications because of the high-pressure flow of blood from arteries directly into veins.
What is an Arteriovenous Fistula?
An arteriovenous fistula (AVF) is an abnormal connection between an artery and a vein. Normally, blood flows from your arteries to your capillaries and then to your veins. In an AVF, this natural course is bypassed as blood flows directly from an artery into a vein. This can cause a range of health issues due to the high-pressure arterial blood overwhelming the veins, which are not designed to handle such pressure. Understanding AVFs is crucial as they can impact blood circulation and overall vascular health.
Causes and Risk Factors
Arteriovenous fistulas can occur either congenitally or as a result of specific medical conditions or procedures. Factors that increase the risk of developing an AVF include:
- Genetic Conditions: Certain genetic disorders may predispose individuals to arteriovenous malformations, which can lead to the formation of fistulas.
- Trauma or Injury: Severe injuries that damage both arteries and veins can result in an AVF.
- Surgical Procedures: Some surgical interventions, particularly involving the arteries and veins, can accidentally create fistulas.
- Underlying Health Conditions: Diseases such as cirrhosis or conditions that weaken blood vessel walls can lead to the development of AVFs.
Types of Arteriovenous Fistula
Arteriovenous fistulas can be classified into several types, based on their nature and location:
- Congenital Fistulas: These are present at birth and result from developmental abnormalities in the vascular system.
- Acquired Fistulas: These develop later in life due to injuries, surgeries, or diseases.
- Dialysis Fistulas: Specifically created for hemodialysis in patients with renal failure, these fistulas connect an artery to a vein, usually in the arm, to facilitate efficient blood flow during dialysis.
Each type of AVF has its own set of implications and treatment approaches. Understanding the specific nature and location of an arteriovenous fistula is essential for effective management and treatment.
Signs and Symptoms of Arteriovenous Fistulas
These symptoms vary depending on the type and location of the fistula. Understanding these symptoms is crucial for early detection and treatment.
Common Symptoms Associated with Arteriovenous Fistulas
- Swelling and Pain: The most common symptom of an arteriovenous fistula is localized swelling. This swelling is often accompanied by pain or discomfort in the affected area.
- Abnormal Pulsation: Patients may feel a strong pulsation or throbbing near the site of the fistula.
- Reduction in Circulation: In some cases, an arteriovenous fistula can lead to reduced circulation in the affected limb, causing symptoms like coldness or numbness.
- Visible Veins: Enlarged, visible veins near the surface of the skin are also a telltale sign, especially in fistulas near the skin.
Symptoms Based on Type and Location
- Cerebral Arteriovenous Fistulas: These occur in the brain and can lead to headaches, seizures, or even stroke-like symptoms.
- Pulmonary Arteriovenous Fistulas: Located in the lungs, these fistulas might cause difficulty breathing, chest pain, or a bluish skin tone.
- Peripheral Arteriovenous Fistulas: Commonly found in limbs, these can result in swelling, pain, and changes in skin color.
When to Seek Medical Attention
- Persistent Pain or Swelling: If you notice unexplained swelling or pain that doesn’t subside, it’s important to consult a healthcare provider.
- Neurological Symptoms: Symptoms like seizures, sudden headaches, or weakness should prompt immediate medical attention, especially in cerebral arteriovenous fistulas.
- Changes in Skin Color or Temperature: Any significant change in the color or temperature of your skin near the fistula site warrants a medical evaluation.
However, being aware of the signs and symptoms of arteriovenous fistulas, especially as they vary by location and type, is key to prompt diagnosis and treatment. Early medical intervention can significantly improve outcomes for individuals with this condition. If you experience any of the symptoms mentioned, seeking medical advice is strongly recommended.
Diagnosis of Arteriovenous Fistula
Here, we will guide you through the diagnosis process, highlighting key steps and the importance of medical expertise in identifying AVF.
Initial Assessment and Medical History
The first step in diagnosing an arteriovenous fistula involves a thorough initial assessment and review of the patient’s medical history. It’s crucial to understand symptoms such as swelling, abnormal vein growth, or changes in skin color, which could indicate AVF. Additionally, knowing the patient’s history, including any previous surgeries or conditions like high blood pressure, can provide valuable insights for a precise diagnosis.
Diagnostic Tests and Imaging Techniques
- Ultrasound: A non-invasive and commonly used technique, ultrasound helps in visualizing blood flow, identifying abnormal connections between blood vessels.
- Magnetic Resonance Imaging (MRI): MRI offers detailed images of blood vessels and surrounding tissues, aiding in spotting irregularities caused by AVFs.
- Computed Tomography (CT) Scans: These scans provide cross-sectional images of the body and are effective in detecting AVFs and assessing their impact on nearby structures.
Each of these imaging techniques has its own advantages and can be used individually or in combination to confirm the presence of an arteriovenous fistula.
Role of Specialists in Diagnosis
The diagnosis of AVF often involves a team of specialists, including:
- Vascular Surgeons: Experts in blood vessel conditions, they play a key role in interpreting diagnostic tests and determining the best course of action.
- Radiologists: They specialize in reading and understanding imaging results, providing crucial information for the diagnosis.
- Cardiologists and Neurologists: Depending on the location of the AVF, these specialists may also be involved in the diagnosis process.
However, the diagnosis of an arteriovenous fistula involves a comprehensive approach, starting from patient history and physical examination, followed by specialized imaging techniques. The involvement of skilled specialists is essential for an accurate diagnosis, guiding the pathway to effective treatment.
Treatment Options for Arteriovenous Fistula
Managing an arteriovenous fistula (AVF), an abnormal connection between arteries and veins, requires a strategic approach. The primary goals of treatment include preventing complications, managing symptoms, and restoring normal blood flow. Understanding these objectives is crucial for both patients and healthcare providers in choosing the most effective treatment plan.
Exploring Non-Surgical Treatments
Non-surgical interventions play a vital role in managing arteriovenous fistulas, especially in their early stages or when surgery poses high risks. These treatments focus on reducing symptoms and slowing the progression of the condition. They include:
- Medication Management: Medications can help manage symptoms like pain and swelling. Blood thinners may be used to prevent clotting issues.
- Compression Therapy: Wearing compression garments can alleviate discomfort and swelling by improving blood flow.
- Lifestyle Adjustments: Changes in diet, exercise, and avoiding certain activities can significantly impact the management of AVF.
The effectiveness of these treatments varies based on the individual’s condition and the severity of the fistula. Regular monitoring and adjustments in the treatment plan are essential for achieving the best outcomes.
Surgical Options: Procedures and Techniques
When non-surgical methods are insufficient, surgery becomes a viable option. Surgical treatments for AVF aim to close or remove the abnormal connection and restore normal blood flow. Common surgical procedures include:
- Embolization: This minimally invasive procedure involves inserting a catheter into the blood vessel to block the abnormal connection using coils or other materials.
- Ligation: This involves tying off the blood vessels involved in the fistula to stop abnormal blood flow.
- Bypass Surgery: In more complex cases, a bypass may be created around the fistula to redirect blood flow.
Each surgical technique has its specific indications, risks, and benefits. The choice of procedure depends on the location, size, and complexity of the arteriovenous fistula, as well as the patient’s overall health.
Treatment options for arteriovenous fistula range from conservative non-surgical methods to more invasive surgical procedures. The choice of treatment should be tailored to the individual’s specific condition, considering the benefits and risks of each option. Ongoing follow-up and care are essential for managing this condition effectively.
Advanced Arteriovenous Fistula Treatments: Paving the Way for the Future
The medical community is constantly evolving, bringing forth innovative solutions to manage and treat these conditions more effectively. In this article, we explore the latest advancements in arteriovenous fistula care, focusing on emerging treatments, the increasing role of minimally invasive surgery, and the exciting prospects for future treatment methods.
Emerging Treatments and Technologies
The landscape of arteriovenous fistula treatment is rapidly changing, thanks to technological advancements. New therapies, guided by the latest research, are providing patients with more effective and less invasive options. These include novel drug therapies that aim to enhance vascular healing and reduce complications. Additionally, advancements in imaging technologies are allowing for more precise diagnosis and treatment planning, enabling personalized care tailored to each patient’s unique condition.
The Role of Minimally Invasive Surgery
Minimally invasive surgery has become a cornerstone in treating arteriovenous fistulas. These procedures, often performed using small incisions and advanced imaging techniques, minimize tissue damage and result in quicker recovery times compared to traditional surgery. Endovascular techniques, such as angioplasty and stenting, are increasingly being used to manage fistulas. These methods not only reduce the physical burden on patients but also improve the overall success rates of the treatments.
Future Prospects in Treatment Methods
The future of arteriovenous fistula treatment holds immense promise. Research is underway exploring the potential of regenerative medicine, including stem cell therapy, which could revolutionize the way these conditions are treated. Furthermore, the development of smart implants and biocompatible materials could lead to more durable and efficient treatment solutions. As technology advances, so does the hope for more effective and less invasive treatment options for patients with arteriovenous fistulas.
However, the field of arteriovenous fistula treatment is witnessing remarkable advancements. From emerging drug therapies and cutting-edge imaging techniques to minimally invasive surgical procedures and the promise of regenerative medicine, the future of this field is bright, offering new hope and improved outcomes for patients worldwide.
Living with an Arteriovenous Fistula
Living with an arteriovenous fistula (AVF) can be challenging, but with the right lifestyle adjustments, ongoing monitoring, and support systems, individuals can manage their condition effectively. Here’s a guide to help those affected by AVF navigate their daily lives with confidence and comfort.
Lifestyle Adjustments and Home Care
Adapting Daily Activities: It’s crucial for patients with an AVF to modify their daily activities to prevent complications. This includes avoiding heavy lifting and high-impact sports which can strain the fistula. Gentle exercises, however, are encouraged to promote blood flow.
Skin Care: Since the skin around an AVF can be sensitive, proper skin care is essential. This involves regular cleaning of the fistula area and using mild, non-irritating soaps. Any signs of infection or unusual changes should be reported to a healthcare provider immediately.
Diet and Nutrition: A heart-healthy diet benefits those with an AVF. This means low in sodium, rich in whole grains, fruits, and vegetables, and limited in saturated fats. Staying hydrated is also important, but fluid intake may need to be monitored in some cases.
Ongoing Monitoring and Follow-up Care
Regular Check-ups: Regular visits to a healthcare provider are crucial for monitoring the function and health of the fistula. These check-ups typically involve physical examinations and sometimes imaging tests to assess blood flow.
Self-monitoring Techniques: Patients are often advised to learn how to check their fistula for patency, which includes feeling for the “thrill” or vibration. Any changes in the sound or feel of the fistula should prompt an immediate consultation with a healthcare professional.
Support Systems and Resources for Patients
Support Groups: Joining a support group can provide emotional support and valuable information from others who are living with an AVF. These groups can be found both in-person and online.
Educational Resources: Many organizations offer educational materials and resources to help patients understand their condition better. These resources can include pamphlets, websites, and patient education sessions.
Mental Health Support: Living with a chronic condition like AVF can be mentally taxing. Seeking support from mental health professionals can be beneficial in managing stress, anxiety, or depression that might accompany this condition.
However, living with an arteriovenous fistula requires careful management, but with the right approach, patients can lead full and active lives. Emphasizing lifestyle adjustments, regular monitoring, and utilizing support resources are key steps in effectively managing an AVF.
Prevention and Risk Reduction for Arteriovenous Fistula
Effective prevention and risk reduction strategies are key to managing this health challenge. Understanding and implementing these strategies can significantly lower the risk of developing arteriovenous fistula or mitigate its severity.
Strategies for Prevention
The primary step in preventing arteriovenous fistula is awareness and proactive management of underlying health conditions. Here are some pivotal strategies:
- Maintain Healthy Blood Pressure Levels: Hypertension is a leading contributor to vascular complications. Regularly monitoring and maintaining blood pressure within recommended ranges is crucial.
- Control Blood Sugar Levels: For individuals with diabetes, meticulous control of blood sugar levels is essential. This helps in reducing the risk of vascular damage that can lead to arteriovenous fistula.
- Healthy Lifestyle Choices: Adopting a healthy lifestyle that includes a balanced diet and regular exercise can significantly lower the risk of vascular problems. Avoiding smoking and excessive alcohol consumption also plays a vital role.
Risk Factor Management
Effectively managing risk factors is a cornerstone in preventing arteriovenous fistula. Key aspects include:
- Regular Health Check-ups: Routine medical check-ups can help in early detection and management of conditions that might lead to arteriovenous fistula.
- Medication Adherence: For those already diagnosed with conditions like hypertension or diabetes, adhering to prescribed medication regimes is vital.
- Education and Awareness: Being informed about the condition and its risk factors empowers individuals to take charge of their health.
The Importance of Regular Check-Ups
Regular check-ups play a pivotal role in the early detection and management of arteriovenous fistula. These check-ups can:
- Identify early signs of vascular problems.
- Help monitor and manage existing health conditions that could lead to arteriovenous fistula.
- Provide an opportunity for healthcare providers to offer personalized advice on lifestyle modifications and risk factor management.
However, a proactive approach combining lifestyle changes, risk factor management, and regular health check-ups is instrumental in preventing and reducing the risk of arteriovenous fistula. It’s a journey of consistent care and awareness, ensuring a healthier vascular system.
FAQs About Arteriovenous Fistula and Its Treatment
What is an Arteriovenous Fistula?
An arteriovenous fistula (AVF) is an abnormal connection between an artery and a vein. Normally, blood flows from your arteries to your capillaries and then to your veins. In an AVF, blood flows directly from an artery into a vein, bypassing some capillaries.
How is an Arteriovenous Fistula Caused?
AVFs can be congenital, meaning they are present at birth, or they can develop after birth. They are often caused by injury or surgery, but can also result from certain medical conditions.
What are the Symptoms of an Arteriovenous Fistula?
Symptoms of an arteriovenous fistula can include swelling, a pulsating lump, and a whooshing sound in the ears. The severity of symptoms typically depends on the size and location of the AVF.
How is an Arteriovenous Fistula Diagnosed?
Diagnosis of an AVF typically involves a physical examination, along with imaging tests such as ultrasound, CT scans, or MRI to confirm the diagnosis and assess the AVF’s size and location.
What are the Treatment Options for Arteriovenous Fistula?
Treatment depends on the size, location, and severity of the AVF. Options may include monitoring, compression therapy, embolization (blocking the fistula), or surgery.
Can Arteriovenous Fistulas Be Prevented?
While congenital AVFs can’t be prevented, you can reduce your risk of acquired AVFs by avoiding injuries and by managing underlying conditions that may contribute to their formation.
When Should I See a Doctor for an Arteriovenous Fistula?
You should see a doctor if you notice symptoms like swelling, a pulsating lump, or a whooshing sound in your ears. Early diagnosis and treatment are crucial for preventing complications.
Conclusion
In summing up, the early diagnosis and effective treatment of Arteriovenous Fistula (AVF) cannot be overstated. Recognizing the initial signs and seeking timely medical intervention are crucial steps in managing this condition. Early detection not only enhances the chances of successful treatment but also significantly reduces the risk of complications associated with AVF.